Abstract
Purpose
To develop and evaluate a quantile regression-based blood loss prediction model for open surgery of spinal metastases.
Methods
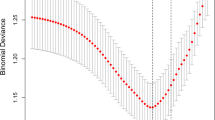
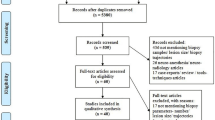
This was a multicenter retrospective cohort study. Over a 11-year period, patients underwent open surgery for spinal metastases at 6 different institutions were reviewed. The outcome measure is intraoperative blood loss (in mL). The effects of baseline, histology of primary tumor and surgical procedure on blood loss were evaluated by univariate and multivariate analysis to determine the predictors. Multivariate ordinary least squares (OLS) regression and 0.75 quantile regression were used to establish two prediction models. The performance of the two models was evaluated in the training set and the test set, respectively.
Results
528 patients were included in this study. Mean age was 57.6 ± 11.2 years, with a range of 20–86 years. Mean blood loss was 1280.1 ± 1181.6 mL, with a range of 10 ~ 10,000 mL. Body mass index (BMI), tumor vascularization, surgical site, surgical extent, total en bloc spondylectomy and microwave ablation use were significant predictors of intraoperative blood loss. Hypervascular tumor, higher BMI, and broader surgical extent were related with massive blood loss. Microwave ablation is more beneficial in surgery with substantial blood loss. Compared to the OLS regression model, the 0.75 quantile regression model may decrease blood loss underestimate.
Conclusion
In this study, we developed and evaluated a prediction model for blood loss in open surgery for spinal metastases based on 0.75 quantile regression, which may minimize blood loss underestimate.





Similar content being viewed by others
References
Chen Y, Tai BC, Nayak D, Kumar N, Chua KH, Lim JW, Goy RW, Wong HK (2013) Blood loss in spinal tumour surgery and surgery for metastatic spinal disease: a meta-analysis. Bone Joint J 95:683–688. https://doi.org/10.1302/0301-620x.95b5.31270
Wright E, Ricciardi F, Arts M, Buchowski JM, Chung CK, Coppes M, Crockard A, Depreitere B, Fehlings M, Kawahara N, Lee CS, Leung Y, Martin-Benlloch A, Massicotte E, Mazel C, Oner C, Peul W, Quraishi N, Tokuhashi Y, Tomita K, Ulbricht C, Verlaan JJ, Wang M, Choi D (2018) Metastatic spine tumor epidemiology: comparison of trends in surgery across two decades and three continents. World Neurosurg 114:e809–e817. https://doi.org/10.1016/j.wneu.2018.03.091
Zhang HR, Qiao RQ, Yang XG, Hu YC (2020) A multicenter, descriptive epidemiologic survey of the clinical features of spinal metastatic disease in China. Neurol Res 42:749–759. https://doi.org/10.1080/01616412.2020.1773630
Asano K, Nakano T, Takeda T, Ohkuma H (2009) Risk factors for postoperative systemic complications in elderly patients with brain tumors. Clinical article J Neurosurg 111:258–264. https://doi.org/10.3171/2008.10.17669
Schiergens TS, Stielow C, Schreiber S, Hornuss C, Jauch KW, Rentsch M, Thasler WE (2014) Liver resection in the elderly: significance of comorbidities and blood loss. J Gastrointest Surg 18:1161–1170. https://doi.org/10.1007/s11605-014-2516-2
He YK, Li HZ, Lu HD (2019) Is blood transfusion associated with an increased risk of infection among spine surgery patients?: A meta-analysis. Med Baltim. 98:e16287. https://doi.org/10.1097/md.0000000000016287
Elsamadicy AA, Adil SM, Charalambous L, Drysdale N, Koo AB, Lee M, Kundishora AJ, Camara-Quintana J, Kolb L, Laurans M, Abbed K, Karikari IO (2020) Independent association between type of intraoperative blood transfusion and postoperative delirium after complex spinal fusion for adult deformity correction. Spine Phila Pa 45:268–274. https://doi.org/10.1097/brs.0000000000003260
Aoude A, Aldebeyan S, Fortin M, Nooh A, Jarzem P, Ouellet JA, Weber MH (2017) Prevalence and complications of postoperative transfusion for cervical fusion procedures in spine surgery: an analysis of 11,588 patients from the american college of surgeons national surgical quality improvement program database. Asian Spine J 11:880–891. https://doi.org/10.4184/asj.2017.11.6.880
Aoude A, Nooh A, Fortin M, Aldebeyan S, Jarzem P, Ouellet J, Weber MH (2016) Incidence, predictors, and postoperative complications of blood transfusion in thoracic and lumbar fusion surgery: an analysis of 13,695 patients from the American college of surgeons national surgical quality improvement program database. Global Spine J 6:756–764. https://doi.org/10.1055/s-0036-1580736
Cui Y, Shi X, Mi C, Wang B, Li H, Pan Y, Lin Y (2021) Risk factors of total blood loss in the posterior surgery for patients with thoracolumbar metastasis. BMC Musculoskelet Disord 22:898. https://doi.org/10.1186/s12891-021-04789-2
Kumar N, Zaw AS, Khine HE, Maharajan K, Wai KL, Tan B, Mastura S, Goy R (2016) Blood loss and transfusion requirements in metastatic spinal tumor surgery: evaluation of influencing factors. Ann Surg Oncol 23:2079–2086. https://doi.org/10.1245/s10434-016-5092-8
Mohme M, Mende KC, Pantel T, Viezens L, Westphal M, Eicker SO, Dreimann M, Krätzig T, Stangenberg M (2021) Intraoperative blood loss in oncological spine surgery. Neurosurg Focus 50:E14. https://doi.org/10.3171/2021.2.Focus201117
Kumar N, Ramos MRD, Patel R, Tan BWL, Lopez KG, Nolan CP, Kumar A, Kumar DS, Liu G, Benneker LM (2021) The spinal metastasis invasiveness index: a novel scoring system to assess surgical invasiveness. Spine Phila Pa 46:478–485. https://doi.org/10.1097/brs.0000000000003823
Gao X, Fan T, He S, Wan W, Zhao C, Wang D, Tang L, Lou Y, Li Z, Liu T, Xiao J (2020) A useful model for predicting intraoperative blood loss in metastatic spine tumor surgery. Clin Spine Surg 33:E256-e262. https://doi.org/10.1097/bsd.0000000000000911
Pennington Z, Ehresman J, Feghali J, Schilling A, Hersh A, Hung B, Lubelski D, Sciubba DM (2021) A clinical calculator for predicting intraoperative blood loss and transfusion risk in spine tumor patients. Spine J 21:302–311. https://doi.org/10.1016/j.spinee.2020.09.011
Stock J, Watson M (2011) Introduction to econometrics (3rd edition). Addison Wesley Longman
Hao L, Naiman D (2007) Quantile regression
Austin PC, Schull MJ (2003) Quantile regression: a statistical tool for out-of-hospital research. Acad Emerg Med 10:789–797. https://doi.org/10.1111/j.1553-2712.2003.tb00075.x
Do YK, Foo K, Ng YY, Ong ME (2013) A quantile regression analysis of ambulance response time. Prehosp Emerg Care 17:170–176. https://doi.org/10.3109/10903127.2012.729127
Tian H, Yim A, Newton DP (2021) Tail-heaviness, asymmetry, and profitability forecasting by quantile regression. Manage Sci 67:5209–5233. https://doi.org/10.1287/mnsc.2020.3694
Khattak AJ, Liu J, Wali B, Li X, Ng M (2016) Modeling traffic incident duration using quantile regression. Transp Res Record. 2554(1):139–148. https://doi.org/10.3141/2554-15
Konstantopoulos S, Li W, Miller S, van der Ploeg A (2019) Using quantile regression to estimate intervention effects beyond the mean. Educ Psychol Meas 79:883–910. https://doi.org/10.1177/0013164419837321
Bilsky MH, Fraser JF (2006) Complication avoidance in vertebral column spine tumors. Neurosurg Clin N Am 17:317–329. https://doi.org/10.1016/j.nec.2006.04.007
Holman PJ, Suki D, McCutcheon I, Wolinsky JP, Rhines LD, Gokaslan ZL (2005) Surgical management of metastatic disease of the lumbar spine: experience with 139 patients. J Neurosurg Spine 2:550–563. https://doi.org/10.3171/spi.2005.2.5.0550
Clausen C, Dahl B, Frevert SC, Hansen LV, Nielsen MB, Lönn L (2015) Preoperative embolization in surgical treatment of spinal metastases: single-blind, randomized controlled clinical trial of efficacy in decreasing intraoperative blood loss. J Vasc Interv Radiol 26:402-412.e401. https://doi.org/10.1016/j.jvir.2014.11.014
Freeman AK, Thorne CJ, Gaston CL, Shellard R, Neal T, Parry MC, Grimer RJ, Jeys L (2017) Hypotensive epidural anesthesia reduces blood loss in pelvic and sacral bone tumor resections. Clin Orthop Relat Res 475:634–640. https://doi.org/10.1007/s11999-016-4858-4
Tang X, Guo W, Yang R, Tang S, Ji T (2009) Risk factors for blood loss during sacral tumor resection. Clin Orthop Relat Res 467:1599–1604. https://doi.org/10.1007/s11999-008-0483-1
Kawai A, Kadota H, Yamaguchi U, Morimoto Y, Ozaki T, Beppu Y (2005) Blood loss and transfusion associated with musculoskeletal tumor surgery. J Surg Oncol 92:52–58. https://doi.org/10.1002/jso.20375
Ozkan E, Gupta S (2011) Embolization of spinal tumors: vascular anatomy, indications, and technique. Tech Vasc Interv Radiol 14:129–140. https://doi.org/10.1053/j.tvir.2011.02.005
Wang Y, Hu J, Ng CS, Hobbs BP (2020) A functional model for classifying metastatic lesions integrating scans and biomarkers. Stat Methods Med Res 29:137–150. https://doi.org/10.1177/0962280218823795
Mazura JC, Karimi S, Pauliah M, Banihashemi MA, Gobin YP, Bilsky MH, Patsalides A (2014) Dynamic contrast-enhanced magnetic resonance perfusion compared with digital subtraction angiography for the evaluation of extradural spinal metastases: a pilot study. Spine Phila Pa 1976 39:950–954. https://doi.org/10.1097/brs.0000000000000409
Yin P, Sun C, Wang S, Chen L, Hong N (2021) Clinical-deep neural network and clinical-radiomics nomograms for predicting the intraoperative massive blood loss of pelvic and sacral tumors. Front Oncol 11:752672. https://doi.org/10.3389/fonc.2021.752672
Khan MA, Deib G, Deldar B, Patel AM, Barr JS (2018) Efficacy and safety of percutaneous microwave ablation and cementoplasty in the treatment of painful spinal metastases and myeloma. AJNR Am J Neuroradiol 39:1376–1383. https://doi.org/10.3174/ajnr.A5680
Pusceddu C, Sotgia B, Fele RM, Melis L (2013) Treatment of bone metastases with microwave thermal ablation. J Vasc Interv Radiol 24:229–233. https://doi.org/10.1016/j.jvir.2012.10.009
Liu B, Yuan Z, Wei CY (2018) Combined microwave ablation and minimally invasive open decompression for the management of thoracic metastasis in breast cancer. Cancer Manag Res 10:1397–1401. https://doi.org/10.2147/cmar.S159561
Wei X, Chen B, Nan L, Shi Y, Wu WW, Ma Y, Hou S (2017) Open microwave ablation in the treatment of spinal metastasis: Preliminary experience. Biomed Res India 28:261–267
Gong Y, Wang C, Liu H, Liu X, Jiang L (2020) Only tumors angiographically identified as hypervascular exhibit lower intraoperative blood loss upon selective preoperative embolization of spinal metastases: systematic review and meta-analysis. Front Oncol 10:597476. https://doi.org/10.3389/fonc.2020.597476
Houten JK, Swiggett SJ, Hadid B, Choueka DM, Kinon MD, Buciuc R, Zumofen DW (2020) Neurologic complications of preoperative embolization of spinal metastasis: a systemic review of the literature identifying distinct mechanisms of injury. World Neurosurg 143:374–388. https://doi.org/10.1016/j.wneu.2020.08.006
Wang B, Han SB, Jiang L, Liu XG, Yang SM, Meng N, Wei F, Liu ZJ (2018) Intraoperative vertebroplasty during surgical decompression and instrumentation for aggressive vertebral hemangiomas: a retrospective study of 39 patients and review of the literature. Spine J 18:1128–1135. https://doi.org/10.1016/j.spinee.2017.11.003
Dong L, Tan M, Wu D, Yi P, Yang F, Tang X, Hao Q (2017) Palliative surgery for spinal metastases using posterior decompression and fixation combined with intraoperative vertebroplasty. Clin Spine Surg 30:343–349. https://doi.org/10.1097/bsd.0000000000000253
Zhang C, Han X, Li L, Zhang C, Ma Y, Wang G (2020) Posterior decompression surgery and radiofrequency ablation followed by vertebroplasty in spinal metastases from lung cancer. Med Sci Monit 26:e925169. https://doi.org/10.12659/msm.925169
Jiang J, Zhou R, Li B, Xue F (2019) Is deliberate hypotension a safe technique for orthopedic surgery?: a systematic review and meta-analysis of parallel randomized controlled trials. J Orthop Surg Res 14:409. https://doi.org/10.1186/s13018-019-1473-6
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58:277–280. https://doi.org/10.1097/00000542-198303000-00016
Acknowledgements
Thanks to Ruiqi Qiao for his contribution to data extraction in this study.
Author information
Authors and Affiliations
Contributions
JL and JZ contributed equally to this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There are no financing or financial conflicts of interest to disclose.
Ethical approval
This study was conducted following the declaration of Helsinki. In view of the retrospective nature of the study, the six institutions (Tianjin Hospital, Tianjin Medical University Cancer Institute and Hospital, Third Hospital of Hebei Medical University, the 960th Hospital of PLA Joint Logistics Support Force, Guangdong Provincial People's Hospital, and The Second Affiliated Hospital, Zhejiang University School of Medicine) unanimously approved the study protocol, and required neither patient approval nor informed consent to review patients’ medical records.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, J., Zhang, J., Zhang, X. et al. Quantile regression-based prediction of intraoperative blood loss in patients with spinal metastases: model development and validation. Eur Spine J 32, 2479–2492 (2023). https://doi.org/10.1007/s00586-023-07653-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07653-0