Abstract
Purpose
This study aimed to compare the clinical features and postoperative outcomes in patients with Lenke type 5C AIS in the early and late teens.
Methods
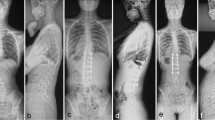
The study included eligible patients with AIS aged < 20 years with Lenke type 5C curves who underwent selective thoracolumbar/lumbar (TL/L) fusion. The patients were divided into two groups according to the age: younger (11–15 years) and older (16–19 years). Demographic data, radiographic parameters, and 22-item scoliosis research society questionnaire (revised) (SRS-22r) scores were compared.
Results
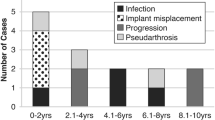
Seventy-three (female: 69, male: 4, mean age: 15.1 years) patients were included. There were 45 and 28 patients in the younger and older groups, respectively. The older group exhibited a significantly smaller TL/L curve than the younger group, whereas no between-group differences were identified regarding curve flexibility and fusion length. The change in coronal balance and subjacent disc angle from preoperative to 2 years after surgery was significantly greater in the younger group, although each curve was equally corrected. Preoperative SRS-22r scores in the older group were significantly worse; however, they improved to the level of the younger group at 2 years after surgery. Postoperative coronal malalignment was observed in six patients (21.4%) in the older group, whereas no cases in the younger group (p < 0.05).
Conclusion
In patients with Lenke type 5C AIS, we showed that late teens had significantly worse SRS-22r scores than did early teens. Postoperative coronal malalignment was frequently observed in the late teens due to the reduced ability of compensation by subjacent disc wedging.



Similar content being viewed by others
References
Hresko MT (2013) Clinical practice. idiopathic scoliosis in adolescents. N Engl J Med 368:834–841. https://doi.org/10.1056/NEJMcp1209063
Peterson LE, Nachemson AL (1995) Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Logistic regression analysis based on data from the brace study of the scoliosis research society. J Bone Joint Surg Am 77:823–827. https://doi.org/10.2106/00004623-199506000-00002
Lonstein JE, Carlson JM (1984) The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am 66:1061–1071
Weinstein SL, Dolan LA, Cheng JCY, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371:1527–1537. https://doi.org/10.1016/S0140-6736(08)60658-3
Weinstein SL (2019) The natural history of adolescent idiopathic scoliosis. J Pediatr Orthop 39:S44-s46. https://doi.org/10.1097/bpo.0000000000001350
Sato T, Hirano T, Ito T, Morita O, Kikuchi R, Endo N, Tanabe N (2011) Back pain in adolescents with idiopathic scoliosis: epidemiological study for 43,630 pupils in Niigata City, Japan. Eur Spine J: Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc 20:274–279. https://doi.org/10.1007/s00586-010-1657-6
Weinstein SL, Zavala DC, Ponseti IV (1981) Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. JBJS 63:1452
Ramirez N, Johnston CE, Browne RH (1997) The prevalence of back pain in children who have idiopathic scoliosis. J Bone Joint Surg Am 79:364–368. https://doi.org/10.2106/00004623-199703000-00007
Fekete TF, Mannion AF, Haschtmann D, Loibl M, Kleinstück FS, Jeszenszky DJ (2019) Back pain and its change after surgery in adolescents and young adults with idiopathic scoliosis. Spine Deform 7:754–758. https://doi.org/10.1016/j.jspd.2019.02.004
Smorgick Y, Mirovsky Y, Baker KC, Gelfer Y, Avisar E, Anekstein Y (2013) Predictors of back pain in adolescent idiopathic scoliosis surgical candidates. J Pediatr Orthop 33:289–292. https://doi.org/10.1097/BPO.0b013e31827d0b43
Zhu F, Bao H, Yan P, Liu S, Zhu Z, Liu Z, Bao M, Qiu Y (2017) Comparison of surgical outcome of adolescent idiopathic scoliosis and young adult idiopathic scoliosis: a match-pair analysis of 160 patients. Spine 42:E1133-e1139. https://doi.org/10.1097/brs.0000000000002106
Deviren V, Berven S, Kleinstueck F, Antinnes J, Smith JA, Hu SS (2002) Predictors of flexibility and pain patterns in thoracolumbar and lumbar idiopathic scoliosis. Spine 27:2346–2349. https://doi.org/10.1097/00007632-200211010-00007
Kurra S, DeMercurio P, Lavelle WF (2022) Comparison of operative implications between adolescent and young adult idiopathic scoliosis patients from scoliosis research society mortality and morbidity database. Spine Deform 10:1133–1138. https://doi.org/10.1007/s43390-022-00515-7
Lavelle W, Kurra S, Hu X, Lieberman I (2020) Clinical outcomes of idiopathic scoliosis surgery: Is there a difference between young adult patients and adolescent patients? Cureus 12:e8118. https://doi.org/10.7759/cureus.8118
Takahashi S, Delécrin J, Passuti N (2002) Surgical treatment of idiopathic scoliosis in adults: an age-related analysis of outcome. Spine 27:1742–1748. https://doi.org/10.1097/00007632-200208150-00011
Lonner BS, Ren Y, Bess S, Kelly M, Kim HJ, Yaszay B, Lafage V, Marks M, Miyanji F, Shaffrey CI, Newton PO (2019) Surgery for the adolescent idiopathic scoliosis patients after skeletal maturity: early versus late surgery. Spine Deform 7:84–92. https://doi.org/10.1016/j.jspd.2018.05.012
Lenke LG, Edwards CCI, Bridwell KH (2003) The lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the Spine. Spine 28:S199–S207. https://doi.org/10.1097/01.brs.0000092216.16155.33
Abel MF, Herndon SK, Sauer LD, Novicoff WM, Smith JS, Shaffrey CI (2011) Spinal deformity study G selective versus nonselective fusion for idiopathic scoliosis: does lumbosacral takeoff angle change? Spine 36:1103–1112. https://doi.org/10.1097/BRS.0b013e3181f60b5b
Senkoylu A, Luk KD, Wong YW, Cheung KM (2014) Prognosis of spontaneous thoracic curve correction after the selective anterior fusion of thoracolumbar/lumbar (Lenke 5C) curves in idiopathic scoliosis. Spine J: Off J North Am Spine Soc 14:1117–1124. https://doi.org/10.1016/j.spinee.2013.07.467
Bridwell KH (1999) Surgical treatment of idiopathic adolescent scoliosis. Spine 24:2607–2616. https://doi.org/10.1097/00007632-199912150-00008
Rushton PR, Grevitt MP (2013) Comparison of untreated adolescent idiopathic scoliosis with normal controls: a review and statistical analysis of the literature. Spine 38:778–785. https://doi.org/10.1097/BRS.0b013e31827db418
Ohashi M, Watanabe K, Hirano T, Hasegawa K, Katsumi K, Shoji H, Mizouchi T, Endo N (2018) Predicting factors at skeletal maturity for curve progression and low back pain in adult patients treated nonoperatively for adolescent idiopathic scoliosis with thoracolumbar/lumbar curves: a mean 25-year follow-up. Spine 43:E1403-e1411. https://doi.org/10.1097/brs.0000000000002716
Pesenti S, Jouve JL, Morin C, Wolff S, Sales de Gauzy J, Chalopin A, Ibnoulkhatib A, Polirsztok E, Walter A, Schuller S, Abelin-Genevois K, Leroux J, Lechevallier J, Kabaj R, Mary P, Fuentes S, Parent H, Garin C, Bin K, Peltier E, Blondel B, Chopin D (2015) Evolution of adolescent idiopathic scoliosis: results of a multicenter study at 20 years’ follow-up. Orthop Traumatol Surg Res OTSR 101:619–622. https://doi.org/10.1016/j.otsr.2015.05.004
Ameri E, Behtash H, Mobini B, Daraie A (2015) Predictors of curve flexibility in adolescent idiopathic scoliosis: a retrospective study of 100 patients. Acta Med Iran 53:182–185
Baroncini A, Trobisch PD, Berjano P, Lamartina C, Kobbe P, Tingart M, Migliorini F (2021) Correlation between age, coronal and sagittal parameters and spine flexibility in patients with adolescent idiopathic scoliosis. Spine Deform 9:1525–1531. https://doi.org/10.1007/s43390-021-00373-9
Landman Z, Oswald T, Sanders J, Diab M (2011) Prevalence and predictors of pain in surgical treatment of adolescent idiopathic scoliosis. Spine 36:825–829. https://doi.org/10.1097/BRS.0b013e3181de8c2b
Puno RM, An KC, Puno RL, Jacob A, Chung SS (2003) Treatment recommendations for idiopathic scoliosis: an assessment of the Lenke classification. Spine 28:2102–2114. https://doi.org/10.1097/01.brs.0000088480.08179.35
Anari JB, LaValva SM, Flynn JM, Tatad AM (2020) Severe persistent coronal imbalance following instrumented posterior spinal fusion for adolescent idiopathic scoliosis. Spine Deform 8:1295–1304. https://doi.org/10.1007/s43390-020-00153-x
Hwang CJ, Lee CS, Kim H, Lee DH, Cho JH (2018) Spontaneous correction of coronal imbalance after selective thoracolumbar-lumbar fusion in patients with Lenke-5C adolescent idiopathic scoliosis. Spine J Off J North Am Spine Soc 18:1822–1828. https://doi.org/10.1016/j.spinee.2018.03.013
Sun Z, Qiu G, Zhao Y, Guo S, Wang Y, Zhang J, Shen J, Zhao H (2014) The effect of unfused segments in coronal balance reconstitution after posterior selective thoracolumbar/lumbar fusion in adolescent idiopathic scoliosis. Spine 39:2042–2048. https://doi.org/10.1097/brs.0000000000000602
Banno T, Yamato Y, Oba H, Ohba T, Hasegawa T, Yoshida G, Arima H, Oe S, Mihara Y, Ushirozako H, Takahashi J, Haro H, Matsuyama Y (2021) Preoperative thoracic curve magnitude and L4 end vertebra were risk factors for subjacent disc wedging after selective thoracolumbar/lumbar fusion with L3 as the lowest instrumented vertebra in lenke type 5 curve patients. Spine. https://doi.org/10.1097/brs.0000000000003961
Yang C, Zhao Y, Zhai X, Li J, Zhu X, Li M (2017) Coronal balance in idiopathic scoliosis: a radiological study after posterior fusion of thoracolumbar/lumbar curves (Lenke 5 or 6). Eur Spine J: Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc 26:1775–1781. https://doi.org/10.1007/s00586-016-4844-2
Mannem A, Cheung PWH, Kawasaki S, Shigematsu H, Cheung JPY (2021) What determines immediate postoperative coronal balance and delayed global coronal balance after anterior spinal fusion for Lenke 5C curves? Eur Spine J: Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc 30:2007–2019. https://doi.org/10.1007/s00586-021-06807-2
Shetty AP, Suresh S, Aiyer SN, Kanna R, Rajasekaran S (2017) Radiological factors affecting post-operative global coronal balance in Lenke 5 C scoliosis. J Spine Surg 3:541–547. https://doi.org/10.21037/jss.2017.09.04
Yang X, Hu B, Song Y, Liu L, Zhou C, Zhou Z, Feng G (2018) Coronal and sagittal balance in Lenke 5 AIS patients following posterior fusion: important role of the lowest instrument vertebrae selection. BMC Musculoskelet Disord 19:212. https://doi.org/10.1186/s12891-018-2135-2
Hu B, Yang X, Yang H, Liu L, Chen P, Wang L, Zhu C, Zhou C, Song Y (2018) Coronal imbalance in Lenke 5C adolescent idiopathic scoliosis regarding selecting the lowest instrumented vertebra: lower end vertebra versus lower end vertebra +1 in posterior fusion. World Neurosurg 117:e522–e529. https://doi.org/10.1016/j.wneu.2018.06.070
Chen K, Bai J, Yang Y, Shao J, Yang M, Zhao J, Yang C, Li M (2019) Immediate postoperative coronal imbalance in Lenke 5 and Lenke 6 adolescent idiopathic scoliosis: Is it predictable? Eur Spine J: Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sec Cerv Spine Res Soc 28:2042–2052. https://doi.org/10.1007/s00586-019-06019-9
Acknowledgements
The authors would like to thank Ms. Nao Kuwahara, Ms. Tomoe Mabuchi, and Mr. Taku Nagao, secretaries of department of Orthopedic Surgery, for their excellence in technical assistance during data collection.
Funding
Donated Fund Laboratory (Division of Geriatric Musculoskeletal Health, Hamamatsu University School of Medicine, Shizuoka, Japan). Meitoku medical institute Jyuzen memorial hospital, Shizuoka, Japan. Japan Medical Dynamic Marketing Inc, Tokyo, Japan. Medtronic Sofamor Danek Inc., Memphis, United States.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have nothing to disclose.
Ethical approval
This study design was approved by the appropriate ethics review boards in Hamamatsu University School of Medicine (IRB No. 19–305). The manuscript submitted does not contain information about medical device(s)/drug(s).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Banno, T., Yamato, Y., Oba, H. et al. Clinical differences in preoperative symptoms and surgical outcomes between early and late-teen patients with Lenke type 5C adolescent idiopathic scoliosis. Eur Spine J 32, 2541–2549 (2023). https://doi.org/10.1007/s00586-023-07758-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07758-6