Abstract
Objective
Anterior bone loss (ABL) was considered as a non-progressive process secondary only to motion-preserving implant and has been noticed recently in cervical disk replacement (CDR) let alone patients with anterior cervical diskectomy and fusion (ACDF). Our purpose is to reveal this unnoticed phenomenon in ACDF and further explore its clinical and radiological outcomes.
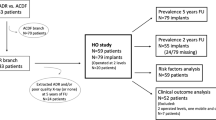
Methods
A total of 77 patients underwent ACDF with a minimum follow-up of at least one year were retrospectively reviewed. The average follow-up time was 22.51 ± 16.31 months. There were 50 patients in group A with ABL, while there were 27 patients in group B without ABL. ABL was measured and classified into four grades according to Kieser’s methods. Clinical evaluation, radiological parameters and fusion rate were recorded.
Results
The incidence of bone ABL was 64.9% of Zero-P and 55.2% of endplates. The incidence of upper and lower endplates was 61% and 49%, respectively, and such difference was not significant. Mild ABL occurred in 22%, moderate ABL in 38% and severe ABL of 40% patients underwent ACDF with ABL. ABL would not affect both clinical outcomes and fusion rate. However, ABL would result in a higher incidence of subsidence.
Conclusion
ABL should be considered as a common phenomenon that both CDR and ACDF owned a non-progressive process which confined in one year. ABL would result in a higher incidence of subsidence. Luckily, this phenomenon does not have an effect on postoperative clinical and fusion rate.








Similar content being viewed by others
Data availability
Datasets are available from the corresponding author on reasonable request.
Abbreviations
- CDR:
-
Cervical disk replacement
- ACDF:
-
Anterior cervical diskectomy and fusion
- JOA:
-
Japanese orthopedic association
- NDI:
-
Neck disability index
- VAS:
-
Visual analog scale
- Cobb C:
-
Overall Cobb angle
- Cobb S:
-
Segmental Cobb angle
- LE:
-
Length of endplate
- CDDD:
-
Cervical degenerative disk disease
- ASD:
-
Adjacent segment degeneration
- HO:
-
Heterotopic ossification
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
References
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40:607–624
Cloward RB (1958) The anterior approach for removal of ruptured cervical discs. J Neurosurg 15:602–617
Zhao Y, Yang S, Huo Y et al (2020) Locking stand-alone cage versus anterior plate construct in anterior cervical discectomy and fusion: a systematic review and meta-analysis based on randomized controlled trials. Eur Spine J 29(11):2734–2744
Lin W, Ha A, Boddapati V, Riew KD et al (2018) Diagnosing pseudoarthrosis after anterior cervical discectomy and fusion. Neurospine 15(3):194–205
Njoku I, Alimi M, Leng LZ et al (2014) Anterior cervical discectomy and fusion with a zero-profile integrated plate and spacer device: a clinical and radiological study: clinical article. J Neurosurg Spine 21(4):529–537. https://doi.org/10.3171/2014.6.SPINE12951
Deng YF, Meng Y, Liu H et al (2020) Space between the titanium plate of zero-profile cage and endplate of the vertebral body might affect the fusion process in anterior cervical discectomy and fusion. Chin Med J (Engl). 133(21):2641–2643
Kim SH, Chung YS, Ropper AE et al (2015) Bone loss of the superior adjacent vertebral body immediately posterior to the anterior flange of Bryan cervical disc. Eur Spine J 24(12):2872–2879. https://doi.org/10.1007/s00586-015-3849-6
Wang XF, Meng Y, Liu H et al (2020) Anterior bone loss after cervical disc replacement: A systematic review. World J Clin Cases 8(21):5284–5295. https://doi.org/10.12998/wjcc.v8.i21.5284
Kieser DC, Cawley DT, Fujishiro T, Tavolaro C, Mazas S, Boissiere L et al (2018) Risk factors for anterior bone loss in cervical disc arthroplasty. J Neurosurg Spine 29(2):123–129. https://doi.org/10.3171/2018.1.SPINE171018
Heo DH, Lee DC, Oh JY, Park CK (2017) Bone loss of vertebral bodies at the operative segment after cervical arthroplasty: a potential complication? Neurosurg Focus 42(2):E7. https://doi.org/10.3171/2016.10.FOCUS16393
Takeshita K, Murakami M, Kobayashi A, Nakamura C (2001) Relationship between cervical curvature index (Ishihara) and cervical spine angle (C2–7). J Orthop Sci 6:223–226. https://doi.org/10.1007/s007760100038
Vasso M, Beaufils P, Cerciello S, Schiavone PA (2014) Bone loss following knee arthroplasty: potential treatment options. Arch Orthop Trauma Surg 134:543–553. https://doi.org/10.1007/s00402-014-1941-8
Lerch M, von der Haar-Tran A, Windhagen H et al (2012) Bone remodelling around the Metha short stem in total hip arthroplasty: a prospective dual-energy X-ray absorptiometry study. Int Orthop 36(3):533–538. https://doi.org/10.1007/s00264-011-1361-0
Gallo J, Goodman SB, Konttinen YT, Wimmer MA, Holinka M (2013) Osteolysis around total knee arthroplasty: a review of pathogenic mechanisms. Acta Biomater 9(9):8046–8058. https://doi.org/10.1016/j.actbio.2013.05.005
Veruva SY, Lanman TH, Hanzlik JA, Kurtz SM, Steinbeck MJ (2015) Rare complications of osteolysis and periprosthetic tissue reactions after hybrid and non-hybrid total disc replacement. Eur Spine J 24:S494–S501. https://doi.org/10.1007/s00586-014-3535-0
Tumialan LM, Gluf WM (2011) Progressive vertebral body osteolysis after disc arthroplasty. Spine 36(14):E973–E978. https://doi.org/10.1097/BRS.0b013e3181fd863b
Veruva SY, Lanman TH, Hanzlik JA, Kurtz SM, Steinbeck MJ (2015) Rare complications of osteolysis and periprosthetic tissue reactions after hybrid and non-hybrid total disc replacement. Eur Spine J 24(Suppl 4):S494–S501. https://doi.org/10.1007/s00586-014-3535-0
Hacker FM, Babcock RM, Hacker RJ (2013) Very late complications of cervical arthroplasty: : results of 2 controlled randomized prospective studies from a single investigator site. Spine 38(26):2223–2226. https://doi.org/10.1097/BRS.0000000000000060
Fraser JF, Werner S, Jacofsky DJ (2015) Wear and loosening in total knee arthroplasty: a quick review. J Knee Surg 28:139–144. https://doi.org/10.1055/s-0034-1398375
Chen CM, Tsai WC, Lin SC, Tseng CS (2014) Effects of stemmed and nonstemmed hip replacement on stress distribution of proximal femur and implant. BMC Musculoskelet Disord 15:312. https://doi.org/10.1186/1471-2474-15-312
Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP (2009) The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine 34(26):2886–2892. https://doi.org/10.1097/BRS.0b013e3181b64f2c
Wang X, Meng Y, Liu H et al (2020) Is anterior bone loss the opposite of anterior heterotopic ossification in Prestige-LP cervical disc replacement? World Neurosurg 136:e407–e418. https://doi.org/10.1016/j.wneu.2020.01.022
Chen H, Zhong J, Tan J, Wu D, Jiang D (2013) Sagittal geometry of the middle and lower cervical endplates. Eur Spine J 22:1570–1575. https://doi.org/10.1007/s00586-013-2791-8
Dunbar L, Vidakovic H, Löffler S, Hammer N, Gille O (2019) Anterior cervical spine blood supply: a cadaveric study. Surg radiol anat 41(6):607–611. https://doi.org/10.1007/s00276-019-02236-5
Acknowledgements
We thank the nursing staffs from our department and the patients enrolled in this study for their supports.
Funding
This study was supported by the 135 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYJC18029), Sichuan Province Science and Technology Support Program of China (NO. 2020YFS0077), Post-Doctor Research Project, West China Hospital, Sichuan University (NO. 2019HXBH063), Postdoctoral Science Foundation of China (NO. 2020M673240) and the West China Nursing Discipline Development Special Fund Project. (NO. HXHL19016 to Ying Hong). No relevant financial activities outside of the submitted work.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare they have no competing interests.
Ethical approval
This study approved by the Institutional Review Board of West China Hospital. Informed consent was obtained from all individual participants included in this study.
Consent for publication
Informed consent was obtained from all individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deng, Y., Wang, B., Hong, Y. et al. Anterior bone loss: A common phenomenon which should be considered as bone remodeling process existed not only in patients underwent cervical disk replacement but also those with anterior cervical diskectomy and fusion. Eur Spine J 32, 977–985 (2023). https://doi.org/10.1007/s00586-022-07504-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07504-4