Abstract
Introduction
Pseudarthrosis after cervical spine surgery represents an underreported and challenging complication. Using a large multi-center surgical database, we sought to: (1) report the incidence of cervical pseudarthrosis, (2) evaluate changes in rates of cervical pseudarthrosis, and (3) describe risk factors for suboptimal outcomes after cervical pseudarthrosis surgery.
Methods
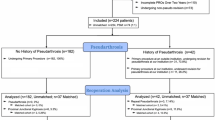
The American College of Surgeons National Surgical Quality Improvement Program database from 2012 to 2019 was used. The primary outcome was occurrence of a cervical fusion procedure with a prior diagnosis of pseudarthrosis. Fusion for pseudarthrosis was divided into anterior and posterior approaches. Post-operative complications were classified as major or minor. Prolonged LOS was defined as exceeding the 75th percentile for total hospital stay.
Results
A total of 780 patients underwent cervical fusion for pseudarthrosis, and a significant increase in rates of surgery for pseudarthrosis was seen (0.25–1.2%, p < 0.001). The majority of cervical pseudarthrosis was treated with a posterior approach (66.5%). Postoperatively, 38 (4.9%) patients suffered a complication and 247 (31.7%) had a prolonged LOS. The three strongest risk factors for complications and extended LOS were > 10% weight loss preoperatively, congestive heart failure, and pre-operative bleeding disorder.
Conclusion
Results from a large multi-center national database revealed that surgery to treat cervical pseudarthrosis has increased from 2012 to 2019. Most pseudarthrosis was treated with a posterior approach. Reoperation to treat cervical pseudarthrosis carried risk, with 5% having complications and 32% having an extended LOS. These results lay the groundwork for a future prospective study to discern the true incidence of cervical pseudarthrosis and how to best avoid its occurrence.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Badiee RK, Mayer R, Pennicooke B et al (2020) Complications following posterior cervical decompression and fusion: a review of incidence, risk factors, and prevention strategies. J Spine Surg 6:323–333. https://doi.org/10.21037/jss.2019.11.01
Leven D, Cho SK (2016) Pseudarthrosis of the cervical spine: risk factors, diagnosis and management. Asian Spine J 10:776–786. https://doi.org/10.4184/asj.2016.10.4.776
Zuckerman SL, Devin CJ (2022) Pseudarthrosis of the cervical spine. Clin Spine Surg 35:97–106. https://doi.org/10.1097/BSD.0000000000001259
Lin W, Ha A, Boddapati V et al (2018) Diagnosing pseudoarthrosis after anterior cervical discectomy and fusion. Neurospine 15:194–205. https://doi.org/10.14245/ns.1836192.096
Wang JC, McDonough PW, Endow KK, Delamarter RB (2000) Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine 25:41–45. https://doi.org/10.1097/00007632-200001010-00009
McAnany SJ, Baird EO, Overley SC et al (2015) A meta-analysis of the clinical and fusion results following treatment of symptomatic cervical pseudarthrosis. Glob Spine J 5:148–155. https://doi.org/10.1055/s-0035-1544176
Carreon L, Glassman SD, Campbell MJ (2006) Treatment of anterior cervical pseudoarthrosis: posterior fusion versus anterior revision. Spine J 6:154–156. https://doi.org/10.1016/j.spinee.2005.07.003
Phillips FM, Carlson G, Emery SE, Bohlman HH (1997) Anterior cervical pseudarthrosis. Nat Hist Treat Spine 22:1585–1589. https://doi.org/10.1097/00007632-199707150-00012
Pennington Z, Mehta VA, Lubelski D et al (2020) Quality of life and cost implications of pseudarthrosis after anterior cervical discectomy and fusion and its subsequent revision surgery. World Neurosurg 133:e592–e599. https://doi.org/10.1016/j.wneu.2019.09.104
Song K-S, Piyaskulkaew C, Chuntarapas T et al (2014) Dynamic radiographic criteria for detecting pseudarthrosis following anterior cervical arthrodesis. J Bone Joint Surg Am 96:557–563. https://doi.org/10.2106/JBJS.M.00167
Song K-S, Chaiwat P, Kim HJ et al (2013) Anterior cervical fusion assessment using reconstructed computed tomographic scans: surgical confirmation of 254 segments. Spine 38:2171–2177. https://doi.org/10.1097/BRS.0000000000000017
Rhee JM, Chapman JR, Norvell DC et al (2015) Radiological determination of postoperative cervical fusion: a systematic review. Spine 40:974–991. https://doi.org/10.1097/BRS.0000000000000940
Sebastian A, Huddleston P, Kakar S et al (2016) Risk factors for surgical site infection after posterior cervical spine surgery: an analysis of 5,441 patients from the ACS NSQIP 2005–2012. Spine J 16:504–509. https://doi.org/10.1016/j.spinee.2015.12.009
Passias PG, Bortz C, Alas H et al (2019) Alcoholism as a predictor for pseudarthrosis in primary spine fusion: an analysis of risk factors and 30-day outcomes for 52,402 patients from 2005 to 2013. J Orthop 16:36–40. https://doi.org/10.1016/j.jor.2018.12.011
Salvetti DJ, Tempel ZJ, Gandhoke GS et al (2015) Preoperative prealbumin level as a risk factor for surgical site infection following elective spine surgery. Surg Neurol Int 6:S500–S503. https://doi.org/10.4103/2152-7806.166893
Kothari P, Lee NJ, Leven DM et al (2016) Impact of gender on 30-day complications after adult spinal deformity surgery. Spine 41:1133–1138. https://doi.org/10.1097/BRS.0000000000001499
Wewel JT, Kasliwal MK, Adogwa O et al (2019) Fusion rate following three- and four-level ACDF using allograft and segmental instrumentation: a radiographic study. J Clin Neurosci 62:142–146. https://doi.org/10.1016/j.jocn.2018.11.040
Shousha M, Alhashash M, Allouch H, Boehm H (2019) Reoperation rate after anterior cervical discectomy and fusion using standalone cages in degenerative disease: a study of 2,078 cases. Spine J 19:2007–2012. https://doi.org/10.1016/j.spinee.2019.08.003
Bergin SM, Wang TY, Park C et al (2021) Pseudarthrosis rate following anterior cervical discectomy with fusion using an allograft cellular bone matrix: a multi-institutional analysis. Neurosurg Focus 50:E6. https://doi.org/10.3171/2021.3.FOCUS2166
Steinhaus ME, York PJ, Bronheim RS et al (2020) Outcomes of revision surgery for pseudarthrosis after anterior cervical fusion: case series and systematic review. Glob Spine J 10:559–570. https://doi.org/10.1177/2192568219863808
Ren C, Qin R, Wang P, Wang P (2020) Comparison of anterior and posterior approaches for treatment of traumatic cervical dislocation combined with spinal cord injury: minimum 10-year follow-up. Sci Rep 10:10346. https://doi.org/10.1038/s41598-020-67265-2
Siccoli A, Schröder ML, Staartjes VE (2021) Influence of dynamic preoperative body mass index changes on patient-reported outcomes after surgery for degenerative lumbar spine disease. Neurosurg Rev 44:2689–2696. https://doi.org/10.1007/s10143-020-01454-5
Rudy HL, Cho W, Oster BA et al (2020) Rapid bodyweight reduction before lumbar fusion surgery increased postoperative complications. Asian Spine J 14:613–620. https://doi.org/10.31616/asj.2019.0236
Maza NM, Ferrer CE, Qureshi SA et al (2019) Contained-delivery route and the administration of postoperative steroids following anterior cervical spinal fusion with low-dose rhBMP-2 reduces the magnitude of respiratory compromise. Clin Spine Surg 32:E420–E425. https://doi.org/10.1097/BSD.0000000000000850
Lord EL, Cohen JR, Buser Z et al (2017) Trends, costs, and complications of anterior cervical discectomy and fusion with and without bone morphogenetic protein in the United States Medicare population. Glob Spine J 7:603–608. https://doi.org/10.1177/2192568217699207
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
*This work has not been presented in any forum.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jo, J., Lakomkin, N., Zuckerman, S.L. et al. The incidence of reoperation for pseudarthrosis after cervical spine surgery. Eur Spine J 33, 1275–1282 (2024). https://doi.org/10.1007/s00586-023-08058-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08058-9