Abstract
Introduction
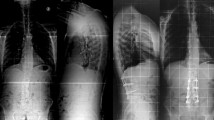
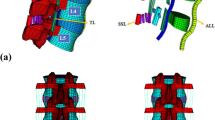
The sagittal plane of body produces a convex curve anteriorly referred to as the lordotic curve. Malalignment of lordotic curve leads to low back disorders and lumbar spinal surgery has been known to cause this. This study was a retrospective analysis of the effects of posterior lumbar interbody fusion using cages on segmental lumbar lordosis.
Materials and methods
We conducted a retrospective study involving 27 patients of which 16 were females and 11 were males. All patients underwent single level posterior lumbar interbody fusion with insertion of non-wedged intervertebral cage and pedicle screw fixation. Intraoperatively, all patients had a change from knee chest position to prone to augment their lumbar lordosis. The minimum follow up was 2 years and fusion was achieved in 21 patients.
Results
Segmental lordotic angles increased from 15.2° to 20.6° at L4/5 level and from 17.8° to 24.5° at L5/S1 level, preoperative to postoperative, respectively (P < 0.01 at both levels).
Conclusion
Thus apparently, posterior lumbar interbody fusion with insertion of non-wedged intervertebral cage and pedicle screw fixation results in creation and maintenance of lumbar lordosis.
Résumé
Introduction
Le plan sagittal des corps vertébraux produit une courbe convexe vers l’avant référée comme étant la lordose lombaire. Le mal alignement de cette lordose entraîne des désordres du bas du dos et la chirurgie lombaire est censée créer ces désordres. Cette étude est une analyse rétrospective des effets de l’arthrodèse intersomatique lombaire avec cages placées par voie postérieure sur la lordose segmentaire lombaire.
Matériels et méthode
Nous avons fait cette étude rétrospective chez 27 patients, soit 16 femmes et 11 hommes. Tous les patients furent opérés par pose de cages intersomatiques non cunéiformes à un seul niveau, associée à une ostéosynthèse avec vissage pédiculaire. Pendant l’intervention tous les patients ont été déplacés de la position genu-pectorale au procubitus afin d’augmenter leur lordose lombaire. Le recul moyen a été de deux ans et la fusion a été considérée comme atteinte chez 21 patients.
Résultats
Les angles de lordose lombaire segmentaire ont augmenté de 15.2° à 20.6° en L4/5 et de 17.8° à 24.5° en L5/S1 entre la mensuration pré-opératoire et la post-opératoire (P < 0.01 aux deux niveaux).
Conclusion
On peut en déduire qu’apparemment l’arthrodèse intersomatique par voie postérieure avec insertion de cages non cunéiformes et fixation par vissage pédiculaire crée et maintient la lordose lombaire.





Similar content being viewed by others
References
Benfanti PL, Geissele AE (1997) The effect of intraoperative hip position on maintenance of lumbar lordosis: a radiographic study of anesthetized patients and unanesthetized volunteers on the Wilson frame. Spine 22:2299–2303
Bernhardt M, Bridwell KH (1989) Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine 14:717–721
Burton CV, Cassidy JD (1992) Economics, epidemiology and risk factors. In: Kirkaldywillis WH, Burton CV (eds) Managing low back pain, 3rd edn. Churchill Livingstone, New York, pp 1–6
Diedrich O, Perlick L, Schmitt O, Kraft CN (2001) Radiographic spinal profile changes induced by cage design after posterior lumbar interbody fusion: preliminary report of a study with wedged implants. Spine 26(12):274–280
Gelb DE, Lenke LG, Bridwell KH, Blanke K, Mc Enery KW (1995) An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine 10:1351–1358
Godde S, Fritsch E, Dienst M, Kohn D (2003) Influence of cage geometry on sagittal alignment in instrumented posterior lumbar interbody fusion. Spine 28(15):1693–1699
Goldstein JA, Macenski MJ, Griffith SL, McAfee PC (2001) Lumbar sagittal alignment after fusion with a threaded interbody cage. Spine 26(10):1137–1142
Guanciale AF, Dinsay JM, Watkins RG (1996) Lumbar lordosis in spinal fusion: a comparison of intraoperative results of patient positioning on two different operative frame types. Spine 21:964–969
Hacker RJ (1997) Comparison of interbody fusion approaches for disabling low back pain. Spine 22:660–666
Jackson RP, McManus AC (1994) Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size: a prospective controlled clinical study. Spine 19:1611–1618
Klemme WR, Owens BD, Dhawan A, Zeidman S, Polly DW Jr (2001) Lumbar sagittal contour after posterior interbody fusion: threaded devices alone versus vertical cages plus posterior instrumentation. Spine 26(5):534–537
Korovessis P, Stamatakis M, Baikousis A (1999) Segmental roentgenographic analysis of vertebral inclination on sagittal plane in asymptomatic versus chronic low back pain patients. J Spinal Disord 12:131–137
Kuslich SD, Ulstrom CL, Griffith SL, Ahern JA, Dowdle JD (1998) The Bagby and Kuslich method of lumbar interbody fusion: history, techniques, and 2-year follow-up results of a United States prospective, multicenter trial. Spine 23:1267–1279
La Grone MO, Bradford DS, Moe JH, Lonstein JE, Winter RB, Ogilvie JW (1988) Treatment of symptomatic flatback after spinal fusion. J Bone Joint Surg 70:569–580
Lord MJ, Small JM, Dinsay JM, Watkins RG (1997) Lumbar lordosis effects of sitting and standing. Spine 22:2571–2574
Ray CD (1997) Threaded titanium cages for lumbar interbody fusions. Spine 22:667–680
Stephens GC, Yoo JU, Wilbur G (1996) Comparison of lumbar sagittal alignment produced by different operative positions. Spine 21:1802–1806
Tann SB, Kozak JA, Dickson JH, Nalty TH (1994) Effect of operative position on sagittal alignment of the lumbar spine. Spine 3:314–318
Tribus CB, Belanger TA, Zdeblick TA (1999) The effect of operative position and short-segment fusion on maintenance of sagittal alignment of the lumbar spine. Spine 24:58–61
Troyanovich SJ, Caillet R, Janik TJ, Harrison DD, Harrison DE (1997) Radiographic mensuration characteristics of the sagittal lumber spine from a normal population with a method to synthesize prior studies of lordosis. J Spinal Disord 10:380–386
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kakkar, R., Sirigiri, P.B.R., Howieson, A. et al. Posterior lumbar interbody fusion and segmental lumbar lordosis. Eur J Orthop Surg Traumatol 17, 125–129 (2007). https://doi.org/10.1007/s00590-006-0137-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-006-0137-5