Abstract
Purpose
Postoperative complication prediction helps surgeons to inform and manage patient expectations. Deep learning, a model that finds patterns in large samples of data, outperform traditional statistical methods in making predictions. This study aimed to create a deep learning-based model (DLM) to predict postoperative complications in patients with cervical ossification of the posterior longitudinal ligament (OPLL).
Methods
This prospective multicenter study was conducted by the 28 institutions, and 478 patients were included in the analysis. Deep learning was used to create two predictive models of the overall postoperative complications and neurological complications, one of the major complications. These models were constructed by learning the patient's preoperative background, clinical symptoms, surgical procedures, and imaging findings. These logistic regression models were also created, and these accuracies were compared with those of the DLM.
Results
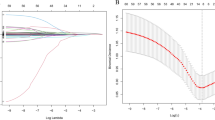
Overall complications were observed in 127 cases (26.6%). The accuracy of the DLM was 74.6 ± 3.7% for predicting the overall occurrence of complications, which was comparable to that of the logistic regression (74.1%). Neurological complications were observed in 48 cases (10.0%), and the accuracy of the DLM was 91.7 ± 3.5%, which was higher than that of the logistic regression (90.1%).
Conclusion
A new algorithm using deep learning was able to predict complications after cervical OPLL surgery. This model was well calibrated, with prediction accuracy comparable to that of regression models. The accuracy remained high even for predicting only neurological complications, for which the case number is limited compared to conventional statistical methods.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Inamasu J, Guiot BH, Sachs DC (2006) Ossification of the posterior longitudinal ligament: an update on its biology, epidemiology, and natural history. Neurosurgery 58:1027–1039. https://doi.org/10.1227/01.Neu.0000215867.87770.73
Mori K, Imai S, Kasahara T, Nishizawa K, Mimura T, Matsusue Y (2014) Prevalence, distribution, and morphology of thoracic ossification of the posterior longitudinal ligament in Japanese: results of CT-based cross-sectional study. Spine 39:394–399. https://doi.org/10.1097/brs.0000000000000153
Nam DC, Lee HJ, Lee CJ, Hwang SC (2019) Molecular pathophysiology of ossification of the posterior longitudinal ligament (OPLL). Biomol Ther 27:342–348. https://doi.org/10.4062/biomolther.2019.043
Fujimori T, Watabe T, Iwamoto Y, Hamada S, Iwasaki M, Oda T (2016) Prevalence, concomitance, and distribution of ossification of the spinal ligaments: results of whole spine CT scans in 1500 Japanese patients. Spine 41(21):1668–1676
Li H, Dai L-Y (2011) A systematic review of complications in cervical spine surgery for ossification of the posterior longitudinal ligament. Spine J 11:1049–1057. https://doi.org/10.1016/j.spinee.2011.09.008
Nakashima H, Tetreault L, Nagoshi N, Nouri A, Arnold P, Yukawa Y, Toyone T, Tanaka M, Zhou Q, Fehlings MG (2016) Comparison of outcomes of surgical treatment for ossification of the posterior longitudinal ligament versus other forms of degenerative cervical myelopathy: results from the prospective, multicenter AOSpine CSM-international study of 479 patients. JBJS 98(5):370–378
Ramos MRD, Liu G, Tan J-H, Tan JHJ, Ruiz JNM, Hey HWD, Lau L-L, Kumar N, Thambiah J, Wong H-K (2021) Risk factors for surgical complications in the management of ossification of the posterior longitudinal ligament. Spine J 21:1176–1184. https://doi.org/10.1016/j.spinee.2021.03.022
O’Neill KR, Neuman BJ, Peters C, Riew KD (2014) Risk factors for dural tears in the cervical spine. Spine 39(17):E1015–E1020
Shou F, Li Z, Wang H, Yan C, Liu Q, Xiao C (2015) Prevalence of C5 nerve root palsy after cervical decompressive surgery: a meta-analysis. Eur Spine J 24:2724–2734. https://doi.org/10.1007/s00586-015-4186-5
Kato S, Chikuda H, Seichi A, Ohtsu H, Kimura A, Toyama Y (2012) Radiographical risk factors for major intraoperative blood loss during laminoplasty in patients with ossification of the posterior longitudinal ligament. Spine 37(25):E1588–E1593
Shah AA, Devana SK, Lee C, Kianian R, van der Schaar M, SooHoo NF (2021) Development of a novel, potentially universal machine learning algorithm for prediction of complications after total hip arthroplasty. J Arthroplasty 36:1655-1662.e1651. https://doi.org/10.1016/j.arth.2020.12.040
Alaa A, Schaar M (2018) AutoPrognosis: automated clinical prognostic modeling via bayesian optimization with structured kernel learning. In: Jennifer D, Andreas K (eds) Proceedings of the 35th International Conference on Machine Learning. PMLR, Proceedings of Machine Learning Research. pp. 139--148.
Shah AA, Devana SK, Lee C, Bugarin A, Lord EL, Shamie AN, Park DY, van der Schaar M, SooHoo NF (2021) Machine learning-driven identification of novel patient factors for prediction of major complications after posterior cervical spinal fusion. Eur Spine J. https://doi.org/10.1007/s00586-021-06961-7
LeCun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521:436–444. https://doi.org/10.1038/nature14539
Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, Yoshikawa H (2007) Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: part 1: clinical results and limitations of laminoplasty. Spine 32:647–653. https://doi.org/10.1097/01.brs.0000257560.91147.86
Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, Yoshikawa H (2007) Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: part 2: advantages of anterior decompression and fusion over laminoplasty. Spine 32:654–660. https://doi.org/10.1097/01.brs.0000257566.91177.cb
Tsuyama N (1984) Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res 71–84
Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda M, Okawa A, Takahashi K, Konishi H (2008) A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine 33:E990-993. https://doi.org/10.1097/BRS.0b013e318188b300
Veeravagu A, Connolly ID, Lamsam L, Li A, Swinney C, Azad TD, Desai A, Ratliff JK (2016) Surgical outcomes of cervical spondylotic myelopathy: an analysis of a national, administrative, longitudinal database. Neurosurg Focus FOC 40:E11. https://doi.org/10.3171/2016.3.FOCUS1669
DePasse JM, Durand W, Eltorai AEM, Palumbo MA, Daniels AH (2018) Timing of complications following posterior cervical fusion. J Orthop 15:522–526. https://doi.org/10.1016/j.jor.2018.03.010
Cruz JA, Wishart DS (2007) Applications of machine learning in cancer prediction and prognosis. Cancer Inf 2:59–77
Luo W, Phung D, Tran T, Gupta S, Rana S, Karmakar C, Shilton A, Yearwood J, Dimitrova N, Ho TB, Venkatesh S, Berk M (2016) Guidelines for developing and reporting machine learning predictive models in biomedical research: a multidisciplinary view. J Med Internet Res 18:e323. https://doi.org/10.2196/jmir.5870
Bakhsh W, Saleh A, Yokogawa N, Gruber J, Rubery PT, Mesfin A (2019) Cervical ossification of the posterior longitudinal ligament: a computed tomography-based epidemiological study of 2917 patients. Glob Spine J 9:820–825. https://doi.org/10.1177/2192568219833658
Kimura A, Takeshita K, Yoshii T, Egawa S, Hirai T, Sakai K, Kusano K, Nakagawa Y, Wada K, Katsumi K, Fujii K, Furuya T, Nagoshi N, Kanchiku T, Nagamoto Y, Oshima Y, Nakashima H, Ando K, Takahata M, Mori K, Nakajima H, Murata K, Matsunaga S, Kaito T, Yamada K, Kobayashi S, Kato S, Ohba T, Inami S, Fujibayashi S, Katoh H, Kanno H, Watanabe K, Imagama S, Koda M, Kawaguchi Y, Nakamura M, Matsumoto M, Yamazaki M, Okawa A (2021) Impact of diabetes mellitus on cervical spine surgery for ossification of the posterior longitudinal ligament. J Clin Med 10(21):5026. https://doi.org/10.3390/jcm10153375
Gianfrancesco MA, Tamang S, Yazdany J, Schmajuk G (2018) Potential biases in machine learning algorithms using electronic health record data. JAMA Intern Med 178:1544–1547. https://doi.org/10.1001/jamainternmed.2018.3763
Acknowledgements
This work was supported by Japanese Agency for Medical Research and Development (AMED) and Health and Labour Science Research Grants. This study was approved by each institutional review board.
Funding
This work was supported by a research grant funded by Japan Agency for Medical Research and Development Grant No. JP15ek0109136 and Japanese Health Labour Sciences Research Grant Number 40. No relevant financial activities outside the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Ethics approval
The study was approved by the Ethics Committee of Tokyo Medical and Dental University (M2000-1963).
Informed consent
The manuscript submitted does not contain information about medical device(s)/drug(s).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ito, S., Nakashima, H., Yoshii, T. et al. Deep learning-based prediction model for postoperative complications of cervical posterior longitudinal ligament ossification. Eur Spine J 32, 3797–3806 (2023). https://doi.org/10.1007/s00586-023-07562-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07562-2