Abstract
Introduction
Despite successful fusion rates with iliac crest bone graft (ICBG), donor-site morbidity and increased operating time remain a considerable limitation and drive the search for alternatives. In this systematic review, grafts with additional cellular supplementation were compared with ICBG for spinal arthrodesis. We compared safety, efficacy and long-term outcomes, thus providing the current and relevant evidence for orthopaedic surgeons to make informed choices regarding this rapidly developing field.
Methods
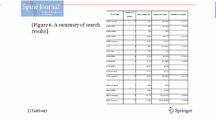
An electronic literature search was conducted according to the PRISMA guidelines by two independent reviewers for articles published up to 1st March 2023 using PubMed, EMBASE and the Cochrane Central Register of Controlled Trial. Cellular allografts were not included. The following data were extracted: Number of patients, type of graft, fusion assessment method, follow-up duration, fusion rates, clinical outcomes and complications. The methodological quality of evidence (MQOE) was assessed using the Risk of Bias 2 (RoB-2) tool and Risk of Bias In Non-Randomised Studies (ROBINS) tool developed by Cochrane for evaluating bias in randomised and non-randomised studies.
Results
Ten studies fulfiled the inclusion criteria, including 465 patients. The mean number of patients per study was 43.8 (std dev. 28.81, range 12–100). Two studies demonstrated cell-based therapy to be significantly more successful in terms of fusion rates compared to ICBG. However, the remaining eight demonstrated equivocal results. No study found that cell-based therapy was inferior. No difference was seen between the two groups in three studies who focused on degenerative cohorts. No difference in functional outcome scores was seen between the groups. A number of different preparation techniques for cell-based grafts were used throughout the studies.
Conclusion
Cell-based therapy offers a promising alternative to ICBG in spinal fusion surgery, which could help reduce the associated morbidity to patients. This review found that cell-based therapy is non-inferior to iliac crest bone graft and may offer patients an alternative treatment option with fewer complications and reduced post-operative pain. However, the literature to date is limited by heterogeneity of the cell preparation and grafting process. Future research with a unified approach to the cell preparation process is required to fully delineate the potential advantages of this technology.





Similar content being viewed by others
References
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1(1):2
Jancuska JM, Hutzler L, Protopsaltis TS, Bendo JA, Bosco J (2016) Utilization of lumbar spinal fusion in New York State: trends and disparities. Spine 41(19):1508–1514
Souslian FG, Patel PD (2021) Review and analysis of modern lumbar spinal fusion techniques. Br J Neurosurg. https://doi.org/10.1080/02688697.2021.1881041
Ahlmann E, Patzakis M, Roidis N, Shepherd L, Holtom P (2002) Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. JBJS 84(5):716–720
Myeroff C, Archdeacon M (2011) Autogenous bone graft: donor sites and techniques. JBJS 93(23):2227–2236
Robinson BT, Metcalfe D, Cuff AV et al (2018) Surgical techniques for autologous bone harvesting from the iliac crest in adults. Cochrane Database Syst Rev 2018(4):CD011783
Khashan M, Inoue S, Berven SH (2013) Cell-based therapies as compared to autologous bone grafts for spinal arthrodesis. Spine 38(21):1885–1891
Johnstone B, Ryaby J, Zhang N et al (2020) Comparing cellular bone matrices for posterolateral spinal fusion. Bone Jt 102:47–47
Robbins MA, Haudenschild DR, Wegner AM, Klineberg EO (2017) Stem cells in spinal fusion. Global spine journal 7(8):801–810
Vaccaro AR, Stubbs HA, Block JE (2007) Demineralized bone matrix composite grafting for posterolateral spinal fusion. Orthopedics 30(7):567
Hart R, Komzák M, Okál F, Náhlík D, Jajtner P, Puskeiler M (2014) Allograft alone versus allograft with bone marrow concentrate for the healing of the instrumented posterolateral lumbar fusion. Spine J 14(7):1318–1324
Gonzalez-Tartiere P, de Frutos AG, Ubierna MT et al (2019) P136. Randomized, prospective clinical trial to evaluate efficacy and safety in lumbar fusion surgery of implantation of autologous bone marrow mesenchymal cells expanded ex vivo and combined with allogeneic bone tissue, compared with autologous iliac crest graft; part II: clinical findings. Spine J 19(9):S220–S221
Kitchel SH (2006) A preliminary comparative study of radiographic results using mineralized collagen and bone marrow aspirate versus autologous bone in the same patients undergoing posterior lumbar interbody fusion with instrumented posterolateral lumbar fusion. Spine J 6(4):405–411
Niu C-C, Tsai T-T, Fu T-S, Lai P-L, Chen L-H, Chen W-J (2009) A comparison of posterolateral lumbar fusion comparing autograft, autogenous laminectomy bone with bone marrow aspirate, and calcium sulphate with bone marrow aspirate: a prospective randomized study. LWW
Moro-Barrero L, Acebal-Cortina G, Suárez-Suárez M, Pérez-Redondo J, Murcia-Mazón A, López-Muñiz A (2007) Radiographic analysis of fusion mass using fresh autologous bone marrow with ceramic composites as an alternative to autologous bone graft. Clin Spine Surg 20(6):409–415
Sterne JA, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. https://doi.org/10.1136/bmj.l4898
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. https://doi.org/10.1136/bmj.i4919
Dryer RF, Pettine KA, Ghiselli G, Bae HW (2013) Study comparing mesenchymal precursor cells and autogenous iliac crest bone graft for lumbar interbody fusion in a randomized controlled phase 2 FDA clinical trial. Spine J 13(9):S30
Chotivichit A, Ruangchainikom M, Tongdee T, Wongkajornsilp A, Permpikul P, Korwutthikulrangsri E (2016) A prospective randomized controlled trial comparing posterolateral lumbar fusion with and without bone marrow concentrate augmentation in single-level lumbar spondylolisthesis. J Med Assoc Thail 99(10):1073–1079
Neen D, Noyes D, Shaw M, Gwilym S, Fairlie N, Birch N (2006) Healos and bone marrow aspirate used for lumbar spine fusion: a case controlled study comparing healos with autograft. Spine 31(18):E636–E640
Bansal S, Chauhan V, Sharma S, Maheshwari R, Juyal A, Raghuvanshi S (2009) Evaluation of hydroxyapatite and beta-tricalcium phosphate mixed with bone marrow aspirate as a bone graft substitute for posterolateral spinal fusion. Indian J Orthop 43(3):234
Banwart JC, Asher MA, Hassanein RS (1995) Iliac crest bone graft harvest donor site morbidity. A Stat Eval Spine 20(9):1055–1060
Merritt AL, Spinnicke A, Pettigrew K, Alamin TF (2010) Gluteal-sparing approach for posterior iliac crest bone graft: description of a new technique and assessment of morbidity in ninety-two patients after spinal fusion. Spine 35(14):1396–1400
Zhu J-F, Xu W-X, Hu Q, Wu T-Q, Liu H (2020) Iliac bone harvesting techniques for bone reconstruction: comparative study between tricortical bone harvesting versus trapdoor technique. Ther Clin Risk Manag 16:559
Dawson J, Kiner D, Warren Gardner I, Swafford R, Nowotarski PJ (2014) The reamer–irrigator–aspirator as a device for harvesting bone graft compared with iliac crest bone graft: union rates and complications. J Orthop Trauma 28(10):584–590
Lehr AM, Oner FC, Hoebink EA et al (2019) Patients cannot reliably distinguish the iliac crest bone graft donor site from the contralateral side after lumbar spine fusion: a patient-blinded randomized controlled trial. Spine 44(8):527–533
Snavely JE, Mercer RW, Stewart G (2019) Harvest of Iliac crest autograft not associated with localized pain. Int J Spine Surg 13(3):275–282
Sheha ED, Meredith DS, Shifflett GD et al (2018) Postoperative pain following posterior iliac crest bone graft harvesting in spine surgery: a prospective, randomized trial. Spine J 18(6):986–992
Edwards R, Gibson J, Mungin-Jenkins E, Pickford R, Lucas JD, Jones GD (2022) A preoperative spinal education intervention for spinal fusion surgery designed using the rehabilitation treatment specification system is safe and could reduce hospital length of stay, normalize expectations, and reduce anxiety: a prospective cohort study. Bone Jt Open 3(2):135
Sipp D, Robey PG, Turner L (2018) Clear up this stem-cell mess. Nature Publishing Group, London
van der Stok J, Hartholt K, Schoenmakers D, Arts J (2017) The available evidence on demineralised bone matrix in trauma and orthopaedic surgery: a systematic review. Bone Jt Res 6(7):423–432
Ruan T, Naveed M, Vien H (2023) Case report: tuberculosis recall on bone graft patient. North Am Spine Soc J 15:100241
Fu R, Selph S, McDonagh M et al (2013) Effectiveness and harms of recombinant human bone morphogenetic protein-2 in spine fusion: a systematic review and meta-analysis. Ann Intern Med 158(12):890–902
Jacobsen MK, Andresen AK, Jespersen AB et al (2020) Randomized double blind clinical trial of ABM/P-15 versus allograft in noninstrumented lumbar fusion surgery. Spine J 20(5):677–684
Arnold PM, Sasso RC, Janssen ME et al (2018) i-Factor™ bone graft versus autograft in anterior cervical discectomy and fusion: 2-year follow-up of the randomized single-blinded food and drug administration investigational device exemption study. Neurosurgery 83(3):377–384
Gibbons D, Welch-Phillips A, Ahern DP, Butler JS (2020) Advantages and design of PROMIS questionnaires. Clin Spine Surg 33(10):408–410
Ambrosi TH, Longaker MT, Chan CK (2019) A revised perspective of skeletal stem cell biology. Front Cell Dev Biol 7:189
de Frutos AG, González-Tartière P, Bonet RC et al (2020) Randomized clinical trial: expanded autologous bone marrow mesenchymal cells combined with allogeneic bone tissue, compared with autologous iliac crest graft in lumbar fusion surgery. Spine J 20(12):1899–1910
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gordon, A., Newsome, F., Ahern, D.P. et al. Iliac crest bone graft versus cell-based grafts to augment spinal fusion: a systematic review and meta-analysis. Eur Spine J 33, 253–263 (2024). https://doi.org/10.1007/s00586-023-07941-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07941-9