Abstract
Purpose
Conflicting reports exist regarding the surgical indications, timing, approach, staged or not operation, and spinal instrumentation for patients with spondylodiscitis. Therefore, we performed this study to evaluate the outcome of a series of patients with spondylodiscitis aiming to answer when and how to operate on these patients.
Materials and methods
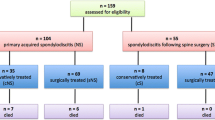
We retrospectively studied the files of 153 patients with spondylodiscitis treated at our institution from 2002 to 2012. The approach included MR imaging of the infected spine, isolation of the pathogen with blood cultures and/or biopsy, and further conservative or surgical treatment. The mean follow-up was 6 years (range 1–13 years). We evaluated the indications, timing (when), and methods (how) for surgical treatment, and the clinical outcome of these patients.
Results
Orthopedic surgical treatment was necessary for 13 of the 153 patients (8.5 %). These were patients with low access to healthcare systems because of low socioeconomic status, third-country migrants, prisoners or intravenous drug use, patients in whom a bacterial isolate documentation was necessary, and patients with previous spinal operations. The most common pathogen was Mycobacterium tuberculosis. The surgical indications included deterioration of the neurological status (11 patients), need for bacterial isolate (10 patients), septicemia due to no response to antibiotics (five patients), and/or spinal instability (three patients). An anterior vertebral approach was more commonly used. Nine of the 13 patients had spinal instrumentation in the same setting. Improvement or recovery of the neurological status was observed postoperatively in all patients with preoperative neurological deficits. Postoperatively, two patients deceased from pulmonary infection and septicemia, and heart infarction. At the last follow-up, patients who were alive were asymptomatic; ten patients were neurologically intact, and one patient experienced paraparesis. Imaging showed spinal fusion, without evidence of recurrent spondylodiscitis. Complications related to the spinal instrumentation were not observed in the respective patients.
Conclusions
Conservative treatment is the standard for spondylodiscitis. Physicians should be alert for Mycobacterium tuberculosis spondylitis because of the low access to healthcare systems of patients with low social and economic status. Surgical indications include obtaining tissue sample for diagnosis, occurrence or progression of neurological symptoms, failure of conservative treatment, large anterior abscesses, and very extensive disease. Thorough debridement of infected tissue and spinal stability is paramount. The anterior approach provides direct access and improved exposure to the most commonly affected part of the spine. Spinal instrumentation is generally recommended for optimum spinal stability and fusion, without any implant-related complications.



Similar content being viewed by others
References
Lee KY (2014) Comparison of pyogenic spondylitis and tuberculous spondylitis. Asian Spine J 8(2):216–223
Grammatico L, Baron S, Rusch E, Lepage B, Surer N, Desenclos JC, Besnier JM (2008) Epidemiology of vertebral osteomyelitis (VO) in France: analysis of hospital-discharge data 2002–2003. Epidemiol Infect 136:653–660
Krogsgaard MR, Wagn P, Bengtsson J (1998) Epidemiology of acute vertebral osteomyelitis in Denmark: 137 cases in Denmark 1978–1982, compared to cases reported to the National Patient Register 1991–1993. Acta Orthop Scand 69:513–517
Colmenero JD, Jiménez-Mejías ME, Sánchez-Lora FJ, Reguera JM, Palomino-Nicás J, Martos F, García de las Heras J, Pachón J (1997) Pyogenic, tuberculous, and brucellar vertebral osteomyelitis: a descriptive and comparative study of 219 cases. Ann Rheum Dis 56:709–715
Sakkas LI, Davas EM, Kapsalaki E, Boulbou M, Makaritsis K, Alexiou I, Tsikrikas T, Stathakis N (2009) Hematogenous spinal infection in central Greece. Spine (Phila Pa 1976) 34:E513-518
Pappas G, Akritidis N, Bosilkovski M, Tsianos E (2005) Brucellosis. N Engl J Med 352:2325–2336
Turunc T, Demiroglu YZ, Uncu H, Colakoglu S, Arslan H (2007) A comparative analysis of tuberculous, brucellar and pyogenic spontaneous spondylodiscitis patients. J Infect 55:158–163
Tuli SM (2007) Tuberculosis of the spine: a historical review. Clin Orthop Relat Res 460:29–38
Rezai AR, Woo HH, Errico TJ, Cooper PR (1999) Contemporary management of spinal osteomyelitis. Neurosurgery 44:1018–1026
Quinones-Hinojosa Jun P, Jacobs R, Rosenberg WS, Weinstein PR (2004) General principles in the medical and surgical management of spinal infections: a multidisciplinary approach. Neurosurg Focus 17(6):E1
Hsieh PC, Wienecke RJ, O’Shaughnessy BA, Koski TR, Ondra SL (2004) Surgical strategies for vertebral osteomyelitis and epidural abscess. Neurosurg Focus 17:E4
Chen WH, Jiang LS, Dai LY (2007) Surgical treatment of pyogenic vertebral osteomyelitis with spinal instrumentation. Eur Spine J 16:1307–1316
Hee HT, Majd ME, Holt RT, Pienkowski D (2002) Better treatment of vertebral osteomyelitis using posterior stabilization and titanium mesh cages. J Spinal Disord Tech 15:149–156
Darouiche RO (2006) Spinal epidural abscess. N Engl J Med 355:2012–2020
Guerado E, Cerván AM (2012) Surgical treatment of spondylodiscitis. An update. Int Orthop 36:413–420
Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ (2000) Hematogenous pyogenic spinal infections and their surgical management. Spine (Phila Pa 1976) 25:1668-1679
Babouee Flury B, Elzi L, Kolbe M, Frei R, Weisser M, Schären S, Widmer AF, Battegay M (2014) Is switching to an oral antibiotic regimen safe after 2 weeks of intravenous treatment for primary bacterial vertebral osteomyelitis? BMC Infect Dis 14:226
Legrand E, Flipo RM, Guggenbuhl P, Masson C, Maillefert JF, Soubrier M, Noël E, Saraux A, Di Fazano CS, Sibilia J, Goupille P, Chevalie X, Cantagrel A, Conrozier T, Ravaud P, Lioté F, Organization Rheumatology Network (2001) Management of nontuberculous infectious discitis. Treatments used in 110 patients admitted to 12 teaching hospitals in France. Joint Bone Spine 68:504–509
McHenry MC, Easley KA, Locker GA (2002) Vertebral osteomyelitis: long-term outcome for 253 patients from 7 Cleveland-area hospitals. Clin Infect Dis 34:1342–1350
Musher DM, Thorsteinsson SB, Minuth JN et al (1976) Vertebral osteomyelitis. Still a diagnostic pitfall. Arch Intern Med 136:105–110
Kaya S, Ercan S, Kaya S, Aktas U, Kamasak K, Ozalp H, Cinar K, Duymus R, Boyaci MG, Akkoyun N, Eskazan AE, Temiz H (2014) Spondylodiscitis: evaluation of patients in a tertiary hospital. J Infect Dev Ctries 8:1272–1276
Kowalski TJ, Berbari EF, Huddleston PM, Steckelberg JM, Osmon DR (2006) Do follow-up imaging examinations provide useful prognostic information in patients with spine infection? Clin Infect Dis 43:172–179
Eismont FJ, Bohlman HH, Soni PL, Goldberg VM, Freehafer AA (1983) Pyogenic and fungal vertebral osteomyelitis with paralysis. J Bone Joint Surg Am 65:19–29
Liebergall M, Chaimsky G, Lowe J, Robin GC, Floman Y (1991) Pyogenic vertebral osteomyelitis with paralysis. Prognosis and treatment. Clin Orthop Relat Res 269:142–150
Euba G, Narváez JA, Nolla JM, Murillo O, Narváez J, Gómez-Vaquero C, Ariza J (2008) Long-term clinical and radiological magnetic resonance imaging outcome of abscess-associated spontaneous pyogenic vertebral osteomyelitis under conservative management. Semin Arthritis Rheum 38:28–40
Siddiq F, Chowfin A, Tight R, Sahmoun AE, Smego RA Jr (2004) Medical vs surgical management of spinal epidural abscess. Arch Intern Med 164:2409–2412
Reihsaus E, Waldbaur H, Seeling W (2000) Spinal epidural abscess, a meta analysis of 915 patients. Neurosurg Rev 23:175–204
Jeong SJ, Choi SW, Youm JY, Kim HW, Ha HG, Yi JS (2014) Microbiology and epidemiology of infectious spinal disease. J Korean Neurosurg Soc 56:21–27
Carragee EJ (1997) Pyogenic vertebral osteomyelitis. J Bone Joint Surg Am 79:874–880
Patzakis MJ, Rao S, Wilkins J, Moore TM, Harvey PJ (1991) Analysis of 61 cases of vertebral osteomyelitis. Clin Orthop Relat Res 264:178–183
Weinstein MA, Eismont FJ (2005) Infections of the spine in patients with human immunodeficiency virus. J Bone Joint Surg Am 87:604–609
Rankine JJ, Barron DA, Robinson P, Millner PA, Dickson RA (2004) Therapeutic impact of percutaneous spinal biopsy in spinal infection. Postgrad Med J 80:607–609
Dufour V, Feydy A, Rillardon L, Redondo A, Le Page L, Bert F, Belmatoug N, Fantin B (2005) Comparative study of postoperative and spontaneous pyogenic spondylodiscitis. Semin Arthritis Rheum 34:766–771
Hadjipavlou AG, Katonis PK, Gaitanis IN, Muffoletto AJ, Tzermiadianos MN, Crow W (2004) Percutaneous transpedicular discectomy and drainage in pyogenic spondylodiscitis. Eur Spine J 13:707–713
Yang SC, Fu TS, Chen LH, Niu CC, Lai PL, Chen WJ (2007) Percutaneous endoscopic discectomy and drainage for infectious spondylitis. Int Orthop 31(3):367–373
Ito M, Abumi K, Kotani Y, Kadoya K, Minami A (2007) Clinical outcome of posterolateral endoscopic surgery for pyogenic spondylodiscitis: results of 15 patients with serious comorbid conditions. Spine 32:200–206
Lee BH, Lee HM, Kim TH, Kim HS, Moon ES, Park JO, Chong HS, Moon SH (2012) Transpedicular curettage and drainage of infective lumbar spondylodiscitis: technique and clinical results. Clin Orthop Surg 4:200–208
Rath SA, Neff U, Schneider O, Richter HP (1996) Neurosurgical management of thoracic and lumbar vertebral osteomyelitis and discitis in adults: a review of 43 consecutive surgically treated patients. Neurosurgery 38:926–933
Korovessis P, Petsinis G, Koureas G, Iliopoulos P, Zacharatos S (2006) One-stage combined surgery with mesh cages for treatment of septic spondylitis. Clin Orthop Relat Res 444:51–59
Fukuta S, Miyamoto K, Masuda T, Hosoe H, Kodama H, Nishimoto H, Sakaeda H, Shimizu K (2003) Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine (Phila Pa 1976) 28:E302-308
Karadimas EJ, Bunger C, Lindblad BE, Hansen ES, Høy K, Helmig P, Kannerup AS, Niedermann B (2008) Spondylodiscitis. A retrospective study of 163 patients. Acta Orthop 79:650–659
Carragee E, Iezza A (2008) Does acute placement of instrumentation in the treatment of vertebral osteomyelitis predispose to recurrent infection: long-term follow-up in immune-suppressed patients? Spine (Phila Pa 1976) 33:2089-2093
Sundararaj GD, Amritanand R, Venkatesh K, Arockiaraj J (2011) The use of titanium mesh cages in the reconstruction of anterior column defects in active spinal infections: can we rest the crest? Asian Spine J 5:155–161
Korres DS, Papagelopoulos PJ, Zahos KA, Kolia MD, Poulakou GG, Falagas ME (2007) Multifocal spinal and extra-spinal Mycobacterium chelonae osteomyelitis in a renal transplant recipient. Transpl Infect Dis 9(1):62–65
Miksić NG (2013) Spinal infections with and without hardware: the viewpoint of an infectious disease specialist. Eur J Orthop Surg Traumatol 23(Suppl 1):S21–S28
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No benefits have been or will be received from a commercial party related directly or indirectly to the subject matter of this article. All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Mavrogenis, A.F., Igoumenou, V., Tsiavos, K. et al. When and how to operate on spondylodiscitis: a report of 13 patients. Eur J Orthop Surg Traumatol 26, 31–40 (2016). https://doi.org/10.1007/s00590-015-1674-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-015-1674-6