Abstract
Background
Proximal junctional kyphosis (PJK) is a complication following surgery for adult spinal deformity (ASD) possibly ameliorated by polymethyl methacrylate (PMMA) vertebroplasty of the upper instrumented vertebrae (UIV). This study quantifies PJK following surgical correction bridging the thoracolumbar junction ± PMMA vertebroplasty.
Methods
ASD patients from 2013 to 2020 were retrospectively reviewed and included with immediate postoperative radiographs and at least one follow-up radiograph. PMMA vertebroplasty at the UIV and UIV + 1 was performed at the surgeons’ discretion.
Results
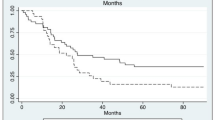
Of 102 patients, 56% received PMMA. PMMA patients were older (70 ± 8 vs. 66 ± 10, p = 0.021), more often female (89.3% vs. 68.2%, p = 0.005), and had more osteoporosis (26.8% vs. 9.1%, p = 0.013). 55.4% of PMMA patients developed PJK compared to 38.6% of controls (p = 0.097), and the rate of PJK development was not different between groups in univariate survival models. There was no difference in PJF (p > 0.084). Reoperation rates were 7.1% in PMMA versus 11.4% in controls (p = 0.501). In multivariable models, PJK development was not associated with the use of PMMA vertebroplasty (HR 0.77, 95% CI 0.38–1.60, p = 0.470), either when considered overall in the cohort or specifically in those with poor bone quality. PJK was significantly predicted by poor bone quality irrespective of PMMA use (HR 3.81, p < 0.001).
Conclusions
In thoracolumbar fusions for adult spinal deformity, PMMA vertebroplasty was not associated with reduced PJK development, which was most highly associated with poor bone quality. Preoperative screening and management for osteoporosis is critical in achieving an optimal outcome for these complex operations.
Level of evidence
4, retrospective non-randomized case review.




Similar content being viewed by others
References
Crawford CH, Glassman SD, Mummaneni PV et al (2016) Back pain improvement after decompression without fusion or stabilization in patients with lumbar spinal stenosis and clinically significant preoperative back pain. J Neurosurg Spine 25:596–601. https://doi.org/10.3171/2016.3.SPINE151468
Schwab FJ, Hawkinson N, Lafage V et al (2012) Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 21:2603–2610. https://doi.org/10.1007/s00586-012-2370-4
Glattes RC, Bridwell KH, Lenke LG et al (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine 30:1643–1649
Kim YJ, Bridwell KH, Lenke LG et al (2006) Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine (Phila Pa 1976) 31:2359–2366. https://doi.org/10.1097/01.brs.0000238969.59928.73
Hart RA, McCarthy I, Ames CP et al (2013) Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am 24:213–218. https://doi.org/10.1016/j.nec.2013.01.001
Hostin R, McCarthy I, OʼBrien M et al (2013) Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976) 38:1008–1015. https://doi.org/10.1097/BRS.0b013e318271319c
Kim HJ, Iyer S (2016) Proximal junctional kyphosis. J Am Acad Orthop Surg 24:318–326. https://doi.org/10.5435/JAAOS-D-14-00393
Kim HJ, Bridwell KH, Lenke LG et al (2013) Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine (Phila Pa 1976) 38:896–901. https://doi.org/10.1097/BRS.0b013e3182815b42
Smith MW, Annis P, Lawrence BD et al (2013) Early proximal junctional failure in patients with preoperative sagittal imbalance. Evid Based Spine Care J 4:163–164. https://doi.org/10.1055/s-0033-1357366
O’Leary PT, Bridwell KH, Lenke LG et al (2009) Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: a matched cohort analysis performed at a single center. Spine (Phila Pa 1976) 34:2134–2139. https://doi.org/10.1097/BRS.0b013e3181b2e17e
Liu J-T, Li C, Chang C-S, Liao W-J (2015) Long-term follow-up study of osteoporotic vertebral compression fracture treated using balloon kyphoplasty and vertebroplasty. J Neurosurg Spine 23:94–98. https://doi.org/10.3171/2014.11.SPINE14579
Kebaish KM, Martin CT, O’Brien JR et al (2013) Use of vertebroplasty to prevent proximal junctional fractures in adult deformity surgery: a biomechanical cadaveric study. Spine J 13:1897–1903. https://doi.org/10.1016/j.spinee.2013.06.039
Feltes C, Fountas KN, Machinis T et al (2005) Immediate and early postoperative pain relief after kyphoplasty without significant restoration of vertebral body height in acute osteoporotic vertebral fractures. Neurosurg Focus 18:e5. https://doi.org/10.3171/foc.2005.18.3.6
Theologis AA, Burch S (2015) Prevention of acute proximal junctional fractures after long thoracolumbar posterior fusions for adult spinal deformity using 2-level cement augmentation at the upper instrumented vertebra and the vertebra 1 level proximal to the upper instrumented vertebra. Spine 40:1516–1526
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103. https://doi.org/10.1007/s005860050038
Jeong-Hoon C, Jee-Soo J, Hyeun-Sung K, Il-Tae J (2017) What is the more appropriate proximal fusion level for adult lumbar degenerative flat back? World Neurosurg. https://doi.org/10.1016/j.wneu.2017.03.051
Kim YJ, Bridwell KH, Lenke LG et al (2008) Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 33:2179–2184. https://doi.org/10.1097/BRS.0b013e31817c0428
Kim JS, Phan K, Cheung ZB et al (2019) Surgical, radiographic, and patient-related risk factors for proximal junctional kyphosis: a meta-analysis. Global Spine J 9:32–40. https://doi.org/10.1177/2192568218761362
Lafage R, Schwab F, Glassman S et al (2017) Age-adjusted alignment goals have the potential to reduce PJK. Spine (Phila Pa 1976) 42:1275–1282
Yilgor C, Sogunmez N, Boissiere L et al (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Jt Surg Am 99:1661–1672. https://doi.org/10.2106/JBJS.16.01594
Copay AG, Glassman SD, Subach BR et al (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the oswestry disability index, medical outcomes study questionnaire short form 36, and pain scales. Spine J 8:968–974. https://doi.org/10.1016/j.spinee.2007.11.006
Yoo J-I, Ha Y-C, Ryu H-J et al (2017) Teriparatide treatment in elderly patients with sacral insufficiency fracture. J Clin Endocrinol Metab 102:560–565
Funding
Arthur R. Bartolozzi: Nothing to disclose, no funding. Yousi A. Oquendo: Nothing to disclose, Stanford Med-Scholars provided funding supporting this project. Jayme C.B. Koltsov: Nothing to Disclose. Todd F. Alamin: None relevant to this study. Medtronic advisory board. Globus consulting and royalties. Nuvasive consultant. Spinal elements royalties. Empirical spine consulting. Kirkham B. Wood: Royalties: Globus, Consulting: Stryker, Nanovis, Lifespine. Ivan Cheng: Consulting: Surgalign, SeaSpine, Nuvasive. Royalties: Nuvasive, Globus, SpineWave. Stocks: Cytonics, SpinalCyte. No other related interests or funding. Serena S. Hu: Board of Directors: AOA (None), SRS (Nonfinancial), SRS (None); Other: OnPoint (None); Royalties: MiRus (None); Stock Ownership: Nuvasive.
Author information
Authors and Affiliations
Contributions
ARB designed the study and data collection instruments reviewed data and drafted the manuscript, YAO reviewed imaging and charts and secured funding for this support, JCBK performed all data analysis and statistics, TFA, KBW, and IC provided cases and feedback in study design as well as reviews of manuscripts, and SSH provided senior mentorship throughout every stage of the project, provided cases as well as initial question and study design.
Corresponding author
Ethics declarations
Conflict of interests
None of the authors have conflicts of interest in financial entities related to the content and conclusions of this article. Further agreements and funding are delineated below.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bartolozzi, A.R., Oquendo, Y.A., Koltsov, J.C.B. et al. Polymethyl methacrylate augmentation and proximal junctional kyphosis in adult spinal deformity patients. Eur Spine J 33, 599–609 (2024). https://doi.org/10.1007/s00586-023-07966-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07966-0