Abstract
Purpose
The aim of this study was to investigate the risks and outcomes of patients with long-term oral anticoagulation (OAC) undergoing spine surgery.
Methods
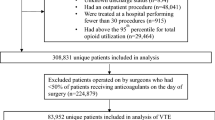
All patients on long-term OAC who underwent spine surgery between 01/2005 and 06/2015 were included. Data were prospectively collected within our in-house Spine Surgery registry and retrospectively supplemented with patient chart and administrative database information. A 1:1 propensity score-matched group of patients without OAC from the same time interval served as control. Primary outcomes were post-operative bleeding, wound complications and thromboembolic events up to 90 days post-surgery. Secondary outcomes included intraoperative blood loss, length of hospital stay, death and 3-month post-operative patient-rated outcomes.
Results
In comparison with the control group, patients with OAC (n = 332) had a 3.4-fold (95%CI 1.3–9.0) higher risk for post-operative bleeding, whereas the risks for wound complications and thromboembolic events were comparable between groups. The higher bleeding risk was driven by a higher rate of extraspinal haematomas (3.3% vs. 0.6%; p = 0.001), while there was no difference in epidural haematomas and haematoma evacuations. Risk factors for adverse events among patients with OAC were mechanical heart valves, posterior neck surgery, blood loss > 1000 mL, age, female sex, BMI > 30 kg/m2 and post-operative PTT levels. At 3-month follow-up, most patients reported favourable outcomes with no difference between groups.
Conclusion
Although OAC patients have a higher risk for complications after spine surgery, the risk for major events is low and patients benefit similarly from surgery.


Similar content being viewed by others
References
Young EY, Ahmadinia K, Bajwa N, Ahn NU (2013) Does chronic warfarin cause increased blood loss and transfusion during lumbar spinal surgery? Spine J 13:1253–1258. https://doi.org/10.1016/j.spinee.2013.05.052
Banat M, Wach J, Salemdawod A et al (2022) Antithrombotic therapy in spinal surgery does not impact patient safety–a single center cohort study. Front Surg 8:791713. https://doi.org/10.3389/fsurg.2021.791713
Zuckerman SL, Berven S, Streiff MB et al (2023) Management of anticoagulation/antiplatelet medication and venous thromboembolism prophylaxis in elective spine surgery: concise clinical recommendations based on a modified delphi process. Spine (Phila Pa 1976) 48:301–309. https://doi.org/10.1097/BRS.0000000000004540
Mannion AF, Vila-Casademunt A, Domingo-Sàbat M et al (2016) The core outcome measures index (comi) is a responsive instrument for assessing the outcome of treatment for adult spinal deformity. Eur Spine J 25:2638–2648. https://doi.org/10.1007/s00586-015-4292-4
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107. https://doi.org/10.1002/sim.3697
Heinze G, Schemper M (2002) A solution to the problem of separation in logistic regression. Stat Med 21:2409–2419. https://doi.org/10.1002/sim.1047
Heinze G, Puhr R (2010) Bias-reduced and separation-proof conditional logistic regression with small or sparse data sets. Stat Med 29:770–777. https://doi.org/10.1002/sim.3794
Stokes ME, Ye X, Shah M et al (2011) Impact of bleeding-related complications and/or blood product transfusions on hospital costs in inpatient surgical patients. BMC Health Serv Res 11:135. https://doi.org/10.1186/1472-6963-11-135
Fang A, Hu SS, Endres N, Bradford DS (2005) Risk factors for infection after spinal surgery. Spine (Phila Pa 1976) 30:1460–1465. https://doi.org/10.1097/01.brs.0000166532.58227.4f
Pull Ter Gunne AF, Van Laarhoven CJHM, Cohen DB (2010) Incidence of surgical site infection following adult spinal deformity surgery: an analysis of patient risk. Eur Spine J 19:982–988. https://doi.org/10.1007/s00586-009-1269-1
Awad JN, Kebaish KM, Donigan J et al (2005) Analysis of the risk factors for the development of post-operative spinal epidural haematoma. J Bone Joint Surg Br 87:1248–1252. https://doi.org/10.1302/0301-620X.87B9.16518
Sokolowski MJ, Garvey TA, Perl J et al (2008) Prospective study of postoperative lumbar epidural hematoma: incidence and risk factors. Spine (Phila Pa 1976) 33:108–113. https://doi.org/10.1097/BRS.0b013e31815e39af
Tafur AJ, McBane R, Wysokinski WE et al (2012) Predictors of major bleeding in peri-procedural anticoagulation management. J Thromb Haemost 10:261–267. https://doi.org/10.1111/j.1538-7836.2011.04572.x
Volovár Š, Tancošová R, Rokyta R (2018) Bridging anticoagulation therapy. Cor Vasa 60:e400–e406. https://doi.org/10.1016/j.crvasa.2018.04.002
Spyropoulos AC, Turpie A, Dunn AS et al (2006) Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost 4:1246–1252. https://doi.org/10.1111/j.1538-7836.2006.01908.x
Hart EA, Jansen R, Meijs TA et al (2017) Anticoagulant bridging in left-sided mechanical heart valve patients. Int J Cardiol 232:121–126. https://doi.org/10.1016/j.ijcard.2017.01.042
Lee MJ, Kwon JS, Jiang HB et al (2019) The antibacterial effect of non-thermal atmospheric pressure plasma treatment of titanium surfaces according to the bacterial wall structure. Sci Rep 9:1–13. https://doi.org/10.1038/s41598-019-39414-9
Nazha B, Spyropoulos AC (2016) The BRIDGE trial: What the hospitalist should know. J Hosp Med 11:652–657. https://doi.org/10.1002/jhm.2594
Douketis JD, Spyropoulos AC, Kaatz S et al (2015) Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med 373:823–833. https://doi.org/10.1056/nejmoa1501035
Siegal D, Yudin J, Kaatz S et al (2012) Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation 126:1630–1639. https://doi.org/10.1161/CIRCULATIONAHA.112.105221
Steinberg BA, Peterson ED, Kim S et al (2015) Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation findings from the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF). Circulation 131:488–494. https://doi.org/10.1161/CIRCULATIONAHA.114.011777
Spyropoulos AC, Al-Badri A, Sherwood MW, Douketis JD (2016) Periprocedural management of patients receiving a vitamin K antagonist or a direct oral anticoagulant requiring an elective procedure or surgery. J Thromb Haemost 14:875–885. https://doi.org/10.1111/jth.13305
Spyropoulos AC, Turpie AGG, Dunn AS et al (2008) Perioperative bridging therapy with unfractionated heparin or low-molecular-weight heparin in patients with mechanical prosthetic heart valves on long-term oral anticoagulants (from the REGIMEN registry). Am J Cardiol 102:883–889. https://doi.org/10.1016/j.amjcard.2008.05.042
Daniels PR, McBane RD, Litin SC et al (2009) Peri-procedural anticoagulation management of mechanical prosthetic heart valve patients. Thromb Res 124:300–305. https://doi.org/10.1016/j.thromres.2009.01.011
Croci DM, Dalolio M, Guzman R et al (2019) Direct oral anticoagulants in patients undergoing spine surgery. World Neurosurg 125:e1034–e1041. https://doi.org/10.1016/j.wneu.2019.01.236
Acknowledgements
We thank all the patients of the Schulthess Klinik who have contributed data to our in-house registry. We thank Gordana Balaban, Julian Amacker, Kirsten Clift, Selina Nauer, Sara Preziosa, Stephanie Dosch, Riccardo Curatolo and Dorian Braun for the administration of the Spine Tango Surgery and Patient Self-Assessment forms.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have neither any conflicts of interest nor competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sweda, R., Mannion, A.F., O’Riordan, D. et al. A decade of experience in over 300 surgically treated spine patients with long-term oral anticoagulation: a propensity score matched cohort study. Eur Spine J 33, 1360–1368 (2024). https://doi.org/10.1007/s00586-024-08134-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-024-08134-8