Abstract
Purpose
To assess the risk of developing thoracogenic scoliosis (THS) in paediatric patients, depending on the side of lateral thoracotomy (LT) and of spine deviation in the coronal plane by means of logistic regression and scoliosis-free survival analyses.
Methods
A total of 307 consecutive patients undergoing LT were retrospectively reviewed; 32 patients met the inclusion criteria: 1) underwent LT and developed THS; 2) age < 15 years at LT; 3) clinical and radiographic follow-up ≥ 5 years. Patients were divided into ipsilateral group (convexity ipsilateral to LT) and contralateral group (convexity contralateral to LT).
Results
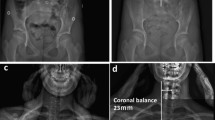
The mean follow-up was 10 ± 4.7 in the ipsilateral group (n = 13) and 12 ± 4.8 years in the contralateral group (n = 19). The contralateral group underwent LT at a younger age (4.4 vs 6.4 years, p = 0.55), developed more severe coronal deformity (27.8° vs 18.9°, p = 0.15), had higher rate of THS > 20° (47.5% vs 38.4%; p = 0.34) and > 45° (21.1% vs 0%; p = 0.99). The mean time from LT to THS diagnosis was 4.2 ± 2.9 in ipsilateral group and 5.5 ± 4.2 years in contralateral group. Left-side LT (p = 0.03) and age > 5 years (p = 0.01) showed a lower risk of THS diagnosis. The group variable had a statistically significant effect on the risk of developing THS > 45° (p = 0.03).
Conclusion
In this series, children that developed THS with a convexity contralateral to the side of LT had more severe and progressive coronal spine deformity.
Level of evidence:
III




Similar content being viewed by others
References
SRS Revised Glossary of Terms. https://www.srs.org/professionals/online-education-and-resources/glossary/revised-glossary-of-terms
Bisgard JD (1939) Thoracogenic scoliosis: influence of thoracic disease and thoracic operations on the spine. Arch Surg 29(3):417–445. https://doi.org/10.1001/archsurg.1934.01180030082006
Eby SF, Hilaire TS, Glotzbecker M et al (2018) Thoracogenic spinal deformity: a rare cause of early-onset scoliosis. J Neurosurg Spine 29(6):674–679. https://doi.org/10.3171/2018.4.SPINE171389
Sacco R, Bonnevalle M, Nectoux E et al (2022) Thoracogenic scoliosis: a retrospective review of 129 pediatric patients with a mean follow-up of 10 years. Eur Spine J. https://doi.org/10.1007/s00586-022-07242-7
DeRosa GP (1985) Progressive scoliosis following chest wall resection in children. Spine 10:618–622. https://doi.org/10.1097/00007632-198509000-00005
Glotzbecker MP, Gold M, Puder M, Hresko MT (2013) Scoliosis after chest wall resection. J Child Orthop 7(4):301–307. https://doi.org/10.1007/s11832-013-0519-2
Cobb J (1948) Outline for the study of scoliosis. Instr Course Lect 5:261–275
Weinstein SL, Dolan LA, Cheng JC et al (2008) Adolescent Idiopathic scoliosis. Lancet 371(9623):1527–1537. https://doi.org/10.1016/S0140-6736(08)60658-3
Mehta MH (1972) The rib-vertebra angle in the early diagnosis between resolving and progressive infantile scoliosis. J Bone Joint Surg Br 54(2):230–243
Canavese F, Holveck J, De Coulon G, Kaelin A (2011) Analysis of concave and convex rib-vertebral angle, angle difference, and angle ratio in patients with lenke type 1 main thoracic adolescent idiopathic scoliosis treated by observation, brag or posterior fusion, and instrumentation. J Spinal Disord Tech 24(8):506–513. https://doi.org/10.1097/BSD.0b013e31820644b4
Canavese F, Turcot K, Holveck J, Farhoumand AD, Kaelin A (2011) Changes of concave and convex rib-vertebral angle, angle difference and angle ratio in patients with right thoracic adolescent idiopathic scoliosis. Eur Spine J 20(1):129–134. https://doi.org/10.1007/s00586-010-1563-y
Nash CL Jr, Moe JH (1969) A study of vertebral rotation. J Bone Joint Surg Am 51(2):223–229
Illés TS, Lavaste F, Dubousset JF (2019) The third dimension of scoliosis: the forgotten axial plane. Orthop Traumatol Surg Res 105(2):351–359. https://doi.org/10.1016/j.otsr.2018.10.021
Dimeglio A, Canavese F (2012) The growing spine: how spinal deformities influence normal spine and thoracic cage growth. Eur Spine J 21(1):64–70. https://doi.org/10.1007/s00586-011-1983-3
Dimeglio A, Canavese F (2013) Progression or not progression? how to deal with adolescent idiopathic scoliosis during puberty. J Child Orthop 7(1):43–49. https://doi.org/10.1007/s11832-012-0463-6
Bastard F, Bonnard A, Rousseau V et al (2018) Thoracic skeletal anomalies following surgical treatment of esophageal atresia lessons from a national cohort. J Pediatr Surg 53(4):605–609. https://doi.org/10.1016/j.jpedsurg.2017.07.01
Gilsanz V, Boechat IM, Birnberg FA et al (1983) Scoliosis after thoracotomy for esophageal atresia. AJR Am J Roentgenol 141(3):457–460. https://doi.org/10.1007/s00383-020-04683-3
Westfelt JN, Nordwall A (1991) Thoracotomy and scoliosis. Spine 16:1124–1125. https://doi.org/10.1097/00007632-199109000-00019
Sistonen SJ, Helenius I, Peltonen J et al (2009) Natural history of spinal anomalies and scoliosis associated with esophageal atresia. Pediatrics 124(6):e1198–e1204. https://doi.org/10.1542/peds.2008-3704
Jacobsen S, Rosenklint A, Halkier E (1974) Post-pneumonectomy scoliosis. Acta Orthop Scand 45(6):867–872. https://doi.org/10.3109/17453677408989697
Bal S, Elshershari H, Celiker R et al (2003) Thoracic sequels after thoracotomies in children with congenital cardiac disease. Cardiol Young 13(3):264–267
Jaureguizar E, Vázquez J, Murcia J et al (1985) Morbid musculoskeletal sequelae of thoracotomy for tracheoesophageal fistula. J Pediatr Surg 20(5):511–514. https://doi.org/10.1016/s0022-3468(85)80477-2
Makita S, Kaneko K, Ono Y et al (2017) Risk factors for thoracic and spinal deformities following lung resection in neonates, infants, and children. Surg Today 47(7):810–814. https://doi.org/10.1007/s00595-016-1434-1
Mishra PR, Tinawi GK, Stringer MD (2020) Scoliosis after thoracotomy repair of esophageal atresia: a systematic review. Pediatr Surg Int 36(7):755–761. https://doi.org/10.1007/s00383-020-04683-3
Van Biezen FC, Bakx PA, De Villeneuve VH et al (1993) Scoliosis in children after thoracotomy for aortic coarctation. J Bone Joint Surg Am 75(4):514–518. https://doi.org/10.2106/00004623-199304000-00006
Durning RP, Scoles PV, Fox OD (1980) Scoliosis after thoracotomy in tracheoesophageal fistula patients. a follow-up study. J Bone Joint Surg Am 62(7):1156–1159
Roclawski M, Sabiniewicz R, Potaz P et al (2009) Scoliosis in patients with aortic coarctation and patent ductus arteriosus: does standard posterolateral thoracotomy play a role in the development of the lateral curve of the spine? Pediatr Cardiol 30(7):941–945. https://doi.org/10.1007/s00246-009-9469-3
Lawal TA, Gosemann JH, Kuebler JF et al (2008) Thoracoscopy versus thoracotomy improves midterm musculoskeletal status and cosmesis in infants and children. Ann Thorac Surg 87(1):224–228. https://doi.org/10.1016/j.athoracsur.2008.08.069
Funding
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Manuscript preparation, data collection and analysis were performed by RS and FC. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Authors have declare no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of the Jeanne de Flandre Hospital of Lille.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sacco, R., Ould-Slimane, M., Bonnevalle, M. et al. Thoracogenic scoliosis: coronal deformity progression in paediatric patients. Eur Spine J 32, 639–650 (2023). https://doi.org/10.1007/s00586-022-07498-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07498-z