Abstract
Purpose
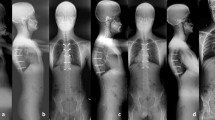
Posterior spinal fusion (PSF) at skeletal maturity is still the gold standard in children with neuromuscular scoliosis (NMS) who underwent fusionless surgery. The aim of this computed tomography (CT) study was to quantify the spontaneous bone fusion at the end of a lengthening program by minimally invasive fusionless bipolar fixation (MIFBF), that could avoid PSF.
Methods
NMS operated on with MIFBF from T1 to the pelvis and at final lengthening program were included. CT was performed at least five years postoperatively. The autofusion was classified as completely or not fused at the facets joint (on both coronal and sagittal plane, right and left side, from T1 to L5), and around the rods (axial plane, right and left side, from T5 to L5). Vertebral body heights were assessed.
Results
Ten patients were included (10.7y ± 2 at initial surgery). Mean Cobb angle was 82 ± 20 preoperatively and 37 ± 13 at last follow-up. CT were performed on average 6.7y ± 1.7 after initial surgery. Mean preoperative and last follow-up thoracic vertebrae height were respectively 13.5 mm ± 1.7 and 17.4 mm ± 1.7 (p < 0.001). 93% facets joints were fused (out of 320 analyzed joints), corresponding to 15/16 vertebral levels. Ossification around the rods was observed in 6.5±2.4 levels out of 13 in the convex side, and 4.2 ± 2.2 in the concave side (p = 0.04).
Conclusions
This first computed quantitative study showed MIFBF in NMS preserved spinal growth, while it induced 93% of facet joints fusion. This could be is an additional argument when questionning the real need for PSF at skeletal maturity.






Similar content being viewed by others
References
Thometz JG, Simon SR (1988) Progression of scoliosis after skeletal maturity in institutionalized adults who have cerebral palsy. J Bone Joint Surg Am 70A:1290–1296
Saito N, Ebara S, Ohotsuka K et al (1998) Natural history of scoliosis in spastic cerebral palsy. Lancet 351:1687–1692. https://doi.org/10.1016/S0140-6736(98)01302-6
Fernandes P, Weinstein SL (2007) Natural history of early onset scoliosis. J Bone Joint Surg Am 89(Suppl 1):21–33. https://doi.org/10.2106/JBJS.F.00754
Bowen RE, Scaduto AA, Banuelos S (2008) Does early thoracic fusion exacerbate preexisting restrictive lung disease in congenital scoliosis patients? J Pediatr Orthop 28:506–511. https://doi.org/10.1097/BPO.0b013e31817b931c
Campbell RM, Smith MD, Mayes TC, Mangos JA, Willey Courand DB, Kose N, Pinero RF, Adler ME, Duong HL, Surber JL (2003) The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am 85:399–408. https://doi.org/10.2106/00004623-200303000-00001
Goldberg CJ, Moore DP, Fogarty EE, Dowling FE (2002) Long-term results from in situ fusion for congenital vertebral deformity. Spine 27:619–628. https://doi.org/10.1097/00007632-200203150-00011
Karol LA, Johnston C, Mladenov K, Schochet P, Walters P, Browne RH (2008) Pulmonary function following early thoracic fusion in non-neuromuscular scoliosis. J Bone Joint Surg Am 90:1272–1281. https://doi.org/10.2106/JBJS.G.00184
Dubousset J, Herring JA, Shufflebarger H (1989) The crankshaft phenomenon. J Pediatr Orthop 9:541–550. https://doi.org/10.1097/01241398-198909010-00008
Zhang H, Sucato DJ (2008) Unilateral pedicle screw epiphysiodesis of the neurocentral synchondrosis. Production of idiopathic-like scoliosis in an immature animal model. J Bone Joint Surg Am 90:2460–2469. https://doi.org/10.2106/JBJS.G.01493
Chest Wall and Spine Deformity Study Group, Growing Spine Study Group, Pediatric Orthopaedic Society of North America, Scoliosis Research Society Growing Spine Study Committee, Skaggs DL, Akbarnia BA, Flynn JM, Myung KS, Sponseller PD, Vitale MG (2014) A classification of growth friendly spine implants. J Pediatr Orthop 34(3):260–274. https://doi.org/10.1097/BPO.0000000000000073
Akbarnia BA, Marks DS, Boachie-Adjei O, Thompson AG, Asher MA (2005) Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine 30:S46–S57. https://doi.org/10.1097/01.brs.0000175190.08134.73
Balsano M, Spina M (2020) Idiopathic early-onset scoliosis treated with Magec rods: what to do after the lengthening period is over? Int J Spine Surg 14(5):847–851. https://doi.org/10.14444/7094. (Epub 2020 Aug 25)
Poe-Kochert C, Shannon C, Pawelek JB, Thompson GH, Hardesty CK, Marks DS, Akbarnia BA, McCarthy RE, Emans JB (2016) Final fusion after growing-rod treatment for early onset scoliosis: is it final? J Bone Joint Surg Am 98(22):1913–1917. https://doi.org/10.2106/JBJS.15.01334
Growing Spine Study Group, Flynn JM, Tomlinson LA, Pawelek J, Thompson GH, McCarthy R, Akbarnia BA (2013) Growing-rod graduates: lessons learned from ninetynine patients who completed lengthening. J Bone Joint Surg Am 95(19):1745–1750. https://doi.org/10.2106/JBJS.L.01386
Pediatric Spine Study Group, Du JY, Poe-Kochert C, Thompson GH, Hardesty CK, Pawelek JB, Flynn JM, Emans JB (2020) Risk factors for reoperation following final fusion after the treatment of early-onset scoliosis with traditional growing rods. J Bone Joint Surg Am 102(19):1672–1678. https://doi.org/10.2106/JBJS.20.00312
Growing Spine Study Group, Jain A, Sponseller PD, Flynn JM, Shah SA, Thompson GH, Means JB, Pawelek JB, Akbarnia BA (2016) Avoidance of “Final” surgical fusion after growing-rod treatment for early-onset scoliosis. J Bone Joint Surg Am 98(13):1073–1078. https://doi.org/10.2106/JBJS.15.01241
Bouthors C, Gaume M, Glorion C, Miladi L (2019) Outcomes at skeletal maturity of 34 children with scoliosis treated with a traditional single growing rod. Spine 44(23):1630–1637. https://doi.org/10.1097/BRS.0000000000003148
Gaume M, Vergari C, Khouri N, Skalli W, Glorion C, Miladi L (2021) Minimally invasive surgery for neuromuscular scoliosis: results and complications at a minimal follow-up of 5 years. Spine 46(24):1696–1704. https://doi.org/10.1097/BRS.0000000000004082
Shao Y-H, Tsai K, Kim S, Yu-Jen Wu Y-J, Demissie K (2019) Exposure to tomographic scans and cancer risks. JNCI Cancer Spectr 4(1):pkz072. https://doi.org/10.1093/jncics/pkz072
Miladi L, Gaume M, Khouri N et al (2018) Minimally invasive surgery for neuromuscular scoliosis: results and complications in a series of one hundred patients. Spine 43:E968–E975. https://doi.org/10.1097/BRS.0000000000002588
Gaume M, Persohn S, Vergari C et al (2020) Biomechanical cadaver study of proximal fixation in a minimally invasive bipolar construct. Spine Deform 8:33–38. https://doi.org/10.1007/s43390-019-00014-2
Dubousset J, Gaume M, Miladi L (2021) Ilio-sacral screw pelvic fixation when correcting spinal deformities with or without pelvic obliquity: our experience over 40 years. Spine Deform 9:665–670. https://doi.org/10.1007/s43390-020-00263-6
Miladi LT, Ghanem IB, Draoui MM et al (1997) Ilio-sacral screw fixation for pelvic obliquity in neuromuscular scoliosis. Long-term Followup study Spine 22:1722–1729. https://doi.org/10.1007/s00402-021-04332-x
Gaume M, Gerard P, Khouri N, Glorion C, Dubousset J, Miladi L (2022) Long-term outcomes of ilio-sacral screws in minimally invasive bipolar fusionless technique for neuromuscular scoliosis: a retrospective study in 167 patients. Arch Orthop Trauma Surg 143(4):1761–1767. https://doi.org/10.1007/s00402-021-04332-x
Frobin W, Brinckmann P, Biggemann M, Tillotson M, Burton K (1997) Precision measurement of disc height, vertebral height, and sagittal plane displacement from lateral radiographic views of the lumbar spine. Clin Biomech (Bristol, Avon) 12(Suppl 1):S1–S63. https://doi.org/10.1016/s0268-0033(96)00067-8
de Reuver S, Costa L, Van Rheenen H, Tabeling CS, Lemans JVC, Schlösser TPC, Kruyt MC, Van Stralen M, Castelein RM (2022) Disc and vertebral body morphology from birth to adulthood. Spine 47(7):E312–E318. https://doi.org/10.1097/BRS.0000000000004278
Cobb JR (ed) (1948) Outline for the study of scoliosis. Instructional course lectures 5:261–275
Moe JH, Kharrat K, Winter RB et al (1984) Harrington instrumentation without fusion plus external orthotic support for the treatment of difficult curvature problems in young children. Clin Orthop Relat Res 185:35–45
Mardjetko SM, Hammerberg KW, Lubicky JP et al (1992) The Luque trolley revisited, review of nine cases requiring revision. Spine 17:582–589. https://doi.org/10.1097/00007632-199205000-00018
Cahill PJ, Marvil S, Cuddihy L, Schutt C, Idema J, Clements DH, Antonacci MD, Asghar J, Samdani AF, Betz RR (2010) Autofusion in the immature spine treated with growing rods. Spine 35(22):E1199-1203. https://doi.org/10.1097/BRS.0b013e3181e21b50
Sankar WN, Skaggs DL, Yazici M et al (2011) Lengthening of dual growing rods and the law of diminishing returns. Spine 36:806–809. https://doi.org/10.1097/BRS.0b013e318214d78f
Noordeen HM, Shah SA, Elsebaie HB et al (2011) In vivo distraction force and length measurements of growing rods: which factors influence the ability to lengthen? Spine 36:2299–2303. https://doi.org/10.1097/BRS.0b013e31821b8e16
Tsirikos AI, Lipton G, Chang WN et al (2008) Surgical correction of scoliosis in pediatric patients with cerebral palsy using the unit rod instrumentation. Spine 33:1133–1140. https://doi.org/10.1097/BRS.0b013e31816f63cf
Tsirikos AI, Mains E (2012) Surgical correction of spinal deformity in patients why cerebral palsy using pedicle screws instrumentation. J Spinal Disord Tech 25:404–408. https://doi.org/10.1097/BSD.0b013e318227728c
Kocyigit IA, Olgun ZD, Demirkiran HG, Ayvaz M, Yazici M (2017) Graduation protocol after growing-rod treatment: removal of implants without new instrumentation is not a realistic approach. J Bone Joint Surg Am 99(18):1554–1564. https://doi.org/10.2106/JBJS.17.00031
Murphy RF, Barfield WR, Emans JB, Akbarnia B et al (2020) Minimum 5-year follow-up on graduates of growing spine surgery for early onset scoliosis. J Pediatr Orthop 40(10):e942–e946. https://doi.org/10.1097/BPO.0000000000001646
Pediatric Spine Study Group, Akbarnia BA, Pawelek JB, Hosseini P, Salari P, Kabirian N, Marks D, Shah SA, Skaggs DL, Emans JB, Elsebaie H, Thompson GH, Sponseller PD (2022) Treatment of early-onset scoliosis: similar outcomes despite different etiologic subtypes in traditional growing rod graduates. J Pediatr Orthop. 42(1):10–16. https://doi.org/10.1097/BPO.0000000000001985
Abul-Kasim K et al (2009) Low-dose helical computed helical tomography (CT) in the perioperative work-up of adolescent idiopathic scoliosis. Eur Radiol 19(3):610–618. https://doi.org/10.1007/s00330-008-1178-4
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript: Mathilde Gaume, Klervie Loiselet, Hedi Chekir, Tristan Langlais, Nathalie Boddaert, Stéphanie Pannier, Wafa Skalli and Claudio Vergari declare no relationships with any companies, whose products or services may be related to the subject matter of the article. Lotfi Miladi is a consultant from EUROS company.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gaume, M., Langlais, T., Loiselet, K. et al. Spontaneous induced bone fusion in minimally invasive fusionless bipolar fixation in neuromuscular scoliosis: a computed tomography analysis. Eur Spine J 32, 2550–2557 (2023). https://doi.org/10.1007/s00586-023-07745-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07745-x