Abstract
Purpose
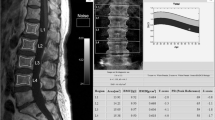
Magnetic Resonance Imaging (MRI) is frequently utilised to aid in the comprehensive assessment of back pain, while dual-energy x-ray absorptiometry (DEXA) is the gold standard test for the assessment of bone density. Assessing bone density on MRI could reduce costs and avoid exposing patients to ionising radiation. The aim of this paper is to investigate whether the relative signal intensity of vertebral bodies compared to other structures can detect osteoporosis on MRI.
Methods
100 patients that had undergone both a lumbar spine MRI and a DEXA scan were identified. The T1 and T2 signal intensity of L1–L4 vertebral bodies (VB), cerebro-spinal fluid (CSF), and psoas muscle were measured within a 1-cm2 region of interest (ROI), and the signal intensity ratios were calculated. The ratios were stratified as normal, osteopenic, or osteoporotic based on DEXA T-scores.
Results
The T1 VB /T1 CSF ratio was significantly higher in the osteoporotic group than the normal and osteopenic groups (p < 0.001). The T1 VB /T1 CSF ratio had excellent discrimination (AUC = 0.841) for the presence of osteoporosis. The Pearson correlation coefficient between the DEXA T-score and the T1 VB/T1 CSF ratio was -0.474 (p < 0.001). The intra-observer (ICC = 0.910, 95% CI = 0.757–0.966) and inter-observer reliability (ICC = 0.927, 95% CI = 0.824–0.970) were excellent. In our cohort, a T1 VB / T1 CSF ratio of greater than 4 is 66.7% sensitive but 90.0% specific for the presence of osteoporosis.
Conclusion
A high T1 VB/T1 CSF ratio suggests osteoporosis on MRI. Prospective validation is needed to confirm these findings.




Similar content being viewed by others
References
Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, Cooper C (2020) The epidemiology of osteoporosis. Br Med Bull 133(1):105–117. https://doi.org/10.1093/bmb/ldaa005
Svedbom A, Hernlund E, Ivergård M et al (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8(1):137. https://doi.org/10.1007/s11657-013-0137-0
Morgan SL, Prater GL (2017) Quality in dual-energy X-ray absorptiometry scans. Bone 104:13–28. https://doi.org/10.1016/j.bone.2017.01.033
Porter JL, Varacallo M (2022) Osteoporosis. In: StatPearls. StatPearls Publishing. Accessed March 16, 2023. http://www.ncbi.nlm.nih.gov/books/NBK441901/
Kanis JA (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 4(6):368–381. https://doi.org/10.1007/BF01622200
Citrin CM, Sherman JL, Gangarosa RE, Scanlon D (1987) Physiology of the CSF flow-void sign: modification by cardiac gating. AJR Am J Roentgenol 148(1):205–208. https://doi.org/10.2214/ajr.148.1.205
Saad MM, Ahmed AT, Mohamed KE, Habba MR (2019) Role of lumbar spine signal intensity measurement by MRI in the diagnosis of osteoporosis in post-menopausal women. Egypt J Radiol Nucl Med 50(1):35. https://doi.org/10.1186/s43055-019-0046-3
Ehresman J, Pennington Z, Schilling A et al (2020) Novel MRI-based score for assessment of bone density in operative spine patients. Spine J 20(4):556–562. https://doi.org/10.1016/j.spinee.2019.10.018
Liu J, Liao JW, Li W (2022) Assessment of Osteoporosis in Lumbar Spine: In Vivo Quantitative MR Imaging of Collagen Bound Water in Trabecular Bone. Front Endocrinol 13:801930. https://doi.org/10.3389/fendo.2022.801930
Sheu A, Diamond T (2016) Bone mineral density: testing for osteoporosis. Aust Prescr 39(2):35–39. https://doi.org/10.18773/austprescr.2016.020
Njeh CF, Fuerst T, Hans D, Blake GM, Genant HK (1999) Radiation exposure in bone mineral density assessment. Appl Radiat Isot Data Instrum Methods Use Agric Ind Med 50(1):215–236. https://doi.org/10.1016/s0969-8043(98)00026-8
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare(s) that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saad, A., Jenko, N., Petrou, E. et al. Assessing bone density on MRI: comparison between routine MRI sequences and DEXA scans. Eur Spine J 33, 1498–1503 (2024). https://doi.org/10.1007/s00586-023-08021-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-08021-8