Abstract
Purpose
Predicting urinary retention is difficult. The aim of this study is to prospectively validate a previously developed model using machine learning techniques.
Methods
Patients were recruited from pre-operative clinic. Prediction of urinary retention was completed pre-operatively by 4 individuals and compared to ground truth POUR outcomes. Inter-rater reliability was calculated with intercorrelation coefficient (2,1).
Results
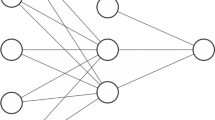
171 patients were included with age 63 ± 14 years, 58.5% (100/171) male, BMI 30.4 ± 5.9 kg/m2, American Society of Anesthesiologists class 2.6 ± 0.5, 1.7 ± 1.0 levels, 56% (96/171) fusions. The observed rate of POUR was 25.7%. The model’s performance was found to be 0.663 (0.567–0.759). With a regression model probability cutoff of 0.24 and a neural network cutoff of 0.23, the following predictive power was achieved: specificity 90.6%, sensitivity 22.7%, negative predictive value 77.2%, positive predictive value 45.5%, and accuracy 73.1%. Intercorrelation coefficient for the regression aspect of the model was found to be 0.889 and intercorrelation coefficient for the neural network aspect of the model was found to be 0.874.
Conclusions
This prospective study confirms performance of the prediction model for POUR developed with retrospective data, showing great correlation. This supports the use of machine learning techniques in the prediction of postoperative complications such as urinary retention.


Similar content being viewed by others
Abbreviations
- ASA:
-
American society of anesthesiologists
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- LOS:
-
Length of stay
- NPV:
-
Negative predictive value
- POUR:
-
Postoperative urinary retention
- PPV:
-
Positive predictive value
References
Swann MC, Hoes KS, Aoun SG, McDonagh DL (2016) Postoperative complications of spine surgery. Best Pract Res Clin Anaesthesiol 30(1):103–120. https://doi.org/10.1016/j.bpa.2016.01.002
Altschul D, Kobets A, Nakhla J et al (2017) Postoperative urinary retention in patients undergoing elective spinal surgery. J Neurosurg Spine 26(2):229–234. https://doi.org/10.3171/2016.8.SPINE151371
Baldini G, Bagry H, Aprikian A, Carli F (2009) Postoperative urinary retention: anesthetic and perioperative considerations. Anesthesiology 110(5):1139–1157. https://doi.org/10.1097/ALN.0b013e31819f7aea
Strickland AR, Usmani MF, Camacho JE et al (2021) Evaluation of risk factors for postoperative urinary retention in elective thoracolumbar spinal fusion patients. Global Spine J 11(3):338–344. https://doi.org/10.1177/2192568220904681
Grass F, Slieker J, Frauche P et al (2017) Postoperative urinary retention in colorectal surgery within an enhanced recovery pathway. J Surg Res 207:70–76. https://doi.org/10.1016/j.jss.2016.08.089
Boulis NM, Mian FS, Rodriguez D, Cho E, Hoff JT (2001) Urinary retention following routine neurosurgical spine procedures. Surg Neurol 55(1):23–27. https://doi.org/10.1016/s0090-3019(01)00331-7
Balderi T, Mistraletti G, D’Angelo E, Carli F (2011) Incidence of postoperative urinary retention (POUR) after joint arthroplasty and management using ultrasound-guided bladder catheterization. Minerva Anestesiol 77(11):1050–1057
Cremins M, Vellanky S, McCann G, Mancini M, Sanzari L, Yannopoulos A (2020) Considering healthcare value and associated risk factors with postoperative urinary retention after elective laminectomy. Spine J 20(5):701–707. https://doi.org/10.1016/j.spinee.2020.01.012
Garg D, Agarwal A (2020) Comment on “Early presentation of urinary retention in multiple system atrophy: can the disease begin in the sacral spinal cord?” J Neurol 267(3):665. https://doi.org/10.1007/s00415-019-09659-5
Agrawal K, Majhi S, Garg R (2019) Post-operative urinary retention: review of literature. World J Anesthesiol. 8(1):1–12. https://doi.org/10.5313/wja.v8.i1.1
Golubovsky JL, Ilyas H, Chen J, Tanenbaum JE, Mroz TE, Steinmetz MP (2018) Risk factors and associated complications for postoperative urinary retention after lumbar surgery for lumbar spinal stenosis. Spine J 18(9):1533–1539. https://doi.org/10.1016/j.spinee.2018.01.022
Sullivan NM, Sutter VL, Mims MM, Marsh VH, Finegold SM (1973) Clinical aspects of bacteremia after manipulation of the genitourinary tract. J Infect Dis 127(1):49–55. https://doi.org/10.1093/infdis/127.1.49
Estimating the additional hospital inpatient cost and mortality associated with selected hospital-acquired conditions. Agency for Health Research and Quality. https://www.ahrq.gov/hai/pfp/haccost2017-results.html. Accessed 14 Oct 2020
Porche K, Maciel CB, Lucke-Wold B et al (2022) Preoperative prediction of postoperative urinary retention in lumbar surgery: a comparison of regression to multilayer neural network. J Neurosurg Spine 36(1):32–41. https://doi.org/10.3171/2021.3.SPINE21189
Brier GW (1950) Verification of forecasts expressed in terms of probability. Monthly Weather Rev 78:1–3
McGraw KO, Wong SP (1996) Forming inferences about some intraclass correlation coefficients. Psychol Methods 1:30–46. https://doi.org/10.1037/1082-989X.1.1.3018
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Porche K, Samra R, Melnick K et al (2022) Enhanced recovery after surgery (ERAS) for open transforaminal lumbar interbody fusion: a retrospective propensity-matched cohort study. Spine J 22(3):399–410. https://doi.org/10.1016/j.spinee.2021.10.007
Acknowledgements
None.
Funding
Research reported in this publication was supported by the University of Florida Clinical and Translational Science Institute, which is supported in part by the NIH National Center for Advancing Translational Sciences under award number UL1TR001427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Porche, K., Maciel, C.B., Lucke-Wold, B. et al. Pre-operative prediction of post-operative urinary retention in lumbar surgery: a prospective validation of machine learning model. Eur Spine J 32, 3868–3874 (2023). https://doi.org/10.1007/s00586-023-07954-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07954-4