Abstract
Background
A network meta-analysis aims to help clinicians make clinical decisions on the most effective treatment for a certain condition. Neck pain is multifactorial, with various classification systems and treatment options. Classifying patients and grouping interventions in clinically relevant treatment nodes for a NMA is essential, but this process is poorly defined.
Objective
Our aim is to obtain consensus among experts on neck pain classifications and the grouping of interventions into nodes for a future network meta-analysis.
Design
A Delphi consensus study involving neck pain experts worldwide.
Methods
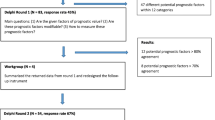
We invited authors of neck pain clinical practice guidelines published from 2014 onwards. The Delphi baseline questionnaire was developed based on the findings of a scoping review, including four items on classifications and 19 nodes. Participants were asked to record their level of agreement on a seven-point Likert scale or using Yes/No/Not sure answer options for the various statements. We used descriptive analysis to summarise the responses on each statement with content analysis of the free-text comments.
Results
In total, 18/80 experts (22.5%) agreed to participate in one or more Delphi rounds. We needed three rounds to reach consensus for two classification of neck pain: one based on aetiology and one on duration. In addition, we also reached consensus on the grouping of interventions, including a definition of each node, with the number of nodes reduced to 17.
Conclusion
With this consensus we clinically validated two neck pain classifications and grouped conservative treatments into 17 well-defined and clinically relevant nodes.

Similar content being viewed by others
References
S Kazeminasab SA Nejadghaderi P Amiri 2022 Neck pain: global epidemiology, trends and risk factors BMC Musculoskelet Disord 23 1 26 https://doi.org/10.1186/s12891-021-04957-4
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9. Erratum in: Lancet. 2020 Nov 14;396(10262):1562.
N Henschke SJ Kamper CG Maher 2015 The epidemiology and economic consequences of pain Mayo Clin Proc 90 1 139 147 https://doi.org/10.1016/j.mayocp.2014.09.010
P Jennum J Kjellberg R Ibsen T Bendix 2013 Health, social, and economic consequences of neck injuries: a controlled national study evaluating societal effects on patients and their partners Spine (Phila Pa 1973) 38 5 449 457 https://doi.org/10.1097/BRS.0b013e3182819203
P Parikh P Santaguida J Macdermid 2019 Comparison of CPG's for the diagnosis, prognosis and management of non-specific neck pain: a systematic review BMC Musculoskelet Disord 20 1 81 https://doi.org/10.1186/s12891-019-2441-3
AP Verhagen 2021 Physiotherapy management of neck pain J Physiother 67 1 5 11 https://doi.org/10.1016/j.jphys.2020.12.005
J IntHout JP Ioannidis GF Borm 2016 Obtaining evidence by a single well-powered trial or several modestly powered trials Stat Methods Med Res 25 2 538 552 https://doi.org/10.1177/0962280212461098
N Graham A Gross CH Goldsmith 2008 Mechanical traction for neck pain with or without radiculopathy Cochrane Database Syst Rev 3 CD006408 https://doi.org/10.1002/14651858.CD006408.pub2
A Gross M Forget K St George 2012 Patient education for neck pain Cochrane Database Syst Rev 3 005106 https://doi.org/10.1002/14651858.CD005106.pub4
A Gross TM Kay JP Paquin 2015 Cervical overview group: Exercises for mechanical neck disorders Cochrane Database Syst Rev 1 1 004250 https://doi.org/10.1002/14651858.CD004250.pub5
A Gross P Langevin SJ Burnie 2015 Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment Cochrane Database Syst Rev 9 v004249x https://doi.org/10.1002/14651858.CD004249.pub4
Haines T, Gross A, Burnie SJ et al (2009) Patient education for neck pain with or without radiculopathy. Cochrane Database Syst Rev 1:CD005106. https://doi.org/10.1002/14651858.CD005106.pub3. Update in: Cochrane Database Syst Rev. 2012;3:CD005106
P Kroeling A Gross N Graham 2013 Electrotherapy for neck pain Cochrane Database Syst Rev https://doi.org/10.1002/14651858.CD004251.pub5
M Monticone E Ambrosini C Cedraschi 2015 Cognitive-behavioral treatment for subacute and chronic neck pain: a cochrane review Spine (Phila Pa 1973) 40 19 1495 1504 https://doi.org/10.1097/BRS.0000000000001052
KC Patel A Gross N Graham 2012 Massage for mechanical neck disorders Cochrane Database Syst Re https://doi.org/10.1002/14651858.CD004871.pub4
Trinh K, Graham N, Irnich D et al (2016) Acupuncture for neck disorders. Cochrane Database Syst Rev.;(5):CD004870. https://doi.org/10.1002/14651858.CD004870.pub4. Update in: Cochrane Database Syst Rev. 2016 Nov 17;11:CD004870.
Verhagen AP, Bierma-Zeinstra SM, Burdorf A, et al 2013 Conservative interventions for treating work-related complaints of the arm, neck or shoulder in adults. Cochrane Database Syst Rev. 12:CD008742. https://doi.org/10.1002/14651858.CD008742.pub2.
B Rouse A Chaimani T Li 2017 Network meta-analysis: an introduction for clinicians Intern Emerg Med 12 1 103 111 https://doi.org/10.1007/s11739-016-1583-7
C Lunny AC Tricco AA Veroniki 2021 Methodological review to develop a list of bias items used to assess reviews incorporating network meta-analysis: protocol and rationale BMJ Open 11 6 e045987 https://doi.org/10.1136/bmjopen-2020-045987
G Salanti 2012 Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool Res Synth Methods 3 2 80 97 https://doi.org/10.1002/jrsm.1037
MR Phillips DH Steel CC Wykoff JW Busse RR Bannuru L Thabane M Bhandari V Chaudhary 2022 Retina Evidence Trials InterNational Alliance (R.E.T.I.N.A.) Study Group: a clinician's guide to network meta-analysis Eye Lond 36 8 1523 1526 https://doi.org/10.1038/s41433-022-01943-5
A James A Yavchitz P Ravaud I Boutron 2018 Node-making process in network meta-analysis of nonpharmacological treatment are poorly reported J Clin Epidemiol 97 95 102 https://doi.org/10.1016/j.jclinepi.2017.11.018
MK Bagg G Salanti JH McAuley 2018 Comparing interventions with network meta-analysis J Physiother 64 2 128 132 https://doi.org/10.1016/j.jphys.2018.02.014
C Shi M Westby G Norman 2018 Node-making processes in network meta-analysis of nonpharmacological interventions should be well planned and reported J Clin Epidemiol 101 124 125 https://doi.org/10.1016/j.jclinepi.2018.04.009
A Xing L Lin 2020 Effects of treatment classifications in network meta-analysis Res Methods Med Health Sci 1 1 12 24 https://doi.org/10.1177/2632084320932756
TC Hoffmann AD Oxman JP Ioannidis 2017 Enhancing the usability of systematic reviews by improving the consideration and description of interventions BMJ 358 j2998 https://doi.org/10.1136/bmj.j2998
CD Giovane L Vacchi D Mavridis 2013 Network meta-analysis models to account for variability in treatment definitions: application to dose effects Stat Med 32 1 25 39 https://doi.org/10.1002/sim.5512
PC Gotzsche 2000 Why we need a broad perspective on meta-analysis: It may be crucially important for patients BMJ 321 7261 585 586 https://doi.org/10.1136/bmj.321.7261.585
I Ishaq P Mehta IW Skinner MK Bagg J Bier AP Verhagen 2023 Treatment classifications and interventions for neck pain: a scoping review J Clin Epidemiol https://doi.org/10.1016/j.jclinepi.2023.04.010
I Belton A Macdonald G Wright I Hamlin 2019 Improving the practical application of the Delphi method in group-based judgment: a six-step prescription for a well-founded and defensible process Technol Forecast Soc Chang 147 72 82 https://doi.org/10.1016/j.techfore.2019.07.002
S Jünger SA Payne J Brine L Radbruch SG Brearley 2017 Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: recommendations based on a methodological systematic review Palliat Med 31 684 706 https://doi.org/10.1177/0269216317690685
I Ishaq IW Skinner P Mehta AP Verhagen 2021 Developing consensus on the classification of neck pain and the grouping of treatments: A delphi study protocol Open Sci Framew 1 22 233 https://doi.org/10.17605/OSF.IO/EBZTN
J Bier WGM Scholten-Peeters JB Staal 2018 Clinical practice guideline for physical therapy assessment and treatment in patients with nonspecific neck pain Phys Ther Rehab J 98 3 162 171 https://doi.org/10.1093/ptj/pzx118
PR Blanpied AR Gross JM Elliott 2017 Neck Pain: Revision 2017 clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association J Orthop Sports Phys Ther 47 7 A1 A83 https://doi.org/10.2519/jospt.2017.0302
R Bryans P Decina M Descarreaux 2014 Evidence-based guidelines for the chiropractic treatment of adults with neck pain J Manip Physiol Ther 37 1 42 63 https://doi.org/10.1016/j.jmpt.2013.08.010
AE Bussieres G Stewart F Al-Zoubi 2016 The treatment of neck pain–associated disorders and whiplash-associated disorders: A clinical practice guideline J Manip Physiol Ther 39 8 523 564 https://doi.org/10.1016/j.jmpt.2016.08.007
P Côté JJ Wong D Sutton 2016 Management of neck pain and associated disorders: a clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration Eur Spine J 25 7 2000 2022 https://doi.org/10.1007/s00586-016-4467-7
P Kjaer A Kongsted J Hartvigsen 2017 National clinical guidelines for non-surgical treatment of patients with recent onset neck pain or cervical radiculopathy Eur Spine J 26 9 2242 2257 https://doi.org/10.1007/s00586-017-5121-8
State Insurance Regulatory Authority (2014) Guidelines for the management of acute whiplash-associated disorders—for health professionals. https://www.sira.nsw.gov.au/resources-library/motor-accident-resources/publications/for-professionals/whiplash-resources/SIRA08104-Whiplash-Guidelines-1117-396479.pdf
Qualtrics (2005) Qualtrics (Version November 2021) [Online survey tool]. Qualtrics. https://www.qualtrics.com
E Ho M Ferreira L Chen 2020 Psychological interventions for chronic non-specific low back pain: protocol of a systematic review with network meta-analysis BMJ Open 10 9 e034996 https://doi.org/10.1136/bmjopen-2019-034996
T Thompson S Dias D Poulter 2020 Efficacy and acceptability of pharmacological and non-pharmacological interventions for non-specific chronic low back pain: a protocol for a systematic review and network meta-analysis Syst Rev 5 9 130 https://doi.org/10.1186/s13643-020-01398-3
T Li MA Puhan SS Vedula 2011 Ad Hoc Network Meta-analysis Methods Meeting Working Group. Network meta-analysis-highly attractive but more methodological research is needed BMC Med 9 79 https://doi.org/10.1186/1741-7015-9-79
GF Moore S Audrey M Barker 2015 Process evaluation of complex interventions: Medical Research Council guidance BMJ 19 350 h1258 https://doi.org/10.1136/bmj.h1258
GF Moore RE Evans J Hawkins 2017 All interventions are complex, but some are more complex than others: using iCAT_SR to assess complexity Cochrane Database Syst Rev 7 ED000122 https://doi.org/10.1002/14651858.ED000122
Acknowledgements
We would like to thank all Dephi participants for their collaboration: Carlo Ammendolia, Paul Beattie, Jasper Bier, Peter Blanpied, Andre Bussieres, Ian Cameron, Pierre Côte, Joseph Godges, Anita Gross, Inge Ris Hansen, Jill Hayden, Joseph Ierano, Per Kjaer, Henrik Hein Lauridsen, Joy Macdermid, Margaretha Nordin, Jesper Nørregaard, Isabelle Pagé, Jan Pool, Pasqualine Santaguida, Michelle Sterling, David Walton, and Jessica Wong. This research was conducted as part of the PhD candidature of the first author at the University of Technology Sydney, funded by an Australian Government Research Training Program Scholarship.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ishaq, I., Skinner, I.W., Mehta, P. et al. Clinical validation of grouping conservative treatments in neck pain for use in a network meta-analysis: a Delphi consensus study. Eur Spine J 33, 166–175 (2024). https://doi.org/10.1007/s00586-023-08025-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08025-4