Abstract
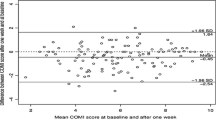
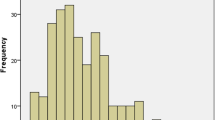
The aim of this study was to determine inter- and intraobserver agreement between spine surgeons and orthopedic radiologists in recognizing distinct degenerative pathology on plain lumbosacral roentgenograms; to estimate the validity (sensitivity and specificity) to make a surgical decision by correlating Short form-36 Health Survey (SF-36) scores and roentgenographic degenerative pathology; and to determine the intra- and interobserver agreement between radiologists, surgeons, and authors in making a surgical decision for treatment on the basis of distinct roentgenographic pathology, SF-36 scores, clinical findings derived from physical examination, or combined. The authors followed three routes to objectively assess the reliability and validity of the surgical decision in chronic low back pain patients: First, 100 consecutive male patients who suffered from low back pain were examined by the authors physically, using imaging techniques (including plain roentgenograms, CT-scan, or/and MRI), and SF-36 survey. Two senior orthopedic radiologists and two senior spine surgeons were asked to read blinded a set of 100 roentgenograms of the lumbar spine in two sessions. Second, surgeons and radiologists were asked to make a surgical decision in each particular patient using either SF-36 scores or plain roentgenograms or matched SF-36 data and roentgenograms, and these decisions were compared with each other as well as with the authors’ decision, which was based on combined imaging (roentgenograms, CT, MRI), SF-36 scores, and surgical findings. The intra- and interobserver reliability on recognizing distinct pathological findings on plain roentgenograms was expressed in terms of kappa, and the validity of the approach that was used by the authors in the present study to calculate the proportion of normal and abnormal roentgenograms, which are likewise “diagnosed” by the level of SF-36 scores shown in terms of sensitivity, specificity, and positive and negative predictive value. The impact of subjectivity in making a surgical decision was tested by randomly asking half of the patients to magnify and the other half to undermagnify their SF-36 data. The prevalence of roentgenographic pathology detected by radiologists, surgeons, and authors was 0.51, 0.53, and 0.54 respectively, while in only 28% of the patients the authors posed the indication for surgery. The interobserver agreement in detecting roentgenographic pathology in the first and second session was for radiologists 0.79 and 0.88 respectively, and 0.81 and 0.91 for surgeons respectively. The average intraobserver agreement in detecting pathology on plain lumbosacral roentgenograms was 0.92 and 0.91 for radiologists and surgeons respectively. The sensitivity and specificity of the method to calculate the surgeons’ proportions of normal and abnormal roentgenograms, which are likewise “diagnosed” by the level of SF-36 scores, was 0.49 and 0.36 respectively. When this calculation was made by radiologists, the sensitivity and specificity was 0.47 and 0.35 respectively. The positive predictive value was 0.38 for both radiologists and surgeons. The consensus between independent radiologist to make a surgical decision using only roentgenographic data was 0. 71 while between spine surgeons based on SF-36 data it was 0.83. The consensus between spine surgeons (decision based on SF-36 data) and orthopedic radiologists (decision based on radiology) was 0.41. In surgical decisions made by spine surgeons using matched SF-36, roentgenographic, and surgical examination data, the consensus raised to 0.67. The consensus between spine surgeons making a surgical decision using matched roentgenographic, SF-36, and surgical examination was 0.58 The impact of subjectivity that was tested when randomly half of the patients were asked to magnify or undermagnify their SF-36 data erroneously increased the sensitivity to 0.54 and 0.59 respectively. This investigation showed that distinct degenerative lumbar spinal pathology can be identified on plain roentgenographs with similarly high accuracy by orthopedic, radiologists, and spine surgeons. The sensitivity and specificity of recognizing abnormal and normal roentgenograms using normal and abnormal SF-36 data was low because of the subjective nature of the SF-36 survey. This study additionally concluded that any surgical decision should not be taken on the basis of any roentgenographic pathology or on what the patient says in the SF-36 questionnaire, but on the basis of matched SF-36 scores, roentgenographic and imaging evaluation, and physical examination data.
Résumé
Le but de ce travail est de déterminer le consensus inter- et intra-observateurs entre les chirurgiens du rachis et les radiologues spécialisés en ostéo-articulaire pour le diagnostic positif de la pathologie dégénérative sur des radiographies standards lombo-sacrées, d’estimer la validité (sensibilité et spécificité) pour poser une indication chirurgicale en corrélant les scores SF-36, les signes dégénératifs radiologiques et les données cliniques. Les voies suivantes ont été suivies par les auteurs pour atteindre ce but. Cent patients lombalgiques masculins consécutifs ont été examinés cliniquement en incluant l’imagerie médicale (radiographies standards, scanner et/ou IRM) et le score SF-36. Deux radiologues ostéo-articulaires seniors et deux chirurgiens du rachis seniors ont été priés d’examiner en double aveugle 100 radiographies du rachis lombaire en deux sessions. Des chirurgiens et des radiologistes ont été priés de poser une indication chirurgicale dans chaque cas particulier en utilisant soit le score SF-36, soit les radiographies standards, soit la combinaison du score SF-36 et des radiographies et ces décisions chirurgicales furent comparées les unes avec les autres aussi bien qu’avec celles des auteurs, basées sur l’ensemble des données d’imagerie, de score SF-36 et sur les constatations opératoires. L’impact de la subjectivité dans la décision chirurgicale fut testé par randomisation pour moitié avec les données du patient, pour l’autre moitié en magnifiant les données du score SF-36. En conclusion, les auteurs ont observé que la pathologie dégénérative lombaire est estimée pareillement sur des radiographies standards aussi bien par les orthopédistes, que les radiologistes et les chirurgiens du rachis. La sensibilité et la spécificité pour reconnaître le normal et l’anormal sur des radiographies étaient basses à cause du caractère spécifique du score SF-36. Cette étude a montré de plus qu’aucune décision chirurgicale n’est à poser sur les seuls radiographies ou sur les seules signes subjectifs décrits par les patients dans le questionnaire SF-36, mais sur une combinaison du score SF-36, des radiographies, de l’imagerie et des données de l’examen clinique.
Similar content being viewed by others
References
Altman GA (ed) (1991) Practical statistics for medical research, first edn. Chapman and Hall, London
Baker JG, Fiedler RC, Ottenbacher KJ, Czyrny JJ, Heinemann AW (1998) Predicting follow-up functional outcomes in outpatient rehabilitation. Am J Phys Med Rehabil 77:202–212
Bernhardt M, Bridwell KH (1998) Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine 14:717–721
Deyo RA (1986) Early diagnostic evaluation of low back pain. J Gen Intern Med 1:328–338
Epstein EN, Hood CD, Bender JF (1997) A comparison of surgeon’s assessment to patient’s self analysis (Short form 36) after far lateral lumbar disc surgery. Spine 22:2422–2428
Frymoyer JW, Phillips RB, Newberg AH, et al (1986) A comparative analysis of the interpretations of lumbar spinal radiographs by chiropractors and medical doctors. Spine 11:1020–1023
Gatchel JR, Mayer T, Dersh J, Robinson R, Polatin P.(1999) The association of the SF-36 health status survey with 1-year socioeconomic outcomes in a chronically disabled spinal disorder population. Spine 24:2126–2170
Jackson RP, McManus AC (1994) Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex and size: A prospective controlled clinical study. Spine 14:1611–1618
Jensen MC, Brandt-Zawaddzki MN, Obuchowski N, Modic MT, Malkasia D, Ross JS (1995) Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 331:69–73
Korovessis P, Baikousis A, Stamatakis M (1998) Reciprocal angulation of vertebral bodies in sagittal plane in an asymptomatic Greek population. Spine 23:700–705
Korovessis P, Stamatkis M, Baikousis A (1999) Segmental roentgenographic analysis of vertebral inclination on sagittal plane in asymptomatic versus chronic low back pain patients J Spin Disord 12(2):131–137
Korovessis P, Dimas A, Lambiris E (2002) Correlative analysis of lateral vertebral radiographic variables and medical outcomes study short-form health status. J Spinal Disord Tech 15:384–390
McDermott W (1981) Absence of indicators of the influence of its physicians on a society’s health. Am J Med 70:833–842
McHorney CA, Ware JE, Raczek AE (1993) The MOS 36 item Short Form Health Survey (SF-36): II: Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31:247–263
McHorney CA, Ware JE, Lu JF, Sherbourne CD (1994) The MOS 36 Short Form Health Survey (SF-36): III: Tests of data quality, scaling assumptions and reliability across diverse patient groups. Medical Care 32:40–66
Merskey EH, Spear FG (1997) The concept of pain. J Pshychosomatic Res 11:59–67
Nachemson A (1975) Towards a better understanding of low-back pain: a review of the mechanics of the lumbar disc. Rheumatol Rehab 14:129–143
Philips RC, Lansky DJ (1992)Outcomes management in heart valve replacement surgery: Early experience. J Heart Valve Dis 1:42–50
Reading AE (19980) A comparison of pain rating scales. J Phychosomatic Res 24:119–124
Schroeder SA (1987) Outcome assessment 70 years later: are we ready? N Engl J Med 316:180–189
Steart LA, Hays DR, Ware EJ (1988) The MOS Short Form General Health Survey. Medical Care 26:724–735
Vingard E, Alfredsson L, Hagberg M et al (2000) To what extent do current and past physical and psychosocial occupational factors explain care-seeking for low-back pain in a working population? Spine 25:493–500
Ware JE Jr, Sherbourne CD (1992) The MOS 36 Item Short-Form Health Survey (SF-36): Conceptual framework and item selection. Med Care 30:473–483
Ware JE, Snow KK, Kosinski M, Gandek B (1993) SF-36 Health Survey: Manual and interpretation guide, The Health Institute, New England Medical Center, Boston
Woodforde JM, Merskey EH (1972) Some relationships between subjective measures of pain. J Psychosomatic Res 16:173–178
Acknowledgement
The authors wish to express their appreciation to Giorgos Korovessis, Institute of Science, University of Ioannina, Greece, for his assistance in making statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Korovessis, P., Dimas, A., Koureas, G. et al. Correlative analysis of reliability and validity of plain radiology, MOS short-form health survey and surgical examination in making decision for treatment of chronic low back pain patients. Eur J Orthop Surg Traumatol 14, 135–141 (2004). https://doi.org/10.1007/s00590-004-0164-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-004-0164-z