Abstract
Purpose
Lumbar spinal fusion surgery (LSFS) is common for lumbar degenerative disorders. The objective was to develop clinical prediction rules to identify which patients are likely to have a favourable outcome to inform decisions regarding surgery and rehabilitation.
Methods
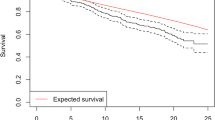
A prospective observational study recruited 600 (derivation) and 600 (internal validation) consecutive adult patients undergoing LSFS for degenerative lumbar disorder through the British Spine Registry. Definition of good outcome (6 weeks, 12 months) was reduction in pain intensity (Numerical Rating Scale, 0–10) and disability (Oswestry Disability Index, ODI 0–50) > 1.7 and 14.3, respectively. Linear and logistic regression models were fitted and regression coefficients, Odds ratios and 95% CIs reported.
Results
Lower BMI, higher ODI and higher leg pain pre-operatively were predictive of good disability outcome, higher back pain was predictive of good back pain outcome, and no previous surgery and higher leg pain were predictive of good leg pain outcome; all at 6 weeks. Working and higher leg pain were predictive of good ODI and leg pain outcomes, higher back pain was predictive of good back pain outcome, and higher leg pain was predictive of good leg pain outcome at 12 months. Model performance demonstrated reasonable to good calibration and adequate/very good discrimination.
Conclusions
BMI, ODI, leg and back pain and previous surgery are important considerations pre-operatively to inform decisions for surgery. Pre-operative leg and back pain and work status are important considerations to inform decisions for management following surgery. Findings may inform clinical decision making regarding LSFS and associated rehabilitation.



Similar content being viewed by others
References
Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA, Maher CG (2018) Prevention and treatment of low back pain: evidence, challenges and promising directions. Lancet 391(10137):2368–2383
Rubin DI (2007) Epidemiology and risk factors for spine pain. Neurol Clin 25(2):353–371
Provaggi E, Capelli C, Leong JJH, Kalaskar DM (2018) A UK—based pilot study of current surgical practice and implant preferences in lumbar fusion surgery. Medicine (Baltimore) 97(26):e11169
Audrey J, Weiss AE (2014) Trends in operating room procedures in U.S. hospitals. 2001–2011. Agency for Healthcare Research and Quality, Rockville
Kaiser MG, Eck JC, Groff MW, Watters WC, Dailey AT, Resnick DK, Choudhri TF, Sharan A, Wang JC, Mummaneni PV, Dhall SS (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 1: introduction and methodology. J Neurosurg Spine 21(1):2–6
National Institute of Clinical Excellence (NICE) (2016) Low back pain and sciatica in over 16s: assessment and management, NICE guideline [NG59]: National Institute for Health and Care Excellence
The Health and Social Care Information Centre. HES online. Admitted Patient Care, Total procedures interventions: 3-character tables (2004–2005, 2014–2015). Available from: http://www.hesonline.nhs.uk. Accessed 29th March 2019
Gibson JN, Waddell G (2005) Surgery for degenerative lumbar spondylosis: updated Cochrane Review. Spine 30(20):2312–2320
Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES (2006) United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine 31(23):2707–2714
Willems P, de Bie R, Oner C, Castelein R, de Kleuver M (2011) Clinical decision making in spinal fusion for chronic low back pain. Results of a nationwide survey among spine surgeons. BMJ Open 1:e000391
Rushton A, White L, Heap A, Heneghan N (2015) Survey of current surgeon practice for patients undergoing lumbar spinal fusion in the UK. World J Orthop 6(6):483–490
Khor S, Lavallee D, Cizik AM, Bellabarba C, Chapman JR, Howe CR, Lu D, Mohit AA, Oskouian RJ, Roh JR, Shonnard N (2018) Development and validation of a prediction model for pain and functional outcomes after lumbar spine surgery. JAMA Surg 153(7):634–642
Janssen ER, Punt IM, van Kuijk SM, Hoebink EA, van Meeteren NL, Willems PC (2020) Development and validation of a prediction tool for pain reduction in adult patients undergoing elective lumbar spinal fusion: a multicentre cohort study. Eur Spine J 29(8):1909–1916
Quddusi A, Eversdijk HA, Klukowska AM, de Wispelaere MP, Kernbach JM, Schröder ML, Staartjes VE (2020) External validation of a prediction model for pain and functional outcome after elective lumbar spinal fusion. Eur Spine J 29(2):374–383
Staartjes VE, Stumpo V, Ricciardi L, Maldaner N, Eversdijk HA, Vieli M, Ciobanu-Caraus O, Raco A, Miscusi M, Perna A, Proietti L (2022) FUSE-ML: development and external validation of a clinical prediction model for mid-term outcomes after lumbar spinal fusion for degenerative disease. Eur Spine J 21:1
Rushton AB, Verra ML, Emms A, Heneghan NR, Falla D, Reddington M, Cole AA, Willems P, Benneker L, Selvey D, Hutton M, Heymans MW, Staal JB (2018) Development of two clinical prediction models to inform clinical decision-making for lumbar spinal fusion surgery for degenerative disorders and rehabilitation following surgery: protocol for a prospective observational study. BMJ Open 8(5):e021078
Moons KG, Altman DG, Reitsma JB, Ioannidis JPA, Macaskll P, Steyerberg EW, Vickers AJ, Ransohoff DF, Collins GS (2015) Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 162(1):W1–W73
Rushton A, Wright C, Heap A, White L, Eveleigh G, Heneghan N (2014) Survey of current physiotherapy practice for patients undergoing lumbar spinal fusion in the United Kingdom. Spine 39(23):E1380–E1387
Rushton AB, Zoulas K, Powell A, Staal JB (2018) Physical prognostic factors predicting outcome following lumbar discectomy surgery: systematic review and narrative synthesis. BMC Musculoskelet Disord 19(11):326
Childs JD, Piva SR, Fritz JM (2005) Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 30(11):1331–1334
Fairbank JC, Pynsent PB (2000) The Oswestry disability index. Spine 25(22):2940–2953
Asher AL, Kerezoudis P, Mummaneni PV, Bisson EF, Glassman SD, Foley KT, Slotkin JR, Potts EA, Shaffrey ME, Shaffrey CI, Coric D, Knightly JJ, Park P, Fu KM, Devin CJ, Archer KR, Chotai S, Chan AK, Virk MS, Bydon M (2018) Defining the minimum clinically important difference for grade I degenerative lumbar spondylolisthesis: insights from the Quality Outcomes Database. Neurosurg Focus 44(1):1–7
Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson A, Cheng JS, McGirt MJ (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 14(5):598–604
Binkley JM, Stratford PW, Lott SA, Riddle DL (1999) The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther 79(4):371–383
Gibson JNA, Grant TC, Waddell G (1999) The Cochrane review of surgery for lumbar disc prolapse and degenerative lumbar spondylosis. Spine 1(24):1820–1832
Li P, Stuart EA, Allison DB (2016) Multiple Imputation: a flexible tool for handling missing data. JAMA 314(18):1966–1967
Schafer JL (1999) Multiple Imputation: a primer. Stat Methods Med Res 8:3–15
Van Buuren S (2018) Flexible imputation of missing data, 2nd edn. Chapman & Hall/CRC, Boca Raton
Peduzzi P, Concato J, Kemper E, Holford TR, Feintein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379
Vittinghoff E, McCulloch CE (2007) Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol 165(6):710–718
Steyeberg EW, Moons KGM, van der Windt DA, Hayden JA, Perel P, Schroter S, Riley RD, Hemingway H, Altman DG, PROGRESS Group (2013) Prognosis research strategy (PROGRESS): prognostic model research. PLoS Med 10(2):e1001381
Deyo RA, Ciol MA, Cherkin DC (1993) Lumbar spinal fusion: a cohort study of complications, re-operations and resources use in the Medicare population. Spine 18(11):1463–1470
Koenders N, Rushton A, Verra ML, Willems PC, Hoogeboom TJ, Staal JB (2019) Pain and disability after first-time spinal fusion for lumbar degenerative disorders: a systematic review and meta-analysis. Eur Spine J 28(4):696–709
Rushton A, Jadhakhan F, Masson A, Athey V, Staal JB, Verra ML, Emms A, Reddington M, Cole A, Willems PC, Benneker L (2020) Patient journey following lumbar spinal fusion surgery (FuJourn): a multicentre exploration of the immediate post-operative period using qualitative patient diaries. PLoS ONE 15(12):e0241931
Giannadakis C, Verland ULFS, Sohein O, Jokola AS, Gulati M, Weber C, Nygaard OP, Solberg TK, Gulati S (2015) Does obesity affect outcomes after decompressive surgery for lumbar spinal stenosis? A multicentre, observational, registry-based study. World Neurosurg 378(9802):1560–1571
Knutsson B, Michaellsson K, Sanden B (2013) Obesity is associated with inferior results after surgery for lumbar spinal stenosis: a study of 2633 patient from the Swedish spine registry. Spine 38(5):435–441
Kehlet H, Holte K (2001) Effect of postoperative analgesia on surgical outcome. Br J Anaesth 87(1):62–72
Lundbald H, Kreicbergs A, Jansson KA (2008) Prediction of persistent pain after total knee replacement for osteoarthritis. J Bone Joint Surg Br 90(2):166–171
DeBerard MS, Wheeler AJ, Gundy JM, Stein DM, Colledge AL (2011) Presurgical biopsychosocial variables predict medical, compensation, and aggregate costs of lumbar discectomy in Utah workers’ compensation patients. Spine J 11(5):395–401
Sigmundsson FG, Kang XP, Jonsson B, Stromqvist B (2000) Prognostic factors in lumbar surgery outcome. Spine 25(20):2616–2621
Dzioba RB, Doxey NC (1984) A prospective investigation into the orthopaedic and psychologic predictors of outcome of first lumbar surgery following industrial injury. Spine 9(6):614–623
Graver V, Haaland AK, Magnaes B, Loeb M (1999) Seven-year clinical follow-up after lumbar disc surgery results and predictors of outcome. Br J Neurosurg 13(2):178–184
Rubin DB (1987) Multiple imputation for nonresponse in surveys. Wiley and Sons, New York
Funding
Modification of the British Spine Registry was supported by Research Stimulation Funding from the University of Birmingham, UK.
Author information
Authors and Affiliations
Contributions
AR is the chief investigator leading protocol development, study management, data analyses, interpretation and dissemination. AR, JBS and MLV led on design and data analysis plans. AR, JBS, MLV, AAC, PW, LB and MH contributed to methodological decisions. MH is the study statistician. FJ carried out the data analyses. AR, JBS, MLV, AAC, PW, LB, AE, MR, NRH and DF have contributed subject-specific expertise (rehabilitation and surgical). AAC, DS and MWH enabled British Spine Registry collaboration and modification. All authors will contribute to data interpretation, conclusions and dissemination. AR and FJ drafted the initial manuscript. All reviewers have read, contributed to and agreed the final manuscript. AR is the guarantor.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the University of Birmingham Ethics Committee (ERN_17-0446).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rushton, A.B., Jadhakhan, F., Verra, M.L. et al. Predictors of poor outcome following lumbar spinal fusion surgery: a prospective observational study to derive two clinical prediction rules using British Spine Registry data. Eur Spine J 32, 2303–2318 (2023). https://doi.org/10.1007/s00586-023-07754-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07754-w