Abstract
Purpose
The aim of this systematic review was primarily to identify the types of mHealth technologies for the rehabilitation of non-specific spinal disorders, second to evaluate their efficacy, and finally to determine their applicability in LMICs.
Methods
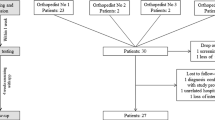
Three databases (Scopus, PubMed, and Web of Science) were searched for randomized controlled trials and clinical trials from January 2012 until December 2022. Studies were found eligible when using mHealth technologies for the rehabilitation of non-specific spinal disorders. To evaluate efficacy, the primary outcome was pain intensity, and the secondary outcomes were disability and quality of life. To evaluate the applicability in LMICs, information about financial and geographical accessibility, offline usability, and languages was extracted.
Results
Fifteen studies were included comprising 1828 participants who suffer from non-specific low back pain (86.05%) and non-specific neck pain (13.95%). Fourteen distinct smartphone-based interventions and two sensor system interventions were found, with a duration ranging from four weeks to six months. All mHealth interventions demonstrated efficacy for the improvement of pain, disability and quality of life in non-specific spinal disorders, particularly low back pain. Five of the evaluated smartphone applications were free of charge accessible and had language features that could be adapted for use in LMICs.
Conclusion
mHealth interventions can be used and integrated into the conventional treatment of non-specific spinal disorders in rehabilitation. They have demonstrated efficacy and could be implemented in LMICs with minor adaptations to overcome language barriers and the absolute necessity of the internet.



Similar content being viewed by others
References
Alshami AM (2015) Prevalence of spinal disorders and their relationships with age and gender. Saudi Med J 36(6):725–730
Raciborski F, Gasik R, Kłak A (2016) Disorders of the spine. A major health and social problem. Reumatologia 54(4):196–200
Wu A, March L, Zheng X, Huang J, Wang X, Zhao J et al (2020) Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med mars 8(6):299
Binder AI (2008) Neck pain. BMJ. Clin Evid 4:1103
Kazeminasab S, Nejadghaderi SA, Amiri P, Pourfathi H, Araj-Khodaei M, Sullman MJM et al (2022) Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord 23(1):26
Chen S, Chen M, Wu X, Lin S, Tao C, Cao H et al (2019) Global, regional and national burden of low back pain 1990–2019: a systematic analysis of the Global Burden of Disease study. J Orthop Transl 32:49–58
Sharma S, McAuley JH (2022) Low back pain in low- and middle-income countries, Part 1: the problem. J Orthopaed Sports Phys Therapy. https://doi.org/10.2519/jospt.2022.11145
Morris LD, Daniels KJ, Ganguli B, Louw QA (2018) An update on the prevalence of low back pain in Africa: a systematic review and meta-analyses. BMC Musculoskelet Disord déc 19(1):196
Kossi O, Yamadjako D, Timmermans A, Michiels S, Adoukonou T, Janssens L (2022) Prevalence and biopsychosocial factors associated with chronic low back pain in urban and rural communities in Western Africa: a population-based door-to-door survey in Benin. Eur Spine J 31(11):2897–2906
Froud R, Patterson S, Eldridge S, Seale C, Pincus T, Rajendran D et al (2014) A systematic review and meta-synthesis of the impact of low back pain on people’s lives. BMC Musculoskelet Disord 15(1):50
Koes BW, van Tulder MW, Thomas S (2006) Diagnosis and treatment of low back pain. BMJ. 332(7555):1430–1434
Liu S, Wang B, Fan S, Wang Y, Zhan Y, Ye D (2022) Global burden of musculoskeletal disorders and attributable factors in 204 countries and territories: a secondary analysis of the Global Burden of Disease 2019 study. BMJ Open 12(6):e062183
Hong JY, Song KS, Cho JH, Lee JH (2017) An updated overview of low back pain management in primary care. Asian Spine J août 11(4):653–660
Gianola S, Bargeri S, Castillo GD, Corbetta D, Turolla A, Andreano A et al (2022) Effectiveness of treatments for acute and subacute mechanical non-specific low back pain: a systematic review with network meta-analysis. Br J Sports Med 56(1):41–50
Tamang M, Dorji T (2021) Physiotherapy services in patient care in Bhutan. Hum Resour Health. 19(1):107
Safiri S, Kolahi AA, Hoy D, Buchbinder R, Mansournia MA, Bettampadi D et al (2017) Global, regional, and national burden of neck pain in the general population, 1990–2017: systematic analysis of the Global Burden of Disease Study. BMJ 368:791
Lewis T, Synowiec C, Lagomarsino G, Schweitzer J (2012) E-health in low- and middle-income countries: findings from the Center for Health Market Innovations. Bull World Health Organ 90(5):332–340
Bashshur R, Shannon G, Krupinski E, Grigsby J (2011) The taxonomy of telemedicine. Telemed J E-Health Off J Am Telemed Assoc 17(6):484–94
Olla P, Shimskey C (2015) mHealth taxonomy: a literature survey of mobile health applications. Health Technol 4:299–308
Larson EC, Goel M, Boriello G, Heltshe S, Rosenfeld M, Patel SN (2012) SpiroSmart: using a microphone to measure lung function on a mobile phone. In: Proceedings of the 2012 ACM Conference on Ubiquitous Computing - UbiComp ’12 [Internet]. Pittsburgh, Pennsylvania: ACM Press; [cité 12 juill 2022]. p. 280. Disponible sur: http://dl.acm.org/citation.cfm?doid=2370216.2370261
Tapley A, Switz N, Reber C, Davis JL, Miller C, Matovu JB et al (2013) Mobile digital fluorescence microscopy for diagnosis of tuberculosis. J Clin Microbiol juin 51(6):1774–1778
Burke LE, Sereika SM, Bizhanova Z, Parmanto B, Kariuki J, Cheng J et al (2022) The effect of tailored, daily, smartphone feedback to lifestyle self-monitoring on weight loss at 12 Months: the SMARTER randomized clinical trial. J Med Internet Res. 24(7):e38243
Wang J, Coleman DC, Kanter J, Ummer B, Siminerio L (2018) Connecting smartphone and wearable fitness tracker data with a nationally used electronic health record system for diabetes education to facilitate behavioral goal monitoring in diabetes care: protocol for a pragmatic multi-site randomized trial. JMIR Res Protoc. 7(4):10009
Wintergerst MWM, Jansen LG, Holz FG, Finger RP (2020) A novel device for smartphone-based fundus imaging and documentation in clinical practice: comparative image analysis study. JMIR MHealth UHealth 8(7):e17480
Kim Y, Oh J, Choi SH, Jung A, Lee JG, Lee YS et al (2021) A portable smartphone-based laryngoscope system for high-speed vocal cord imaging of patients with throat disorders: instrument validation study. JMIR MHealth UHealth 9(6):e25816
Bhavnani SP, Narula J, Sengupta PP (2016) Mobile technology and the digitization of healthcare. Eur Heart J 37(18):1428
Marcolino MS, Oliveira JAQ, D’Agostino M, Ribeiro AL, Alkmim MBM, Novillo-Ortiz D (2018) The impact of mhealth interventions: systematic review of systematic reviews. JMIR MHealth UHealth 6(1):e23
Flores Mateo G, Granado-Font E, Ferré-Grau C, Montaña-Carreras X (2015) Mobile phone apps to promote weight loss and increase physical activity: a systematic review and meta-analysis. J Med Internet Res. 17(11):253
Timmers T, Janssen L, Pronk Y, van der Zwaard BC, Koëter S, van Oostveen D et al (2018) Assessing the efficacy of an educational smartphone or tablet app with subdivided and interactive content to increase patients’ medical knowledge: randomized controlled trial. JMIR MHealth UHealth 6(12):e10742
Linardon J, Cuijpers P, Carlbring P, Messer M, Fuller-Tyszkiewicz M (2019) The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry 18(3):325–336
Pérez-Jover V, Sala-González M, Guilabert M, Mira JJ (2019) Mobile apps for increasing treatment adherence: systematic review. J Med Internet Res 21(6):e12505
Rowland SP, Fitzgerald JE, Holme T, Powell J, McGregor A (2020) What is the clinical value of mHealth for patients? NPJ Digit Med 3:4
Machado GC, Pinheiro MB, Lee H, Ahmed OH, Hendrick P, Williams C et al (2016) Smartphone apps for the self-management of low back pain: a systematic review. Best Pract Res Clin Rheumatol 30(6):1098–1109
Moman RN, Dvorkin J, Pollard EM, Wanderman R, Murad MH, Warner DO et al (2019) A systematic review and meta-analysis of unguided electronic and mobile health technologies for chronic pain-is it time to start prescribing electronic health applications? Pain Med Malden Mass 20(11):2238–2255
Du S, Liu W, Cai S, Hu Y, Dong J (2020) The efficacy of e-health in the self-management of chronic low back pain: a meta analysis. Int J Nurs Stud 106:103507
Chen M, Wu T, Lv M, Chen C, Fang Z, Zeng Z et al (2021) Efficacy of mobile health in patients with low back pain: systematic review and meta-analysis of randomized controlled trials. JMIR MHealth UHealth 9(6):e26095
Rintala A, Rantalainen R, Kaksonen A, Luomajoki H, Kauranen K (2022) mHealth apps for low back pain self-management: scoping review. JMIR MHealth UHealth 10(8):e39682
Shukla R, Kapur A (2022) Methods and lessons from costing a large mhealth intervention at scale in India. Front Public Health 10:894390
Bonnechère B, Kossi O, Mapinduzi J, Panda J, Rintala A, Guidetti S et al (2023) Mobile health solutions: an opportunity for rehabilitation in low- and middle income countries? Front Public Health 10:1072322
Local production [Internet]. [cité 12 sept 2022]. Disponible sur: https://www.who.int/teams/health-product-policy-and-standards/assistive-and-medical-technology/medical-devices/local-production
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M (2003) Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 83(8):713–721
de Morton NA (2009) The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 55(2):129–133
Cashin AG, McAuley JH (2020) Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J Physiother 66(1):59
Israel S (2016) How social policies can improve financial accessibility of healthcare: a multi-level analysis of unmet medical need in European countries. Int J Equity Health 15(1):41
Fritzell J, Rehnberg J, Bacchus Hertzman J, Blomgren J (2015) Absolute or relative? A comparative analysis of the relationship between poverty and mortality. Int J Public Health 60(1):101–110
Willcox M, Moorthy A, Mohan D, Romano K, Hutchful D, Mehl G et al (2019) Mobile technology for community health in ghana: is maternal messaging and provider use of technology cost-effective in improving maternal and child health outcomes at scale? J Med Internet Res 21(2):e11268
Delamater PL, Messina JP, Shortridge AM, Grady SC (2012) Measuring geographic access to health care: raster and network-based methods. Int J Health Geogr 11(1):15
AccessMod: geographic access to health care [Internet]. [cité 6 sept 2022]. Disponible sur: https://www.who.int/tools/accessmod-geographic-access-to-health-care
Mobile data prices fall across low and middle income countries [Internet]. Alliance for Affordable Internet. 2019 [cité 5 sept 2022]. Disponible sur: https://a4ai.org/news/mobile-data-prices-fall-across-low-and-middle-income-countries/
McCormick D. What is an Offline App and Why Are Offline Apps Important? [Internet]. [cité 5 sept 2022]. Disponible sur: https://www.alphasoftware.com/blog/offline-apps
Ransing R, Vadivel R, Halabi SE, Jatchavala C, Shalbafan M, Noël C et al (2021) Language as multi-level barrier in health research and the way forward. Indian J Psychol Med. https://doi.org/10.1177/02537176211052071
Smith-Greenaway E (2015) Educational attainment and adult literacy: a descriptive account of 31 Sub-Saharan Africa countries. Demogr Res 11(33):1015–1034
Veroniki AA, Jackson D, Viechtbauer W, Bender R, Bowden J, Knapp G et al (2016) Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res Synth Methods 7(1):55–79
Carter EC, Schönbrodt FD, Gervais WM, Hilgard J (2019) Correcting for bias in psychology: a comparison of meta-analytic methods. Adv Methods Pract Psychol Sci 2(2):115–44
Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J et al (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002
Pustejovsky JE, Rodgers MA (2019) Testing for funnel plot asymmetry of standardized mean differences. Res Synth Methods mars 10(1):57–71
Peter K, Robert L, Terry H (2015) The effect of changing movement and posture using motion-sensor biofeedback, versus guidelines-based care, on the clinical outcomes of people with sub-acute or chronic low back pain-a multicentre, cluster-randomised, placebo-controlled, pilot trial. BMC Musculoskelet Disord mai 16:131
Itoh N, Mishima H, Yoshida Y, Yoshida M, Oka H, Matsudaira K (2022) Evaluation of the Effect of Patient Education and Strengthening Exercise Therapy Using a Mobile Messaging App on Work Productivity in Japanese Patients with Chronic Low Back Pain: Open-Label, Randomized, Parallel-Group Trial. JMIR MHealth UHealth [Internet]. 10(5). Disponible sur: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85130048622&doi=10.2196%2f35867&partnerID=40&md5=04a1e0d90cd92f35dd93ca4bb02b7ec3
Toelle TR, Utpadel-Fischler DA, Haas KK, Priebe JA (2019) App-based multidisciplinary back pain treatment versus combined physiotherapy plus online education: a randomized controlled trial. NPJ Digit Med 2:34
Bernardelli G, Vigna L, Nava C, De Gennaro CV, Andersen LL, Consonni D et al (2020) Physical activity in healthcare workers with low back pain: effects of the back-fit randomized trial. J Occup Environ Med juin 62(6):e245–e249
Chhabra HS, Sharma S, Verma S (2018) Smartphone app in self-management of chronic low back pain: a randomized controlled trial. Eur Spine J 27(11):2862–2874
Hagiwara Y, Yabe Y, Yamada H, Watanabe T, Kanazawa K, Koide M et al (2017) Effects of a wearable type lumbosacral support for low back pain among hospital workers: a randomized controlled trial. J Occup Health 59(2):201–209
Koppenaal T, Pisters MF, Kloek CJ, Arensman RM, Ostelo RW, Veenhof C (2022) The 3-month effectiveness of a stratified blended physiotherapy intervention in patients with nonspecific low back pain: cluster randomized controlled trial. J Med Internet Res. 24(2):e31675
Sitges C, Terrasa JL, García-Dopico N, Segur-Ferrer J, Velasco-Roldán O, Crespí-Palmer J, et al. (2022) An Educational and Exercise Mobile Phone-Based Intervention to Elicit Electrophysiological Changes and to Improve Psychological Functioning in Adults With Nonspecific Chronic Low Back Pain (BackFit App): Nonrandomized Clinical Trial. JMIR MHealth UHealth [Internet]. 10(3). Disponible sur: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85126446350&doi=10.2196%2f29171&partnerID=40&md5=31354eaee609f09155a0a53eb9bb8506
Sandal LF, Bach K, Øverås CK, Svendsen MJ, Dalager T, Stejnicher Drongstrup Jensen J et al (2021) Effectiveness of app-delivered, tailored self-management support for adults with lower back pain-related disability: a selfback randomized clinical trial. JAMA Intern Med 181(10):1288–1296
Zheng F, Zheng Y, Liu S, Yang J, Xiao W, Xiao W et al (2022) The effect of m-health-based core stability exercise combined with self-compassion training for patients with nonspecific chronic low back pain: a randomized controlled pilot study. Pain Ther 11(2):511–528
Zheng F, Liu S, Zhang S, Yu Q, Lo WLA, Li T et al (2022) Does m-health-based exercise (guidance plus education) improve efficacy in patients with chronic low-back pain? A preliminary report on the intervention’s significance. Trials 23(1):1903
Pach D, Blödt S, Wang J, Keller T, Bergmann B, Rogge AA et al (2022) App-based relaxation exercises for patients with chronic neck pain: pragmatic randomized trial. JMIR MHealth UHealth 10(1):e31482
Petrozzi MJ, Leaver A, Ferreira PH, Rubinstein SM, Jones MK, Mackey MG (2019) Addition of MoodGYM to physical treatments for chronic low back pain: a randomized controlled trial. Chiropr Man Ther 27:54
Amorim AB, Pappas E, Simic M, Ferreira ML, Jennings M, Tiedemann A et al (2019) Integrating Mobile-health, health coaching, and physical activity to reduce the burden of chronic low back pain trial (IMPACT): a pilot randomised controlled trial. BMC Musculoskelet Disord 20(1):71
Mbada C, Olaoye M, Dada O, Ayanniyi O, Johnson O, Odole A et al (2019) Comparative efficacy of clinic-based and telerehabilitation application of McKenzie therapy in chronic low-back pain. Int J Telerehabilitation 11(1):41–57
Kent P, Laird R, Haines T (2015) The effect of changing movement and posture using motion-sensor biofeedback, versus guidelines-based care, on the clinical outcomes of people with sub-acute or chronic low back pain-a multicentre, cluster-randomised, placebo-controlled, pilot trial. BMC Musculoskelet Disord 16:131
John MP, Andrew L, Paulo HF, Sidney MR, Merwen KJ, Martin GM (2019) Addition of MoodGYM to physical treatments for chronic low back pain: a randomized controlled trial. Chiropr Man Ther 27:54
moodgym CBT training program [Internet]. [cité 22 août 2022]. Disponible sur: https://moodgym.com.au/info/faq
Mutubuki EN, Beljon Y, Maas ET, Huygen FJPM, Ostelo RWJG, van Tulder MW et al (2020) The longitudinal relationships between pain severity and disability versus health-related quality of life and costs among chronic low back pain patients. Qual Life Res 29(1):275–287
Kovacs FM, Abraira V, Zamora J, del Real TGM, Llobera J, Fernández C et al (2004) Correlation between pain, disability, and quality of life in patients with common low back pain. Spine 29(2):206–210
Matheve T, Brumagne S, Demoulin C, Timmermans A (2018) Sensor-based postural feedback is more effective than conventional feedback to improve lumbopelvic movement control in patients with chronic low back pain: a randomised controlled trial. J Neuroengineering Rehabil 15(1):85
Africa’s most affordable mobile internet is in Algeria [Internet]. Quartz. 2022 [cité 5 janv 2023]. Disponible sur: https://qz.com/africas-most-affordable-mobile-internet-is-in-algeria-1849586465
Graetz N, Woyczynski L, Wilson KF, Hall JB, Abate KH, Abd-Allah F et al (2020) Mapping disparities in education across low- and middle-income countries. Nature 577(7789):235–238
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mitchaï, P.M., Mapinduzi, J., Verbrugghe, J. et al. Mobile technologies for rehabilitation in non-specific spinal disorders: a systematic review of the efficacy and potential for implementation in low- and middle-income countries. Eur Spine J 32, 4077–4100 (2023). https://doi.org/10.1007/s00586-023-07964-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07964-2