Abstract
Purpose
The aim of this study was to determine whether the presence of abdominal aortic calcification (AAC) can predict patient bone status, represented by volumetric bone mineral density (vBMD) assessed with quantitative computed tomography (QCT).
Methods
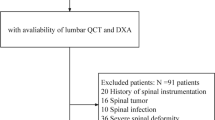
Patients undergoing lumbar fusion surgery at a tertiary care center between 2014 and 2021, with a preoperative lumbar CT-scan and lateral lumbar radiographs were retrospectively reviewed. A semi-quantitative measurement method for AAC (AAC 4, 8 and 24) was performed. QCT measurements were made for L1 and L2. Patients were divided into two groups depending on whether AAC was present. A one-way analysis of covariance was conducted to adjust for age. A multiple linear regression model was used to test if age, sex, BMI, diabetes, hypertension, smoking and presence of AAC could predict the vBMD. A receiver operating characteristic (ROC) analysis was conducted for predicting impaired bone status.
Results
267 patients with a median age of 65.1 years and BMI of 29.8 kg/m2 were analyzed, 59.6% of patients had AAC. The group comparison showed that vBMD was significantly lower in patients with the presence of AAC (97.8 mg/cm3 vs. 121.5 mg/cm3). Age (β = − 0.360; p < 0.001) and presence of AAC (β = −0.206; p = 0.005) significantly predict vBMD as independent variables. Impaired bone status could be discriminated using AAC 4, 8 and 24 (cut off value 0.5) with a sensitivity of 70.1% and a specificity of 60.2%.
Conclusion
The presence of AAC may identify patients at risk for impaired bone status. Preoperative evaluation of standard lumbar radiographs could be used as a potential diagnostic tool in assessing bone status.





Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Gupta A, Cha T, Schwab J et al (2021) Osteoporosis increases the likelihood of revision surgery following a long spinal fusion for adult spinal deformity. Spine J 21(1):134–140
Lee CK, Choi SK, An SB et al (2021) Influence of osteoporosis following spine surgery on reoperation, readmission, and economic costs: an 8-year nationwide population-based study in Korea. World Neurosurg 149:e360–e368
Bjerke BT, Zarrabian M, Aleem IS et al (2018) Incidence of osteoporosis-related complications following posterior lumbar fusion. Global Spine J 8(6):563–569
Khalid SI, Nunna RS, Maasarani S et al (2020) Association of osteopenia and osteoporosis with higher rates of pseudarthrosis and revision surgery in adult patients undergoing single-level lumbar fusion. Neurosurg Focus 49(2):E6
Weiser L, Huber G, Sellenschloh K et al (2017) Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur Spine J 26(11):2891–2897
Oh KW, Lee JH, Lee JH, Lee DY, Shim HJ (2017) the correlation between cage subsidence, bone mineral density, and clinical results in posterior lumbar interbody fusion. Clin Spine Surg 30(6):E683–E689
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29(17):1938–1944
Lopez Picazo M, Humbert L, Winzenrieth R, Di Gregorio S, Gonzalez Ballester MA, Del Rio Barquero LM (2020) Association between osteoporotic femoral neck fractures and DXA-derived 3D measurements at lumbar spine: a case-control study. Arch Osteoporos 15(1):8
Pasco JA, Sanders KM, Hoekstra FM, Henry MJ, Nicholson GC, Kotowicz MA (2005) The human cost of fracture. Osteoporos Int 16(12):2046–2052
Bouchard R, Woltmann A, Staubach K-H et al (1999) Die mortalität von alten menschen nach hüftgelenksnahen femurfrakturen. Unfallchirurgie 25(3):119–132
Shepherd JA, Schousboe JT, Broy SB, Engelke K, Leslie WD (2015) Executive summary of the 2015 ISCD position development conference on advanced measures from DXA and QCT: fracture prediction beyond BMD. J Clin Densitom 18(3):274–286
Knapp KM, Welsman JR, Hopkins SJ, Fogelman I, Blake GM (2012) Obesity increases precision errors in dual-energy X-ray absorptiometry measurements. J Clin Densitom 15(3):315–319
Guglielmi G, Grimston SK, Fischer KC, Pacifici R (1994) Osteoporosis: diagnosis with lateral and posteroanterior dual x-ray absorptiometry compared with quantitative CT. Radiology 192(3):845–850
Drinka PJ, DeSmet AA, Bauwens SF, Rogot A (1992) The effect of overlying calcification on lumbar bone densitometry. Calcif Tissue Int 50(6):507–510
Li N, Li X, Xu L, Sun W, Cheng X, Tian W (2013) Comparison of QCT and DXA: osteoporosis detection rates in postmenopausal women. Int J Endocrinol 2013:895474
Dagenais S, Caro J, Haldeman S (2008) A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 8(1):8–20
Heliovaara M, Sievers K, Impivaara O et al (1989) Descriptive epidemiology and public health aspects of low back pain. Ann Med 21(5):327–333
Maher C, Underwood M, Buchbinder R (2017) Non-specific low back pain. Lancet 389(10070):736–747
Szulc P, Blackwell T, Kiel DP et al (2015) Abdominal aortic calcification and risk of fracture among older women—the SOF study. Bone 81:16–23
El Maghraoui A, Rezqi A, Mounach A, Achemlal L, Bezza A, Ghozlani I (2012) Relationship between vertebral fracture prevalence and abdominal aortic calcification in men. Rheumatology (Oxford) 51(9):1714–1720
Szulc P, Samelson EJ, Sornay-Rendu E, Chapurlat R, Kiel DP (2013) Severity of aortic calcification is positively associated with vertebral fracture in older men—a densitometry study in the STRAMBO cohort. Osteoporos Int 24(4):1177–1184
Naves M, Rodriguez-Garcia M, Diaz-Lopez JB, Gomez-Alonso C, Cannata-Andia JB (2008) Progression of vascular calcifications is associated with greater bone loss and increased bone fractures. Osteoporos Int 19(8):1161–1166
Kauppila LI, Polak JF, Cupples LA, Hannan MT, Kiel DP, Wilson PW (1997) New indices to classify location, severity and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis 132(2):245–250
Frye MA, Melton LJ 3rd, Bryant SC et al (1992) Osteoporosis and calcification of the aorta. Bone Miner 19(2):185–194
Persy V, D’Haese P (2009) Vascular calcification and bone disease: the calcification paradox. Trends Mol Med 15(9):405–416
Chow JT, Khosla S, Melton LJ 3rd, Atkinson EJ, Camp JJ, Kearns AE (2008) Abdominal aortic calcification, BMD, and bone microstructure: a population-based study. J Bone Miner Res 23(10):1601–1612
Kauppila LI, McAlindon T, Evans S, Wilson PWF, Kiel D, Felson DT (1997) Disc degeneration/back pain and calcification of the abdominal aorta: a 25-year follow-up study in framingham. Spine 22(14):1642–1647. https://doi.org/10.1097/00007632-199707150-00023
Sakaura H, Miwa T, Kuroda Y, Ohwada T (2016) Surgical outcomes after laminoplasty for cervical spondylotic myelopathy in patients with renal dysfunction and/or aortic arch calcification. J Neurosurg Spine 25(4):444–447
Sakaura H, Ikegami D, Fujimori T, Sugiura T, Owaki H, Fuji T (2019) Abdominal aortic calcification is a significant poor prognostic factor for clinical outcomes after decompressive laminotomy for lumbar spinal canal stenosis. Glob Spine J 9(7):724–728
Sakaura H, Ikegami D, Fujimori T, Sugiura T, Mukai Y, Hosono N (2021) Does atherosclerosis have negative impacts on early adjacent segment degeneration after posterior lumbar interbody fusion? Global Spine J 11(5):674–678
Acknowledgements
Dr. Sama reports royalties from Ortho Development, Corp.; private investments for Vestia Ventures MiRUS Investment, LLC, IVY II, LLC, ISPH 3, LLC, and VBros Venture Partners X Centinel Spine; consulting fee from Clariance, Inc., Kuros Biosciences AG, and Medical Device Business Service, Inc.; speaking and teaching arrangements of DePuy Synthes Products, Inc.; membership of scientific advisory board of Clariance, Inc., and Kuros Biosciences AG; and trips/travel of Medical Device Business research support from Spinal Kinetics, Inc., outside the submitted work. Dr. Cammisa reports royalties from NuVasive, Inc. Accelus; private investments for 4WEB Medical/4WEB, Inc., Bonovo Orthopedics, Inc., Healthpoint Capital Partners, LP, ISPH II, LLC, ISPH 3 Holdings, LLC, Ivy Healthcare Capital Partners, LLC, Medical Device Partners II, LLC, Medical Device Partners III, LLC, Orthobond Corporation, Spine Biopharma, LLC, Synexis, LLC, Tissue Differentiation Intelligence, LLC, VBVP VI, LLC, VBVP X, LLC (Centinel) and Woven Orthopedics Technologies; consulting fees from 4WEB Medical/4WEB, Inc., DePuy Synthes Spine, NuVasive, Inc., Spine Biopharma, LLC, and Synexis, LLC, Accelus; membership of scientific advisory board/other office of Healthpoint Capital Partners, LPIVY, Medical Device Partners III, LLC, Orthobond Corporation, Spine Biopharma, LLC, Synexis, LLC, and Woven Orthopedic Technologies; and research support from 4WEB Medical/4WEB, Inc., Mallinckrodt Pharmaceuticals, Camber Spine, and Centinel Spine, outside the submitted work. Dr. Girardi reports royalties from Lanx, Inc., and Ortho Development Corp.; private investments for Centinel Spine, and BCMID; stock ownership of Healthpoint Capital Partners, LP; and consulting fees from NuVasive, Inc., and DePuy Synthes Spine, outside the submitted work. Dr. Hughes reports research support from NuVasive, Inc. and Kuros Biosciences AG; and fellowship support from NuVasive, Inc. and Kuros Biosciences AG, outside the submitted work.
Funding
Research reported in this publication was supported by the National Center for Advancing Translational Science of the National Institute of Health Under Award Number UL1TR002384.
Author information
Authors and Affiliations
Contributions
Conception and design: M. Acquisition of data: M, H. Analysis and interpretation of data: M, H. Drafting the article: M. Critically revising the article: all authors. Preparation of Graphical Content: M, H. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: H. Statistical analysis: M. Administrative/technical/material support: S. Study supervision: H.
Corresponding author
Ethics declarations
Conflict of interest
The Authors declare that there is no conflict of interest regarding this work.
Ethical approval
The investigation was approved by the institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The institutional review board of the Hospital for Special Surgery approved this study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muellner, M., Haffer, H., Chiapparelli, E. et al. Abdominal aortic calcification assessed on standard lateral lumbar radiographs as a screening tool for impaired bone status in spine surgery. Eur Spine J 32, 3030–3038 (2023). https://doi.org/10.1007/s00586-023-07846-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07846-7