Abstract
Purpose
Predict nonhome discharge (NHD) following elective anterior cervical discectomy and fusion (ACDF) using an explainable machine learning model.
Methods
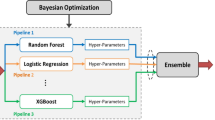
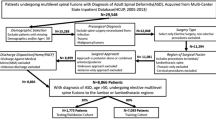
2227 patients undergoing elective ACDF from 2008 to 2019 were identified from a single institutional database. A machine learning model was trained on preoperative variables, including demographics, comorbidity indices, and levels fused. The validation technique was repeated stratified K-Fold cross validation with the area under the receiver operating curve (AUROC) statistic as the performance metric. Shapley Additive Explanation (SHAP) values were calculated to provide further explainability regarding the model’s decision making.
Results
The preoperative model performed with an AUROC of 0.83 ± 0.05. SHAP scores revealed the most pertinent risk factors to be age, medicare insurance, and American Society of Anesthesiology (ASA) score. Interaction analysis demonstrated that female patients over 65 with greater fusion levels were more likely to undergo NHD. Likewise, ASA demonstrated positive interaction effects with female sex, levels fused and BMI.
Conclusion
We validated an explainable machine learning model for the prediction of NHD using common preoperative variables. Adding transparency is a key step towards clinical application because it demonstrates that our model’s “thinking” aligns with clinical reasoning. Interactive analysis demonstrated that those of age over 65, female sex, higher ASA score, and greater fusion levels were more predisposed to NHD. Age and ASA score were similar in their predictive ability. Machine learning may be used to predict NHD, and can assist surgeons with patient counseling or early discharge planning.




Similar content being viewed by others
References
Epstein NE (2019) A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int. https://doi.org/10.25259/SNI-191-2019
Fountas KN, Kapsalaki EZ, Nikolakakos LG et al (2007) Anterior cervical discectomy and fusion associated complications. Spine 32:2310–2317. https://doi.org/10.1097/BRS.0b013e318154c57e
Newhouse JP, Garber AM (2013) Geographic variation in medicare services. N Engl J Med 368:1465–1468. https://doi.org/10.1056/NEJMp1302981
Neifert SN, Gal JS, Chapman EK, Caridi JM (2020) Nonhome discharge as an independent risk factor for adverse events and readmission in patients undergoing anterior cervical discectomy and fusion. Clin Spine Surg 33:E454–E459. https://doi.org/10.1097/BSD.0000000000000961
Schoenfeld AJ, Harris MB, Liu H, Birkmeyer JD (2014) Variations in medicare payments for episodes of spine surgery. Spine J 14:2793–2798. https://doi.org/10.1016/j.spinee.2014.07.002
Dial BL, Esposito VR, Danilkowicz R et al (2020) Factors associated with extended length of stay and 90-day readmission rates following ACDF. Glob Spine J. https://doi.org/10.1177/2192568219843111
Lopez CD, Boddapati V, Lombardi JM et al (2020) Recent trends in medicare utilization and reimbursement for anterior cervical discectomy and fusion. Spine J 20:1737–1743. https://doi.org/10.1016/j.spinee.2020.06.010
Virk SS, Phillips FM, Khan SN (2016) Reimbursement related to a 90-day episode of care for a one or two-level anterior cervical discectomy and fusion. J Bone Joint Surg Am 98:1378–1384. https://doi.org/10.2106/JBJS.15.01169
Goyal A, Ngufor C, Kerezoudis P et al (2019) Can machine learning algorithms accurately predict discharge to nonhome facility and early unplanned readmissions following spinal fusion? Analysis of a national surgical registry. J Neurosurg Spine. https://doi.org/10.3171/2019.3.SPINE181367
Martini ML, Neifert SN, Oermann EK et al (2021) Application of cooperative game theory principles to interpret machine learning models of nonhome discharge following spine surgery. Spine 46:803–812. https://doi.org/10.1097/BRS.0000000000003910
Poon AIF, Sung JJY (2021) Opening the black box of AI-medicine. J Gastroenterol Hepatol 36:581–584. https://doi.org/10.1111/jgh.15384
Alsoof D, McDonald CL, Kuris EO, Daniels AH (2022) Machine learning for the orthopaedic surgeon: uses and limitations. J Bone Joint Surg Am. https://doi.org/10.2106/JBJS.21.01305
Lundberg S, Lee S-I (2017) A unified approach to interpreting model predictions. arXiv [cs.AI]
Lundberg SM, Nair B, Vavilala MS et al (2018) Explainable machine-learning predictions for the prevention of hypoxaemia during surgery. Nat Biomed Eng 2:749–760. https://doi.org/10.1038/s41551-018-0304-0
Pedregosa F, Varoquaux G, Gramfort A et al (2011) Scikit-learn: machine learning in python. J Mach Learn Res 12:2825–2830
Ley C, Martin RK, Pareek A et al (2022) Machine learning and conventional statistics: making sense of the differences. Knee Surg Sports Traumatol Arthrosc 30:753–757. https://doi.org/10.1007/s00167-022-06896-6
Chandra A, Dalton MA, Holmes J (2013) Large increases in spending on postacute care in medicare point to the potential for cost savings in these settings. Health Aff 32:864–872. https://doi.org/10.1377/hlthaff.2012.1262
Centers for Medicare & Medicaid Services Data. https://data.cms.gov/provider-summary-by-type-of-service/medicare-post-acute-care-hospice/medicare-post-acute-care-hospice-by-provider-and-service/data/2019. Accessed 10 Jan 2022
Salas-Vega S, Chakravarthy VB, Winkelman RD et al (2021) Late-week surgery and discharge to specialty care associated with higher costs and longer lengths of stay after elective lumbar laminectomy. J Neurosurg Spine. https://doi.org/10.3171/2020.11.SPINE201403
Rosman M, Rachminov O, Segal O, Segal G (2015) Prolonged patients’ in-hospital waiting period after discharge eligibility is associated with increased risk of infection, morbidity and mortality: a retrospective cohort analysis. BMC Health Serv Res 15:246. https://doi.org/10.1186/s12913-015-0929-6
Price WN (2018) Big data and black-box medical algorithms. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aao5333
Di Capua J, Somani S, Kim JS et al (2017) Predictors for patient discharge destination after elective anterior cervical discectomy and fusion. Spine 42:1538–1544. https://doi.org/10.1097/BRS.0000000000002140
Martini ML, Neifert SN, Gal JS et al (2021) Drivers of prolonged hospitalization following spine surgery: a game-theory-based approach to explaining machine learning models. J Bone Joint Surg Am 103:64–73. https://doi.org/10.2106/JBJS.20.00875
Ondeck NT, Bohl DD, Bovonratwet P et al (2018) Discriminative ability of commonly used indices to predict adverse outcomes after poster lumbar fusion: a comparison of demographics, ASA, the modified Charlson Comorbidity Index, and the modified Frailty Index. Spine J 18:44–52. https://doi.org/10.1016/j.spinee.2017.05.028
Buerba RA, Giles E, Webb ML et al (2014) Increased risk of complications after anterior cervical discectomy and fusion in the elderly: an analysis of 6253 patients in the American College of Surgeons National Surgical Quality Improvement Program database. Spine 39:2062–2069. https://doi.org/10.1097/BRS.0000000000000606
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
IRB approval was obtained for the submitted work at our institution, the Icahn School of Medicine at Mount Sinai.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geng, E.A., Gal, J.S., Kim, J.S. et al. Robust prediction of nonhome discharge following elective anterior cervical discectomy and fusion using explainable machine learning. Eur Spine J 32, 2149–2156 (2023). https://doi.org/10.1007/s00586-023-07621-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07621-8