Abstract
Purpose
Bone graft extenders have been developed to prevent donor site morbidity associated with iliac crest bone graft, but few studies compared the efficacy of various substitutes. Our purpose was to determine fusion rate and clinical outcome in patients undergoing lumbar arthrodesis using demineralized bone matrix (DBM) and biphasic calcium phosphate (BCP).
Methods
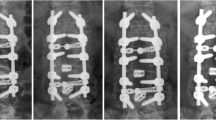
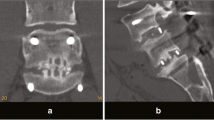
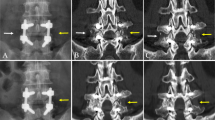
Patients with degenerative spondylolisthesis undergoing one-level or two-level arthrodesis of lumbar spine were retrospectively reviewed. Two treatment groups placed either BCP or DBM, in addition to local autograft in lumbar posterolateral space. Three-dimensional CT exam and dynamic flexion–extension radiographs at postoperative 2-year were assessed for posterolateral fusion status and pain scale and Oswestry Disability Index (ODI) for clinical outcome.
Results
Of the 148 patients reviewed (including 23 in one- and 58 patients in two-level in BCP group, and 47 in one- and 20 patients in two-level in DBM group), no significant differences were found in terms of age, sex, BMI, smoking, diabetes, steroids, number of level fused, non-union rate or revision surgery between BCP and DBM groups. Significantly improved pain scale of back and leg and ODI were found in both groups postoperatively without group difference. We found a comparable fusion rate in one-level surgery (100% versus 93.6%) and a superior fusion rate of BCP group in two-level surgery (98.3% versus 80.0%, p = 0.01).
Conclusion
Being a bone graft extender without osteoinductive property, with local autograft, BCP is comparable to DBM for one- and superior for two-level fusion. No significant difference was found in clinical outcomes.




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available in the electronic supplementary material.
References
Cammisa FP Jr, Lowery G, Garfin SR, Geisler FH, Klara PM, McGuire RA, Sassard WR, Stubbs H, Block JE (2004) Two-year fusion rate equivalency between Grafton DBM gel and autograft in posterolateral spine fusion: a prospective controlled trial employing a side-by-side comparison in the same patient. Spine (Phila Pa 1976) 29(6):660–666
Rihn JA, Kirkpatrick K, Albert TJ (2010) Graft options in posterolateral and posterior interbody lumbar fusion. Spine (Phila Pa 1976) 35(17):1629–1639. https://doi.org/10.1097/BRS.0b013e3181d25803
Ortega B, Gardner C, Roberts S, Chung A, Wang JC, Buser Z (2020) Ceramic biologics for bony fusion-a journey from first to third generations. Curr Rev Musculoskelet Med 13(4):530–536. https://doi.org/10.1007/s12178-020-09651-x
Peterson B, Whang PG, Iglesias R, Wang JC, Lieberman JR (2004) Osteoinductivity of commercially available demineralized bone matrix. Preparations in a spine fusion model. J Bone Joint Surg Am 86(10):2243–2250. https://doi.org/10.2106/00004623-200410000-00016
Morris MT, Tarpada SP, Cho W (2018) Bone graft materials for posterolateral fusion made simple: a systematic review. Eur Spine J 27(8):1856–1867. https://doi.org/10.1007/s00586-018-5511-6
Kang J, An H, Hilibrand A, Yoon ST, Kavanagh E, Boden S (2012) Grafton and local bone have comparable outcomes to iliac crest bone in instrumented single-level lumbar fusions. Spine (Phila Pa 1976) 37(12):1083–1091. https://doi.org/10.1097/BRS.0b013e31823ed817
Nickoli MS, Hsu WK (2014) Ceramic-based bone grafts as a bone grafts extender for lumbar spine arthrodesis: a systematic review. Global Spine J 4(3):211–216. https://doi.org/10.1055/s-0034-1378141
Pugely AJ, Petersen EB, DeVries-Watson N, Fredericks DC (2017) Influence of 45S5 bioactive glass in a standard calcium phosphate collagen bone graft substitute on the posterolateral fusion of rabbit spine. Iowa Orthop J 37:193–198
Plantz MA, Gerlach EB, Hsu WK (2021) Synthetic bone graft materials in spine fusion: current evidence and future trends. Int J Spine Surg 15(s1):104–112. https://doi.org/10.14444/8058
Ricart PH, Gandhi SD, Geisinger J, Baker K, Park DK (2018) Clinical and CT analysis of lumbar spine arthrodesis: beta-tricalcium phosphate versus demineralized bone matrix. J Am Acad Orthop Surg Glob Res Rev 2(9):e024. https://doi.org/10.5435/JAAOSGlobal-D-18-00024
Yi J, Lee GW, Nam WD, Han KY, Kim MH, Kang JW, Won J, Kim SW, Noh W, Yeom JS (2015) A prospective randomized clinical trial comparing bone union rate following anterior cervical discectomy and fusion using a polyetheretherketone cage: hydroxyapatite/B-tricalcium phosphate mixture versus hydroxyapatite/demineralized bone matrix mixture. Asian Spine J 9(1):30–38. https://doi.org/10.4184/asj.2015.9.1.30
Feng JT, Yang XG, Wang F, He X, Hu YC (2020) Efficacy and safety of bone substitutes in lumbar spinal fusion: a systematic review and network meta-analysis of randomized controlled trials. Eur Spine J 29(6):1261–1276. https://doi.org/10.1007/s00586-019-06257-x
Lenke LG, Bridwell KH, Bullis D, Betz RR, Baldus C, Schoenecker PL (1992) Results of in situ fusion for isthmic spondylolisthesis. J Spinal Disord 5(4):433–442. https://doi.org/10.1097/00002517-199212000-00008
Brodsky AE, Kovalsky ES, Khalil MA (1991) Correlation of radiologic assessment of lumbar spine fusions with surgical exploration. Spine (Phila Pa 1976) 16(6 Suppl):S261-265. https://doi.org/10.1097/00007632-199106001-00017
Choudhri TF, Mummaneni PV, Dhall SS, Eck JC, Groff MW, Ghogawala Z, Watters WC 3rd, Dailey AT, Resnick DK, Sharan A, Wang JC, Kaiser MG (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 4: radiographic assessment of fusion status. J Neurosurg Spine 21(1):23–30. https://doi.org/10.3171/2014.4.spine14267
Walsh WR, Vizesi F, Cornwall GB, Bell D, Oliver R, Yu Y (2009) Posterolateral spinal fusion in a rabbit model using a collagen-mineral composite bone graft substitute. Eur Spine J 18(11):1610–1620. https://doi.org/10.1007/s00586-009-1034-5
Aghdasi B, Montgomery SR, Daubs MD, Wang JC (2013) A review of demineralized bone matrices for spinal fusion: the evidence for efficacy. Surgeon 11(1):39–48. https://doi.org/10.1016/j.surge.2012.08.001
Chang DG, Park JB, Han Y (2021) Surgical outcomes of two kinds of demineralized bone matrix putties/local autograft composites in instrumented posterolateral lumbar fusion. BMC Musculoskelet Disord 22(1):200. https://doi.org/10.1186/s12891-021-04073-3
Atici T, Yerebakan S, Ermutlu C, Özyalçın A (2020) Augmenting posterolateral fusion with transforaminal lumbar interbody fusion cage improves clinical outcome, but not fusion rate, of posterior decompression. J Int Med Res 48(4):300060520910025. https://doi.org/10.1177/0300060520910025
Macki M, Bydon M, Weingart R, Sciubba D, Wolinsky JP, Gokaslan ZL, Bydon A, Witham T (2015) Posterolateral fusion with interbody for lumbar spondylolisthesis is associated with less repeat surgery than posterolateral fusion alone. Clin Neurol Neurosurg 138:117–123. https://doi.org/10.1016/j.clineuro.2015.08.014
Liu XY, Wang YP, Qiu GX, Weng XS, Yu B (2014) Meta-analysis of circumferential fusion versus posterolateral fusion in lumbar spondylolisthesis. J Spinal Disord Tech 27(8):E282-293. https://doi.org/10.1097/bsd.0000000000000116
Plantz MA, Hsu WK (2020) Single-level posterolateral fusion (PLF) alone and posterior interbody fusion (PLIF/TLIF) alone lead to a decreased risk of short-term complications compared to combined PLF with PLIF/TLIF procedures: a matched analysis. Spine (Phila Pa 1976) 45(21):E1391-e1399. https://doi.org/10.1097/brs.0000000000003615
Gaffney CJ, Pinto MR, Buyuk AF, Garvey TA, Mueller B, Schwender JD, Transfeldt EE, Tam HK, Dawson JM (2019) Posterolateral versus transforaminal interbody L4/5 fusion: correlation with subsequent surgery. Clin Spine Surg 32(2):E91-e98. https://doi.org/10.1097/bsd.0000000000000733
Ozalay M, Sahin O, Akpinar S, Ozkoc G, Cinar M, Cesur N (2009) Remodeling potentials of biphasic calcium phosphate granules in open wedge high tibial osteotomy. Arch Orthop Trauma Surg 129(6):747–752. https://doi.org/10.1007/s00402-008-0781-9
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Ethical review committee statement: this retrospective study with Ref. No. 201901144B0 was approved with informed consent waiver by the Chang Gung Memorial Hospital Institutional Review Board (CGMH IRB, Linkou, Taiwan).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, CA., Chen, WC., Lu, ML. et al. Use of biphasic calcium phosphate versus demineralized bone matrix: retrospective clinical and CT analysis of posterolateral fusion results. Eur Spine J 32, 734–742 (2023). https://doi.org/10.1007/s00586-022-07499-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07499-y