Abstract
Introduction
Despite modern fixation techniques, spinopelvic fixation failure (SPFF) after adult spinal deformity (ASD) surgery ranges from 4.5 to 38.0%, with approximately 50% requiring reoperation. Compared to other well-studied complications after ASD surgery, less is known about the incidence and predictors of SPFF.
Aims/objectives
Given the high rates of SPFF and reoperation needed to treat it, the purpose of this systematic review and meta-analysis was to report the incidence and failure mechanisms of SPF after ASD surgery.
Materials/methods
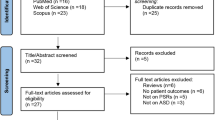
The literature search was executed across four databases: Medline via PubMed and Ovid, SPORTDiscus via EBSCO, Cochrane Library via Wiley, and Scopus. Study inclusion criteria were patients undergoing ASD surgery with spinopelvic instrumentation, report rates of SPFF and type of failure mechanism, patients over 18 years of age, minimum 1-year follow-up, and cohort or case–control studies. From each study, we collected general demographic information (age, gender, and body mass index), primary/revision, type of ASD, and mode of failure (screw loosening, rod breakage, pseudarthrosis, screw failure, SI joint pain, screw protrusion, set plug dislodgment, and sacral fracture) and recorded the overall rate of SPF as well as failure rate for each type. For the assessment of failure rate, we required a minimum of 12 months follow-up with radiographic assessment.
Results
Of 206 studies queried, 14 met inclusion criteria comprising 3570 ASD patients who underwent ASD surgery with pelvic instrumentation (mean age 65.5 ± 3.6 years). The mean SPFF rate was 22.1% (range 3–41%). Stratification for type of failure resulted in a mean SPFF rate of 23.3% for the pseudarthrosis group; 16.5% for the rod fracture group; 13.5% for the iliac screw loosening group; 7.3% for the SIJ pain group; 6.1% for the iliac screw group; 3.6% for the set plug dislodgement group; 1.1% for the sacral fracture group; and 1% for the iliac screw prominence group.
Conclusion
The aggregate rate of SPFF after ASD surgery is 22.1%. The most common mechanisms of failure were pseudarthrosis, rod fracture, and iliac screw loosening. Studies of SPFF remain heterogeneous, and a consistent definition of what constitutes SPFF is needed. This study may enable surgeons to provide patient specific constructs with pelvic fixation constructs to minimize this risk of failure.










Similar content being viewed by others
References
Sebaaly A, Gehrchen M, Silvestre C et al (2020) Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classification: a multicentric study. Eur Spine J 29(4):904–913
Anand N, Chung A, Kong C et al (2022) Prevalence and modes of posterior hardware failure with a staged protocol for circumferential minimally invasive surgical correction of adult spinal deformity: a 13-year experience. Int J Spine Surg 16(3):481–489
Eastlack RK, Soroceanu A, Mundis GM Jr et al (2022) Rates of loosening, failure, and revision of iliac fixation in adult deformity surgery. Spine (Phila Pa 1976) 47(14):986–994
De la Garza RR, Nakhla J, Sciubba DM et al (2018) Iliac screw versus S2 alar-iliac screw fixation in adults: a meta-analysis. J Neurosurg Spine 30(2):253–258
Panico M, Chande RD, Lindsey DP et al (2023) Stability and instrumentation stresses among sacropelvic fixation techniques with novel porous fusion/fixation implants: a finite element study. Int J Spine Surg 17(4):598–606
Kuklo TR, Bridwell KH, Lewis SJ et al (2001) Minimum 2-year analysis of sacropelvic fixation and L5–S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976) 26(18):1976–1983
Hyun SJ, Jung JM, Kim KJ et al (2020) Durability and failure types of S2-alar-iliac screws: an analysis of 312 consecutive screws. Oper Neurosurg (Hagerstown) 20(1):91–97
Park SJ, Park JS, Nam Y et al (2021) Failure types and related factors of spinopelvic fixation after long construct fusion for adult spinal deformity. Neurosurgery 88(3):603–611
Hallager DW, Karstensen S, Bukhari N et al (2017) Radiographic predictors for mechanical failure after adult spinal deformity surgery: a retrospective cohort study in 138 patients. Spine (Phila Pa 1976) 42(14):E855–E863
Mazur MD, Ravindra VM, Schmidt MH et al (2015) Unplanned reoperation after lumbopelvic fixation with S-2 alar-iliac screws or iliac bolts. J Neurosurg Spine 23(1):67–76
Diesing D, Franke J, Tschoeke SK et al (2019) Persistent iliosacral joint syndrome following instrumentation to the sacropelvis in patients with adult spinal deformity. J Neurol Surg A Cent Eur Neurosurg 80(1):15–25
Gao Z, Sun X, Chen C et al (2021) Comparative radiological outcomes and complications of sacral-2-alar iliac screw versus iliac screw for sacropelvic fixation. Eur Spine J 30(8):2257–2270
Bess S, Line B, Fu KM et al (2016) The health impact of symptomatic adult spinal deformity: comparison of deformity types to united states population norms and chronic diseases. Spine (Phila Pa 1976) 41(3):224–233
Diebo BG, Shah NV, Boachie-Adjei O et al (2019) Adult spinal deformity. Lancet 394(10193):160–172
Daniels AH, DePasse JM, Durand W, Hamilton DK, Passias P, Kim HJ, Protopsaltis T, Reid DB, LaFage V, Smith JS, Shaffrey C (2018) Rod fracture after apparently solid radiographic fusion in adult spinal deformity patients. World Neurosurg 117:e530–e537
Chanbour H, Hassan FM, Zuckerman SL, Park PJ, Morrissette C, Cerpa M, Lee NJ, Ha AS, Lehman RA Jr, Lenke LG (2023) Rod fractures after multi-rod constructs in adult spinal deformity patients fused to the sacrum/pelvis: where do they occur and why? Spine Deform 11(2):471–479
Merrill RK, Kim JS, Leven DM, Kim JH, Cho SK (2017) Multi-rod constructs can prevent rod breakage and pseudarthrosis at the lumbosacral junction in adult spinal deformity. Global Spine J 7(6):514–520
Zuckerman SL, Cher D, Capobianco R, Sciubba D, Polly DW (2023) Estimating the cost of spinopelvic complications after adult spinal deformity surgery. Clinicoecon Outcomes Res 9(15):765–772
Buell TJ, Yener U, Wang TR, Buchholz AL, Yen CP, Shaffrey ME, Shaffrey CI, Smith JS (2020) Sacral insufficiency fractures after lumbosacral arthrodesis: salvage lumbopelvic fixation and a proposed management algorithm. J Neurosurg Spine 27:1–12
Banno T, Hasegawa T, Yamato Y et al (2017) Prevalence and risk factors of iliac screw loosening after adult spinal deformity surgery. Spine (Phila Pa 1976) 42(17):E1024–E1030
Liu G, Hasan MY, Wong HK (2018) Subcrestal iliac-screw: a technical note describing a free hand, in-line, low profile iliac screw insertion technique to avoid side-connector use and reduce implant complications. Spine (Phila Pa 1976) 43(2):E68–E74
Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C (2006) Minimum 5-year analysis of L5–S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine 31(3):303–308
Manzetti M, Ruffilli A, Barile F et al (2023) Sacroiliac Joint degeneration and pain after spinal arthrodesis: a systematic review. Clin Spine Surg 36(4):169–182
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Cho W, Mason JR, Smith JS et al (2013) Failure of lumbopelvic fixation after long construct fusions in patients with adult spinal deformity: clinical and radiographic risk factors: clinical article. J Neurosurg Spine 19(4):445–453
El Dafrawy M, Bridwell K, Adogwa O et al (2021) Rod fractures and nonunions after long fusion to the sacrum for primary presentation adult spinal deformity: a comparison with and without interbody fusion in the distal lumbar spine. Spine Deform 9(1):231–237
Ilyas H, Place H, Puryear A (2015) A comparison of early clinical and radiographic complications of iliac screw fixation versus S2 alar iliac (S2AI) fixation in the adult and pediatric populations. J Spinal Disord Tech 28(4):E199-205
Ishida W, Elder BD, Holmes C et al (2017) Comparison between S2-alar-iliac screw fixation and iliac screw fixation in adult deformity surgery: reoperation rates and spinopelvic parameters. Global Spine J 7(7):672–680
Martin CT, Holton KJ, Elder BD et al (2022) Catastrophic acute failure of pelvic fixation in adult spinal deformity requiring revision surgery: a multicenter review of incidence, failure mechanisms, and risk factors. J Neurosurg Spine 38(1):98–106
Nguyen JH, Buell TJ, Wang TR et al (2019) Low rates of complications after spinopelvic fixation with iliac screws in 260 adult patients with a minimum 2-year follow-up. J Neurosurg Spine. https://doi.org/10.3171/2018.9.SPINE18239
Park SJ, Park JS, Lee CS et al (2021) Metal failure and nonunion at L5–S1 after long instrumented fusion distal to pelvis for adult spinal deformity: anterior versus transforaminal interbody fusion. J Orthop Surg (Hong Kong) 29(3):23094990211054224
Uotani K, Tanaka M, Sonawane S et al (2021) Comparative study of bilateral dual sacral-alar-iliac screws versus bilateral single sacral-alar-iliac screw for adult spine deformities. World Neurosurg 156:e300–e306
Petersen T, Laslett M, Juhl C (2017) Clinical classification in low back pain: best-evidence diagnostic rules based on systematic reviews. BMC Musculoskelet Disord 18(1):188
Sohn S, Park TH, Chung CK et al (2018) Biomechanical characterization of three iliac screw fixation techniques: a finite element study. J Clin Neurosci 52:109–114
Shin JK, Lim BY, Goh TS et al (2018) Effect of the screw type (S2-alar-iliac and iliac), screw length, and screw head angle on the risk of screw and adjacent bone failures after a spinopelvic fixation technique: a finite element analysis. PLoS ONE 13(8):e0201801
Homer CJ, Haselhuhn JJ, Ellingson AM et al (2023) Development of a sacral fracture model to demonstrate effects on sagittal alignment. Spine Deform. https://doi.org/10.1007/s43390-023-00721-x
Yang H, Pan A, Hai Y et al (2023) Biomechanical evaluation of multiple pelvic screws and multirod construct for the augmentation of lumbosacral junction in long spinal fusion surgery. Front Bioeng Biotechnol 11:1148342
Martin CT, Holton KJ, Jones KE et al (2021) Bilateral open sacroiliac joint fusion during adult spinal deformity surgery using triangular titanium implants: technique description and presentation of 21 cases. J Neurosurg Spine 36(1):86–92
Polly DW Jr, Holton KJ, Soriano PO et al (2022) Multiple points of pelvic fixation: stacked S2-alar-iliac screws (S2AI) or concurrent S2AI and open sacroiliac joint fusion with triangular titanium rod. JBJS Essent Surg Tech 12(4):e21.00044
Author information
Authors and Affiliations
Contributions
KO & DP contributed to study conception and design. Material preparation, data collection, and analysis were performed by KO, & HC. KO, DP, HC, & SZ commented on the previous versions of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
KO and HC declare no financial conflicts. DP has consultancies with SI-Bone, Globus, and Alexion, royalties SI-Bone and Springer (textbook), research support from Medtronic and MizuhoOSI and Medtronic. SLZ is a member of the NFL Head, Neck, and Spine Injury Committee and an Unaffiliated Neurotrauma Consultant for the NFL.
Ethical approval
Research protocol for this project, which relied on de-identified data, did not require University of Minnesota Institutional Review Board approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Odland, K., Chanbour, H., Zuckerman, S.L. et al. Spinopelvic fixation failure in the adult spinal deformity population: systematic review and meta-analysis. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08241-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08241-6