Abstract
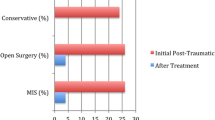
Spinal fractures are commonly encountered in ankylosing spondylitis (AS) patients. This study compares the outcome of early surgical treatment with initial conservative treatment for thoracolumbar fractures in patients with AS. From 1996 to 2008, 28 patients with AS were treated either operatively or conservatively for thoracolumbar fractures; however, only 25 patients met the inclusion criteria with a minimum follow-up of 2 years. For surgically treated patients, posterior spinal instrumentation was performed using a transpedicle screw system. Nonsurgically treated patients wore a fracture brace. The demographic data, diagnosis, mechanism of injury, and neurological status were recorded, and fracture healing was assessed radiographically. The mean age was 54.2 ± 13.8 years (range 30–80 years). Six patients (Group A) received surgical intervention within 1 month. All of these fractures healed, and two of five patients showed neurologic improvement after surgery. Eight patients (Group B) had fractures that were missed. The delay in diagnosis resulted in pseudoarthrosis in all cases, and progressive neurologic deficits were identified in four cases. Eleven patients (Group C) received conservative treatment with bracing. Fracture union was achieved in three cases, and pseudoarthrosis occurred in eight cases. Operative treatment can achieve solid fusion and improve the neurological status, while conservative treatment may result in pseudoarthrosis and progressive neurologic deficit. The results suggest that AS patients with unstable spinal fractures should receive early surgical management to prevent further sequelae.



Similar content being viewed by others
References
Donnelly S, Doyle DV, Denton A, Rolfe I, McCloskey EV, Spector TD (1994) Bone mineral density and vertebral compression fracture rates in ankylosing spondylitis. Ann Rheum Dis 53(2):117–121
Cooper C, Carbone L, Michet CJ, Atkinson EJ, O’Fallon WM, Melton LJ 3rd (1994) Fracture risk in patients with ankylosing spondylitis: a population based study. J Rheumatol 21(10):1877–1882
Hunter T, Dubo H (1978) Spinal fractures complicating ankylosing spondylitis. Ann Intern Med 88(4):546–549
Hunter T, Dubo HI (1983) Spinal fractures complicating ankylosing spondylitis. A long-term followup study. Arthritis Rheum 26(6):751–759
Chaudhary SB, Hullinger H, Vives MJ (2011) Management of acute spinal fractures in ankylosing spondylitis. ISRN Rheumatol 2011:Article ID 150484. doi:10.5402/2011/150484
Anwar F, Al-Khayer A, Joseph G, Fraser MH, Jigajinni MV, Allan DB (2011) Delayed presentation and diagnosis of cervical spine injuries in long-standing ankylosing spondylitis. Eur Spine J 20(3):403–407. doi:10.1007/s00586-010-1628-y
Hosssain M, McLean A, Fraser MH (2004) Outcome of halo immobilisation of 104 cases of cervical spine injury. Scott Med J 49(3):90–92
Farrokhi MR, Motallebi H (2007) Outcome of surgical and nonsurgical methods in the treatment of unstable traumatic lesions of the lower cervical spine. Arch Iran Med 10(2):157–160
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L (2007) Fracture and dislocation classification compendium-2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 21(10 Suppl):S1–133
Jacobs WB, Fehlings MG (2008) Ankylosing spondylitis and spinal cord injury: origin, incidence, management, and avoidance. Neurosurg Focus 24(1):E12. doi:10.3171/FOC/2008/24/1/E12
Caron T, Bransford R, Nguyen Q, Agel J, Chapman J, Bellabarba C (2010) Spine fractures in patients with ankylosing spinal disorders. Spine 35(11):E458–464. doi:10.1097/BRS.0b013e3181cc764f (Phila Pa 1976)
Sapkas G, Kateros K, Papadakis SA, Galanakos S, Brilakis E, Machairas G, Katonis P (2009) Surgical outcome after spinal fractures in patients with ankylosing spondylitis. BMC Musculoskelet Disord 10:96. doi:10.1186/1471-2474-10-96
Hitchon PW, From AM, Brenton MD, Glaser JA, Torner JC (2002) Fractures of the thoracolumbar spine complicating ankylosing spondylitis. J Neurosurg 97(2 Suppl):218–222
Westerveld LA, Verlaan JJ, Oner FC (2009) Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J 18(2):145–156. doi:10.1007/s00586-008-0764-0
Feltelius N, Hedenstrom H, Hillerdal G, Hallgren R (1986) Pulmonary involvement in ankylosing spondylitis. Ann Rheum Dis 45(9):736–740
Momeni M, Taylor N, Tehrani M (2011) Cardiopulmonary manifestations of ankylosing spondylitis. Int J Rheumatol 2011:Article ID 728471. doi:10.1155/2011/728471
Fox MW, Onofrio BM, Kilgore JE (1993) Neurological complications of ankylosing spondylitis. J Neurosurg 78(6):871–878. doi:10.3171/jns.1993.78.6.0871
Author information
Authors and Affiliations
Corresponding author
Additional information
Meng-Ling Lu and Tsung-Ting Tsai have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lu, ML., Tsai, TT., Lai, PL. et al. A retrospective study of treating thoracolumbar spine fractures in ankylosing spondylitis. Eur J Orthop Surg Traumatol 24 (Suppl 1), 117–123 (2014). https://doi.org/10.1007/s00590-013-1375-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-013-1375-y