Abstract
Purpose
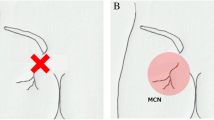
The middle cluneal nerve (MCN) is a pure sensory nerve around the middle buttock. Its entrapment between the iliac crest and the long posterior sacroiliac ligament elicits low back pain (LBP) that can be treated by MCN neurolysis or neurectomy. Because few studies examined the pathology of MCN entrapment (MCN-E) we subjected 7 neurectomized specimens from 6 LBP patients to pathologic study.
Methods
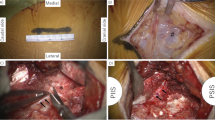
We present 6 consecutive patients (7 sides) with intractable LBP who underwent successful MCN neurectomy. Their symptom duration ranged from 6 to 96 months (average 47.3 months); the follow-up period ranged from 6 to 17 months (average 11.7 months). The surgical outcomes were evaluated using the numerical rating scale (NRS) for LBP and the Roland-Morris Disability Questionnaire (RDQ) score. The resected MCNs underwent neuropathological analysis.
Results
Postoperatively, all 6 patients reported immediate LBP amelioration; their NRS and RDQ scores were improved significantly. Pathological study of the 7 resected nerves showed that the myelinated fiber density was decreased in 6 nerves; we observed marked enlargement (n = 5), perineurial thickening and disruption (n = 6), intrafascicular fibrous changes (n = 5), myelinated fibers separated by fibrous cells under the perineurium (n = 4), and Renaut bodies (n = 3). The 7th nerve appeared normal with respect to the density and size of the myelinated fibers, however, the perineurium was slightly thickened.
Conclusion
We present pathological evidence at the MCN compression site of 7 nerves from 6 patients whose LBP was alleviated by MCN neurectomy, indicating that MCN entrapment can elicit LBP.

Similar content being viewed by others
References
Deyo RA, Weinstein JN (2001) Low back pain. N Engl J Med 344:363–370
Ermis MN, Yildirim D, Durakbasa MO, Tamam C, Ermis OE (2011) Medial superior cluneal nerve entrapment neuropathy in military personnel; diagnosis and etiologic factors. J Back Musculoskelet Rehabil 24:137–144
Kuniya H, Aota Y, Kawai T, Kaneko K, Konno T, Saito T (2014) Prospective study of superior cluneal nerve disorder as a potential cause of low back pain and leg symptoms. J Orthop Surg Res 31:139
Maigne JY, Doursounian L (1997) Entrapment neuropathy of the medial superior cluneal nerve. Nineteen cases surgically treated, with a minimum of 2 years’ follow-up. Spine 22:1156–1159
Morimoto D, Isu T, Kim K et al (2013) Surgical treatment of superior cluneal nerve entrapment neuropathy. J Neurosurg Spine 19:71–75
Morimoto D, Isu T, Kim K et al (2017) Long-term outcome of surgical treatment for superior cluneal nerve entrapment neuropathy. Spine 42:783–788
Tubbs RS, Levin MR, Loukas M, Potts EA, Cohen-Gadol AA (2010) Anatomy and landmarks for the superior and middle cluneal nerves: application to posterior iliac crest harvest and entrapment syndromes. J Neurosurg Spine 13:356–359
Kuniya H, Aota Y, Saito T et al (2013) Anatomical study of superior cluneal nerve entrapment. J Neurosurg Spine 19:76–80
Lu J, Ebraheim NA, Huntoon M, Heck BE, Yeasting RA (1998) Anatomic considerations of superior cluneal nerve at posterior iliac crest region. Clin Orthop Relat Res 347:224–228
Kim K, Shimizu J, Isu T et al (2018) Low back pain due to superior cluneal nerve entrapment: a clinicopathologic study. Muscle Nerve 57:777–783
McGrath MC, Zhang M (2005) Lateral branches of dorsal sacral nerve plexus and the long posterior sacroiliac ligament. Surg Radiol Anat 27:327–330
Konno T, Aota Y, Saito T et al (2017) Anatomical study of middle cluneal nerve entrapment. J Pain Res 10:1431–1435
Aota Y (2016) Entrapment of middle cluneal nerves as an unknown cause of low back pain. World J Orthop 7:167–170
Fujihara F, Isu T, Kim K et al (2021) Clinical features of middle cluneal nerve entrapment neuropathy. Acta Neurochir 163:817–822
Fujihara F, Kim K, Kokubo R et al (2021) High frequency thermal coagulation therapy for middle cluneal nerve entrapment neuropathy. Acta Neurochir 163:823–828
Kim K, Isu T, Matsumoto J, Yamazaki K, Isobe M (2018) Low back pain due to middle cluneal nerve entrapment neuropathy. Eur Spine J 27:S309-313
Kim K, Kokubo R, Isu T, Morimoto D, Morita A (2022) Patient satisfaction with cluneal nerve entrapment surgery. Acta Neurochir 164:2667–2671
Matsumoto J, Isu T, Kim K, Iwamoto N, Morimoto D, Isobe M (2018) Surgical treatment of middle cluneal nerve entrapment neuropathy: technical note. J Neurosurg Spine 29:208–213
Matsumoto J, Isu T, Kim K, Miki K, Fujihara F, Isobe M (2019) Middle cluneal nerve entrapment mimics sacroiliac joint pain. Acta Neurochir 161:657–661
Fujiwara A, Kobayashi N, Saiki K, Kitagawa T, Tamai K, Saotome K (2003) Association of the Japanese orthopaedic association score with the Oswestry disability index, Roland–Morris disability questionnaire, and short-form 36. Spine 28:1601–1607
Hjermstad MJ, Fayers PM, Haugen DF et al (2011) Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manag 41:1073–1093
Berini SE, Spinner RJ, Jentoft ME et al (2014) Chronic meralgia paresthetica and neurectomy: a clinical pathologic study. Neurology 82:1551–1555
Mackinnon SE, Dellon AL, Hudson AR, Hunter DA (1986) Chronic human nerve compression—a histological assessment. Neuropathol Appl Neurobiol 12:547–565
Neary D, Ochoa J, Gilliatt RW (1975) Subclinical entrapment neuropathy in man. J Neurol Sci 24:283–298
Thomas PK, Fullerton PM (1963) Nerve fibre size in the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry 26:520–527
Funding
The authors have no personal, financial, or institutional interests in any of the drugs, materials, or devices described article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were by KK, JS, TI, DM, and AK. The first draft of the manuscript was written by KK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict of interest to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Chiba Hokuso Hospital, Nippon Medical School (dated May 7, 2021; number B-2020-329).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, K., Shimizu, J., Isu, T. et al. A clinicopathological study of low back pain due to middle cluneal nerve entrapment: case series. Eur Spine J 33, 490–495 (2024). https://doi.org/10.1007/s00586-023-07944-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07944-6