Abstract
Objective
The aim of this study was to explore the correlation between PI and standing-to-sitting changes of the sagittal alignment in patients with lumbar degenerative diseases, and investigate the differences in posture changes among Roussouly types.
Methods
A total of 209 patients with lumbar degenerative disease were retrospectively included in this study. All the patients received lateral full body imaging in both standing and sitting positions. Sagittal parameters including SVA, OD-HA, PT, PI, PT/PI, SS, LL, TK, Upper LL (L1-L4) and Lower LL (L4-S1) were measured in both standing and sitting position, and the parameters were compared between two positions. The correlations between PI and lumbo-pelvic changes were analyzed. The postural changes were compared among different Roussouly types.
Results
From standing to sitting, all the parameters except PI significantly changed, including SVA, OD-HA, PT, PT/PI, SS, LL, TK, Upper LL and Lower LL. The contribution of lower LL was greater to global LL than upper LL. PI had a significant correlation with ΔPT, ΔSS, ΔLL, ΔUpper LL and ΔLower LL. From standing to sitting, type 4 patients had the most pronounced ΔPT, ΔSS and ΔLL, and ΔLower LL of types 3 and 4 were greater than that of types 1 and 2.
Conclusions
In patients with degenerative disease, PI plays an important role in determining the extent of lumbo-pelvic changes from standing to sitting. Among different Roussouly types, type 4 patients have the most pronounced changes of PT, SS and LL, suggesting the relatively greater flexibility of pelvis and lumbar spine.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sitting is a common position in modern life and work. Office workers spend more than 70% of their working time in sitting position [1]. Previous study has shown that the spinal-pelvic sagittal alignment in sitting position is quite different from that in standing position, such as decreased lumbar lordosis (LL) and increased pelvic tilt (PT) [2]. Compared with traditional upright or flexion–extension standing lateral radiographs, sitting lateral radiographs show a better sensitivity in detecting dynamic lumbar instability [3]. It has been reported that patients who have undergone lumbar fusion would have adaptive changes in the region of adjacent segments during sitting position, which may lead to development of adjacent segment diseases [4, 5]. Thus, exploring the spinal-pelvic sagittal parameters of patients with lumbar degenerative diseases in sitting position is of great benefit to provide specific reference for treatment decision making.
Pelvic incidence (PI) is an important spinal-pelvic sagittal parameter in assessing spinal balance, which has a close relationship with several parameters in standing position [6, 7]. In asymptomatic individuals, PI has been shown to impact the magnitude and distribution of LL. Individuals with a higher PI exhibit a more horizontal sacrum and greater LL with a more proximal apex compared to those with a lower PI [8]. Numerous studies have demonstrated that PI remains unchanged from standing to sitting position [2, 9]. Investigating the relationship between PI and the change values of lumbo-pelvic sagittal alignment will engender a better understanding of the postural pelvic compensatory capacity.
Roussouly classification has been widely used to evaluate the spinal-pelvic profile since 2005 [10], which defines four different spinal-pelvic types by the differences in sacral slope (SS) and the apex of the lumbar curve in standing position. For degenerative scoliosis patients, Zhang et al. [11] found that if the postoperative sagittal profile can be restored to match the patient’s own PI value, use of the Roussouly classification can reduce the incidence of postoperative mechanical complications. In healthy subjects, it has been demonstrated that spinal-pelvic alignment changed differently among four types during standing to sitting position [12]. Since Laouissat et al. [13] have proved that mean PI values gradually increase from type 1 to type 4, comparing the postural spinal-pelvic changes between different Roussouly types helps to better understand the role that PI plays in transition of posture.
The aim of this study was to figure out the correlation between PI and changes of spinal-pelvic sagittal alignment from standing to sitting position in patients with lumbar degenerative diseases. Furthmore, we intended to provide a comprehensive interpretation of standing-to-sitting changes in spinal-pelvic sagittal parameters among different Roussouly types.
Methods
We conducted a retrospective study of patients with lumbar degenerative disease who visited our outpatient clinic between September 2018 and September 2023. Patients diagnosed with lumbar degenerative disc disease, lumbar disc herniation, lumbar spinal stenosis, or low-grade lumbar spondylolisthesis (Meyerding’s Grade I or II) were selected. Exclusion criteria were: (1) scoliosis angle on the coronal plane > 20°; (2) thoracolumbar kyphosis deformity > 50°; (3) a history of spinal surgery, trauma, infection, or pelvic/lower limbs fracture. A total of 209 patients (92 men and 117 women) were enrolled and their demographic data were recorded. This study was approved by the ethics committee of our hospital (2021-LCYJ-DBZ-05).
Each patient received lateral full body imaging in both standing and sitting positions, taken by trained radiology technologists using a lower radiation dose of EOS machine (EOS Imaging Inc, Paris, France). Before imaging, patients were required to have a break more than 15 min. When taking standing radiographs, patients were instructed to stand straight, with arms 90° forward, hands holding two bars and elbows extended. When taking sitting radiographs, patients were instructed to flex their hips and knees to 90°, sit straight in a backless metal chair with their feet flat on the ground, arms 90° forward, hands holding two bars and elbows extended.
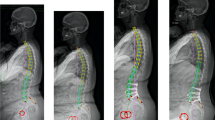
All measurements (Fig. 1) were performed by a spine surgeon using Surgimap Spine software (version: 2.2.12.1, New York, NY, USA). Global parameters were listed below: SVA (C7-sagittal vertical axis), OD-HA (odontoid hip axis, the angle between the vertical and the highest point of the odontoid process connecting to the center of the bi-coxofemoral axis [14]), PI (pelvic incidence), PT (pelvic tilt), SS (sacral slope), TK (T5-T12 thoracic kyphosis) and LL (global lumbar lordosis). Local parameters included upper lumbar lordosis (upper LL), defined as the angle between the superior endplate of L1 and the superior endplate of L4; and lower lumbar lordosis (lower LL), defined as the angle between the superior endplate of L4 and the superior endplate of S1. Each parameter was measured twice, and finally the average value was adopted for further analyses (ICC 0.921 [95% CI 0.870–0.953]). According to Roussouly classification proposed in 2005 [10], patients were divided into four types based on SS and the apex of the lumbar curve in standing position.
Statistical methods
All analyses were performed using SPSS version 24.0 (SPSS, Chicago, IL, USA). Continuous variables were expressed as means ± SDs. We used paired t test to analyze the difference in the same parameter from standing to sitting. Independent sample t test was utilized to compare the upper and lower LL. Correlations between PI and the changes of lumbo-pelvic parameters were analyzed using the Pearson correlation coefficient. The difference in changes of parameters were analyzed by means of one-way ANOVA and LSD t test among different Roussouly types. Histograms and line charts were generated through Prism 9 software (GraphPad Software, San Diego, California, USA). When p value < 0.05, it was considered statistically significant.
Results
General data
A total of 209 patients (92 men and 117 women) were included in this study, with an average age of 53.9 ± 12.7 years. The mean body mass index was 22.7 ± 3.4 kg/m2. There were 98 cases of lumbar spondylolisthesis, 78 cases of lumbar disc herniation and 33 cases of lumbar spinal stenosis. With regards to Roussouly classification, 8 patients were excluded since their SS value did not match the apex of lumbar curve, so that they did not belong to any of the four types. The remaining 201 patients were classified as follows: type 1, 40 patients (19.9%); type 2, 65 patients (32.3%); type 3, 81 patients (40.3%); type 4, 15 patients (7.5%).
Spinal-pelvic sagittal alignment in standing and sitting positions
Table 1 shows spinal-pelvic sagittal alignment in standing and sitting positions. When patients moved from standing to sitting, spinal-pelvic sagittal parameters changed significantly, except PI (49.3º ± 10.6º vs. 49.3º ± 10.3º; p = 0.922). Among global parameters, SVA (9.3 mm ± 34.0 mm vs. 44.3 mm ± 29.9 mm; p < 0.001), OD-HA (−2.0º ± 3.1º vs. −0.3º ± 3.2º; p < 0.001), PT (15.4º ± 7.6º vs. 26.3º ± 11.7º; p < 0.001) and PT/PI (30.5% ± 13.1% vs. 53.0% ± 20.3%; p < 0.001) increased significantly, which indicated that the gravity of the body moved forward and the pelvis had a tendency to retrovert. On the contrary, it was noticed that SS (34.0º ± 8.2º vs. 23.0º ± 10.4º; p < 0.001), LL (45.1º ± 12.8º vs. 27.3º ± 14.4º; p < 0.001) and TK (24.4º ± 9.5º vs. 23.3º ± 9.0º; p = 0.003) had a decreasing trend, implying the global spine straightened out when standing-to-sitting. As to local parameters, upper LL (14.5º ± 9.2º vs. 7.3º ± 10.2º; p < 0.001) and lower LL (30.6º ± 8.8º vs. 20.0º ± 8.7º; p < 0.001) were found to be significantly decreased. As is shown in Table 2, lower LL contributed more to global LL than upper LL, regardless of position (standing: 14.5º ± 9.2º vs. 30.6º ± 8.8º; p < 0.001; sitting: 7.3º ± 10.2º vs. 20.0º ± 8.7º; p < 0.001). Additionally, the postural changes experienced the same result (7.2º ± 6.9º vs. 10.6º ± 7.1º; p < 0.001).
Correlations between standing PI and the lumbo-pelvic changes from standing to sitting
As present in Table 3, PI was found to be correlated significantly with ΔPT, ΔSS, ΔLL, ΔUpper LL and ΔLower LL, which implied that patients with a larger PI would have greater postural changes of sagittal alignment. PI had a negative correlation with ΔPT (r = −0.184; p = 0.008) and a positive correlation with ΔSS (r = 0.222; p = 0.001), indicating progressively greater pelvic rotation and sacral inclination with increasing PI. In addition, PI was positively correlated with ΔLL (r = 0.229; p = 0.001), ΔUpper LL (r = 0.153; p = 0.027) and ΔLower LL (r = 0.226; p = 0.001). In patients with a larger PI, the decrease of LL is more pronounced from standing to sitting, predominantly in the lower lumbar spine.
The differences in changes of parameters among Roussouly types
The differences in changes of lumbo-pelvic alignment among Roussouly types are shown in Table 4. From standing to sitting, the changes of several parameters (ΔPT, ΔSS, ΔLL and ΔLower LL) significantly differed among four Roussouly types. As shown in Fig. 2, ΔPT (p = 0.002), ΔSS (p < 0.001) and ΔLL (p = 0.018) of type 4 were significantly greater than those of types 1, 2 and 3, and ΔLower LL (p = 0.007) of types 3 and 4 were significantly greater than that of types 1 and 2. There existed no significant difference in ΔSVA (p = 0.105) and ΔOD-HA (p = 0.079) among the four types. Despite no significant difference (p = 0.177), ΔUpper LL of type 4 was greater than that of any other type.
Discussion
This was an attempt to investigate the decisive influence of PI on sagittal changes during standing-to-sitting transformation, and to figure out the difference in postural changes among different Roussouly types. Our results revealed that PI was correlated significantly with ΔPT, ΔSS, ΔLL, ΔUpper LL and ΔLower LL, and when standing-to-sitting, type 4 patients performed greatest ΔPT and ΔLL than other types.
Postural changes in spinal-pelvic sagittal alignment
When standing-to-sitting, we found that in patients with lumbar degenerative disease, SVA, OD-HA and PT increased significantly while SS, LL, TK, upper LL and lower LL had a significant decreasing trend. The OD-HA (odontoid hip axis) is a reliable parameter to evaluate the overall sagittal balance, and its normal range is + 2° to − 5° in asymptomatic patients [15]. Overall, when shifting from standing to sitting, the sagittal balance moved forward, the pelvis retroverted and the whole spine got flattened, which was consistent with previous studies [2, 12]. Compared with standing position, it was noted that PT/PI increased in sitting position. Mac-Thiong et al. [16] once reported the change of PT/PI was important to detect the early spinal pathology, such as spondylolisthesis. Thus, the increase of PT/PI might link to the decreased compensatory capacity of the pelvis in sitting position. In this study, we found that lower LL was larger than upper LL, regardless of posture. It is suggested that the contribution of the lower lumbar region was greater to global LL than the upper lumbar region, and the flexibility of L4-S1 was higher than L1-L4 during standing-to-sitting.
Correlations between PI and lumbo-pelvic changes
PI is a vital predicting factor among lumbo-pelvic parameters and represents the compensatory capacity of lumbo-pelvic sagittal alignment in standing position [17, 18]. In a study of asymptomatic populations, Pesenti et al. [19] found that PI affected the distribution of lumbar lordosis, and the percentage of L4-S1 lordosis and L1-L4 lordosis in global LL varied with PI. In our study, we found that PI was correlated to ΔPT, ΔSS and ΔLL significantly, which meant patients with a larger PI had a higher capacity of performing changes on sagittal alignment. Several studies have posed an opinion that lumbo-sacral fixation might limit pelvic retroversion and lumbar mobility [20, 21]. If the sagittal profile did not match the patient’s own PI value after lumbar fusion surgery, especially multisegmental lumbosacral fusion, patients could not increase their PT to the optimal value during sitting, which might affect the completion of some daily activities. The deficiency of pelvic retroversion also increased the risk of hip dislocation [9] and had a correlation to post-operation pain [22]. During preoperative planning, it is indispensable to evaluate PI and the capacity of pelvic retroversion in both standing and sitting position, which has a value in determining an appropriate restoration plan to minimize the risk of pelvic stiffness or anterior hip joint impingement.
Notably, ΔLower LL correlated more strongly with PI compared to ΔUpper LL, indicating that patients with a large PI had more loss of lumbar lordosis in L4-S1 during postural transition. Sitting required pelvic retroversion and spinal straightening, while the changes did not occur in fused segments after lumbar fusion surgery. The adjacent unfused segments tended to overcompensate, which increased the risk of the adjacent segment degeneration [23, 24]. Considering that the lower lumbar spine had greater mobility during sitting-to-standing motion, the possibility of adjacent segment disease in the upper lumbar spine would greatly increase if LL was not properly reconstructed in L4-S1 fusion surgery. Before restoring lumbar lordosis, the surgeons ought to make personalized analysis based on PI and spinal-pelvic anatomy, and select the surgical segments carefully, to prevent postoperative lumbar stiffness or junctional complications in sitting position.
Differences in postural changes among Roussouly types
Our results revealed that Roussouly type 4 patients had the most pronounced ΔPT and ΔSS. On the one hand, it might be related with higher PI values in type 4 patients. On the other hand, it suggested that compared with the other three types, type 4 patients had greater pelvic retroversion during postural changes. From standing to sitting, due to the loss of LL in type 4 patients, the overall lumbar segments tended to be flattened, resulting in forward displacement of the sagittal balance. To maintain spinal stability, type 4 patients had postural pelvic retroversion. Barrey et al. [17] once reported that PT had a certain reference value for evaluating spinal-pelvic sagittal compensation, and the pelvis would gradually retroverted as the sagittal imbalance developed. Earlier studies found that in order to retain balanced sagittal profile, pelvis retroverted further in sitting position as a compensatory mechanism [25, 26]. Considering that type 4 patients would have excessive pelvic rotation in sitting position, the ability of pelvic retroversion should be properly preserved in preoperative planning.
As shown in our study, ΔLL of type 4 patients was significantly greater than that of any other type. In types 1 and 2 patients, the lumbar curve was relatively flat and the stress mainly concentrated on the anterior and middle column when the posture changed. While in type 4 patients, the lumbar spine appeared in the shape of “C” when standing. Owing to remarkable ΔLL, the gravity produced forward shear force in sitting position which concentrated on the posterior facet joints and isthmus originally [27]. Thus, type 4 patients should pay attention to the occurrence of lumbar instability owing to greater range of motion. It may also explain the reason why sitting radiographs brought out a higher slip percentage in previous studies [3]. The ΔUpper LL and ΔLower LL of type 4 patients were the greatest, which meant that type 4 patients presented greater flexibility of the global lumbar spine than the other three types. After lumbar fusion surgery, surgeons ought to take precautions against potential challenges in adjacent segments when patients are seated.
Limitations
This study has several limitations. First of all, this was a single center study. Secondly, we only collected the preoperative imaging data in our patient clinic, with no data of patients who have undergone lumbar fusion surgery.
Conclusion
From standing to sitting position, PI plays an important role in determining the extent of lumbo-pelvic changes in patients with degenerative diseases. Among different Roussouly types, type 4 patients have the most pronounced changes of PT, SS and LL, suggesting the relatively greater flexibility of pelvis and lumbar spine.
References
Clemes SA, O’Connell SE, Edwardson CL (2014) Office workers’ objectively measured sedentary behavior and physical activity during and outside working hours. J Occup Environ Med 56:298–303. https://doi.org/10.1097/JOM.0000000000000101
Hey HWD, Teo AQA, Tan K-A et al (2017) How the spine differs in standing and in sitting—important considerations for correction of spinal deformity. Spine J 17:799–806. https://doi.org/10.1016/j.spinee.2016.03.056
Zhou Q, Sun X, Chen X et al (2021) Utility of natural sitting lateral radiograph in the diagnosis of segmental instability for patients with degenerative lumbar spondylolisthesis. Clin Orthop 479:817–825. https://doi.org/10.1097/CORR.0000000000001542
Borgeaud T, Le Huec J-C, Faundez A (2022) Pelvic and spinal postural changes between standing-sitting positions following lumbosacral fusion: a pilot study. Int Orthop 46:1839–1846. https://doi.org/10.1007/s00264-022-05365-6
Sun Z, Zhou S, Wang W et al (2020) Differences in standing and sitting spinopelvic sagittal alignment for patients with posterior lumbar fusion: important considerations for the changes of unfused adjacent segments lordosis. BMC Musculoskelet Disord 21:760. https://doi.org/10.1186/s12891-020-03777-2
Hasegawa K, Okamoto M, Hatsushikano S et al (2016) Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J 25:3675–3686. https://doi.org/10.1007/s00586-016-4702-2
Yang M, Yang C, Zhai X et al (2017) Analysis of factors associated with sagittal balance in normal asymptomatic individuals: a retrospective study in a population of east China. Spine 42:E219–E225. https://doi.org/10.1097/BRS.0000000000001782
Diebo BG, Balmaceno-Criss M, Lafage R et al (2024) Sagittal alignment in the degenerative lumbar spine: surgical planning. J Bone Jt Surg 106:445–457. https://doi.org/10.2106/JBJS.23.00672
Ochi H, Baba T, Homma Y et al (2016) Importance of the spinopelvic factors on the pelvic inclination from standing to sitting before total hip arthroplasty. Eur Spine J 25:3699–3706. https://doi.org/10.1007/s00586-015-4217-2
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30:346–353. https://doi.org/10.1097/01.brs.0000152379.54463.65
Zhang H, Hai Y, Meng X et al (2022) Validity of the Roussouly classification system for assessing distal junctional problems after long instrumented spinal fusion in degenerative scoliosis. Eur Spine J 31:258–266. https://doi.org/10.1007/s00586-021-07083-w
Sun Z, Zhou S, Jiang S et al (2022) Variations of sagittal alignment in standing versus sitting positions under the roussouly classification in asymptomatic subjects. Glob Spine J 12:772–779. https://doi.org/10.1177/2192568220962436
Laouissat F, Sebaaly A, Gehrchen M, Roussouly P (2018) Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J 27:2002–2011. https://doi.org/10.1007/s00586-017-5111-x
Amabile C, Pillet H, Lafage V et al (2016) A new quasi-invariant parameter characterizing the postural alignment of young asymptomatic adults. Eur Spine J 25:3666–3674. https://doi.org/10.1007/s00586-016-4552-y
Le Huec JC, Thompson W, Mohsinaly Y et al (2019) Sagittal balance of the spine. Eur Spine J 28:1889–1905. https://doi.org/10.1007/s00586-019-06083-1
Mac-Thiong J-M, Roussouly P, Berthonnaud É, Guigui P (2011) Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J 20:572–577. https://doi.org/10.1007/s00586-011-1923-2
Barrey C, Roussouly P, Le Huec J-C et al (2013) Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 22:834–841. https://doi.org/10.1007/s00586-013-3030-z
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20:609–618. https://doi.org/10.1007/s00586-011-1928-x
Pesenti S, Lafage R, Stein D et al (2018) The amount of proximal lumbar lordosis is related to pelvic incidence. Clin Orthop 476:1603–1611. https://doi.org/10.1097/CORR.0000000000000380
Zhou S, Zhong W, Sun Z et al (2022) The standing and sitting spino-pelvic sagittal alignment in patients with instrumented lumbar fusion might correlate with adjacent segment degeneration. Orthop Surg. https://doi.org/10.1111/os.13553
Wang S, Zhou Q, Xu L et al (2021) Impact of lumbar fusion on sitting spinopelvic balance: multisegmental versus monosegmental. Clin Neurol Neurosurg 209:106905. https://doi.org/10.1016/j.clineuro.2021.106905
Lazennec J-Y, Ramaré S, Arafati N et al (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9:47–55. https://doi.org/10.1007/s005860050008
Bagheri SR, Alimohammadi E, Zamani Froushani A, Abdi A (2019) Adjacent segment disease after posterior lumbar instrumentation surgery for degenerative disease: incidence and risk factors. J Orthop Surg 27:230949901984237. https://doi.org/10.1177/2309499019842378
Bae JS, Lee S-H, Kim J-S et al (2010) Adjacent segment degeneration after lumbar interbody fusion with percutaneous pedicle screw fixation for adult low-grade isthmic spondylolisthesis: minimum 3 years of follow-up. Neurosurgery 67:1600–1608. https://doi.org/10.1227/NEU.0b013e3181f91697
Hey HWD, Low TL, Soh HL et al (2023) Prevalence and risk factors of degenerative spondylolisthesis and retrolisthesis in the thoracolumbar and lumbar spine—an EOS study using updated radiographic parameters. Glob Spine J. https://doi.org/10.1177/21925682221134044
Zhou Q, Mm SX et al (2020) How does sagittal spinopelvic alignment of lumbar multisegmental spondylolysis differ from monosegmental spondylolysis? J Neurosurg Spine 33:211–218. https://doi.org/10.3171/2020.2.SPINE191415
Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16:1459–1467. https://doi.org/10.1007/s00586-006-0294-6
Funding
Jiangsu Provincial Medical Innovation Center of Orthopedic Surgery, CXZX202214, Yong Qiu.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, Y., Chen, H., Zhou, Q. et al. Can pelvic incidence affect changes in sagittal spino-pelvic parameters between standing and sitting positions in individuals with lumbar degenerative disease?. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08441-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08441-0