Abstract
Introduction
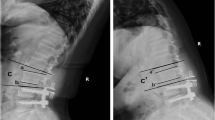
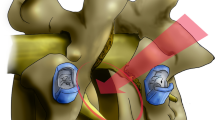
The impact of pre-existing degeneration of a disc underlying a lumbar arthrodesis via lateral approach on long-term clinical outcome has, to our knowledge, not been studied. When performing arthrodesis between L2 and L5, its extension to L5S1 is challenging because it imposes a different surgical approach. Therefore, surgeon’s temptation is to not include L5S1 in the fusion even in case of discopathy. Our objective was to study the influence of the preoperative L5S1 status on the clinical outcome of lumbar lateral interbody fusion (LLIF) using a pre-psoatic approach between L2 and L5 with a minimum follow-up of 2 years.
Material and methods
Patients who underwent LLIF from L2 to L5 between 2015 and 2020 were included in our study. We studied VAS, ODI, and global clinical outcome before surgery and at last follow-up. The L5–S1 disc was radiologically studied in preoperative imaging. Patients were included in two groups (A “with” and B :without” L5–S1 disc degeneration) to compare the clinical outcomes at last follow-up. Our primary objective was to evaluate the rate of L5–S1 disc revision surgery at last follow-up.
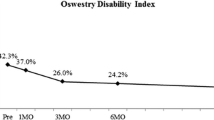
Results
102 patients were included. 2 required L5–S1 disc surgery following overlying arthrodesis. Our results showed a significant improvement in the patients' clinical outcomes at the last follow-up (p < 0.0001). We did not find any significant difference on clinical criteria between groups A & B.
Conclusion
A preop L5S1 disc degeneration does not seem to impact the final clinical outcomes after lumbar lateral interbody fusion at a minimal two years F.U. It should not be systematically involved in an overlying fusion.


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Guigui P, Wodecki P, Bizot P, Lambert P, Chaumeil G, Deburge A (2000) Influence à long terme de l’arthrodèse associée sur les niveaux adjacents dans le traitement des sténoses lombaires [Long-term influence of associated arthrodesis on adjacent segments in the treatment of lumbar stenosis: a series of 127 cases with 9-year follow-up]. Rev Chir Orthop Reparatrice Appar Mot 86(6):546–557
Gillet P (2003) The fate of the adjacent motion segments after lumbar fusion. Spine 28:338–345
Mannion AF, Leivseth G, Brox JI, Fritzell P, Hagg O, Fairbank JC (2014) ISSLS prize winner: long-term follow-up suggests spinal fusion is associated with increased adjacent segment disc degeneration but without influence on clinical outcome: results of a combined follow-up from 4 randomized controlled trials. Spine 39(17):1373–1783
Ghiselli G, Wang JC, Hsu WK, Dawson EG (2003) L5–S1 segment survivorship and clinical outcome analysis after L4–L5 isolated fusion. Spine 28(12):1275–1280
Xia XP, Chen HL, Cheng HB (2013) Prevalence of adjacent segment degeneration after spine surgery: a systematic review and meta-analysis. Spine 38(7):597–608. https://doi.org/10.1097/BRS.0b013e318273a2ea
Wai EK, Santos ERG, Morcom RA, Fraser RD (2006) Magnetic resonance imaging 20 years after anterior lumbar interbody fusion. Spine 31:1952–1956
Min JH, Jang JS, Jung B, Lee HY, Choi WC, Shim CS et al (2008) The clinical characteristics and risk factors for the adjacent segment degeneration in instrumented lumbar fusion. J Spinal Disord Tech 21(5):305–309
Hashimoto K, Aizawa T, Kanno H, Itoi E (2019) Adjacent segment degeneration after fusion spinal surgery: a systematic review. Int Orthop 43:987–993
Pan A, Hai Y, Yang J, Zhou L, Chen X, Guo H (2016) Adjacent segment degeneration after lumbar spinal fusion compared with motion-preservation procedures: a meta-analysis. Eur Spine J 25:1522–1532
Scemama C, Magrino B, Gillet P, Guigui P (2016) Risk of adjacent-segment disease requiring surgery after short lumbar fusion: results of the French Spine surgery society series. J Neurosurg Spine 25:46–51
Miyakoshi N, Abe E, Shimada Y, Okuyama K, Suzuki T, Sato K (2000) Outcome of one-level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine 25:1837–1842
Sears WR, Sergides IG, Kazemi N, Smith M, White GJ, Osburg B (2011) Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J 11(1):11–20
Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y et al (2007) Adjacent segment disease followinglumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine 32(20):2253–2257
Liao JC, Chen WJ, Chen LH, Niu CC (2009) Outcome of the L5–S1 segment after posterior instrumented spinal surgery in degenerative lumbar diseases. Chang Gung Med J 32(1):81–8
Park JY, Chin DK, Cho YE (2009) Accelerated L5–S1 segment degeneration after spinal fusion on and above L4–5: minimum 4-year follow-up results. J Korean Neurosurg Soc 45(2):81–84
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Mag- netic resonance classification of lumbar intervertebral disc degene- ration. Spine 26:1873–1878
Modic MT, Masaryk TJ, Ross JS, Carter JR (1988) Imaging of degenerative disk disease. Radiology 168:177–186. https://doi.org/10.1148/radiology.168.1.3289089
Chao Li, Qing He, Tang Y, Ruan D (2015) The fate of adjacent segments with pre-existing degeneration after lumbar posterolateral fusion: the influence of degenerative grading. Eur Spine J 24:2468–2473. https://doi.org/10.1007/s00586-015-3921-2
Nakashima H, Kawakami N, Tsuji T et al (2015) Adjacent segment disease after posterior lumbar interbody fusion. Spine 40(14):E831–E834. https://doi.org/10.1097/BRS.0000000000000917
Lee CS, Hwang CJ, Lee SW et al (2009) Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J 18(11):1637–1643. https://doi.org/10.1007/s00586-009-1060-3
Lai PL, Chen LH, Niu CC, Fu TS, Chen WJ (2004) Relation between laminectomy and development of adjacent segment instability after lumbar fusion with pedicle fixation. Spine 2004(29):2527–2532. https://doi.org/10.1097/01.brs.0000144408.02918.20
Rothrock RJ, McNeill IT, Yaeger K, Oermann EK, Cho SK, Caridi JM (2018) Lumbar lordosis correction with interbody fusion: systematic literature review and analysis. World Neurosurg 118:21–31. https://doi.org/10.1016/j.wneu.2018.06.216
Pesenti S, Lafage R, Stein D, Elysee JC, Lenke LG, Schwab FJ et al (2018) The amount of proximal lumbar lordosis is related to pelvic incidence. Clin Orthop 476:1603–1611. https://doi.org/10.1097/CORR.0000000000000380
Rothrock RJ, McNeill IT, Yaeger K, Oermann EK, Cho SK, Caridi JM (2018) Lumbar lordosis correction with interbody fusion: systematic literature review and analysis. World Neurosurg 118:21–31. https://doi.org/10.1016/j.wneu.2018.06.216
Liu H, Wu W, Li Y, Liu J, Yang K, Chen Y (2013) Protective effects of preserving the posterior complex on the development of adjacent-segment degeneration after lumbar fusion: clinical article. J Neurosurg Spine 19(2):201–206
Funding
No funding was required for this study.
Author information
Authors and Affiliations
Contributions
JA is the overall study principal investigator. LP, AR, PA, DJ, DT, QS, and JA participated in the study conception and design, contributed to the writing of the study protocol, drafting, and editing of this manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Pr POIGNARD Alexandre, Dr DELAMBRE Jerome and Dr LAVANTES Paul have no relevant financial or non-financial interests to disclose. Dr DUFOUR Thierry is consultant for and has some royalties from ZimVie. Dr QUEINNEC Steffen is consultant for STRYKER compagny and NEO compagny, also shareholder and proxy for the NEO compagny. Dr ARVIEU Robin is consultant for NEO company. Pr ALLAIN Jerome has consultant for STRYKER compagny and NEO company and MEDTRONIC and has some royalties from ZimVie.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lavantes, P., Poignard, A., Delambre, J. et al. Influence of the preoperative L5S1 disc state on lateral L2 to L5 fusion’s outcomes at an average follow-up of 3,5 years (minimum 2 years). Eur Spine J 32, 2344–2349 (2023). https://doi.org/10.1007/s00586-023-07771-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07771-9