Abstract
Purpose
It is sometimes anticipated that patients with prior spine surgery will have a compromised outcome from future procedures. The purpose of this study was to compare TDR outcomes in patients with prior lumbar spine surgery to those with no previous surgery.
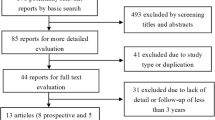
Methods
Post hoc analysis was performed on 5-year follow-up data collected prospectively in the multi-centre FDA-regulated trial for the activL® Artificial Disc which involved 376 patients treated for single-level symptomatic disc degeneration. Clinical outcome measures included the Oswestry Disability Index (ODI), visual analog scales (VAS) assessing back and leg pain, SF-36, adverse events, and re-operations. Radiographic outcomes included flexion/extension range of motion (ROM) and translation of the operated segment. Patients were divided into two groups: Prior Lumbar Surgery (PLS, n = 92) and No Prior Lumbar Surgery (NPLS, n = 284).
Results
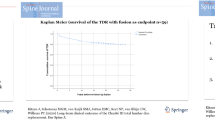
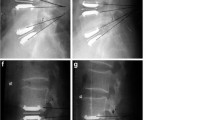
Baseline demographics were similar in the two groups. ODI, VAS, and SF-36 Physical Component Scale scores improved significantly (p < 0.05) from baseline in both groups with improvements maintained through 5-year post-TDR with no significant differences between groups. There were no statistically significant differences in rates of serious device-related events, procedure-related events, or re-operations. While ROM was significantly less prior to TDR surgery in the PLS group, there was no significant difference in ROM at post-operative points.
Conclusion
Prior lumbar spine surgery was not associated with compromised outcomes following TDR. These results are in line with reports from earlier studies with shorter follow-up, finding that non-destabilizing prior surgery is not a contra-indication for TDR provided that selection criteria are met.
Level of Evidence I
Diagnostic: individual cross-sectional studies with the consistently applied reference standard and blinding.





Similar content being viewed by others
References
Blumenthal S, McAfee PC, Guyer RD, Hochschuler SH, Geisler FH, Holt RT, Garcia R Jr, Regan JJ, Ohnmeiss DD (2005) A prospective, randomized, multicenter food and drug administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part i: evaluation of clinical outcomes. Spine 30(14):1565–1575. https://doi.org/10.1097/01.brs.0000170587.32676.0e
Guyer RD, McAfee PC, Banco RJ, Bitan FD, Cappuccino A, Geisler FH, Hochschuler SH, Holt RT, Jenis LG, Majd ME, Regan JJ, Tromanhauser SG, Wong DC, Blumenthal SL (2009) Prospective, randomized, multicenter food and drug administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: five-year follow-up. Spine J 9(5):374–386
Zigler JE, Delamarter RB (2012) Five-year results of the prospective, randomized, multicenter, food and drug administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential arthrodesis for the treatment of single-level degenerative disc disease. J Neurosurg Spine 17(6):493–501. https://doi.org/10.3171/2012.9.SPINE11498
Gornet MF, Burkus JK, Dryer RF, Peloza JH, Schranck FW, Copay AG (2019) Lumbar disc arthroplasty versus anterior lumbar interbody fusion: 5-year outcomes for patients in the Maverick disc investigational device exemption study. J Neurosurg Spine 31(3):347–356. https://doi.org/10.3171/2019.2.spine181037
Garcia R Jr, Yue JJ, Blumenthal S, Coric D, Patel VV, Leary SP, Dinh DH, Buttermann GR, Deutsch H, Girardi F, Billys J, Miller LE (2015) Lumbar total disc replacement for discogenic low back pain: 2-year outcomes of the activl multicenter randomized controlled IDE clinical trial. Spine 40(24):1873–1881. https://doi.org/10.1097/BRS.0000000000001245
Guyer RD, Pettine K, Roh JS, Dimmig TA, Coric D, McAfee PC, Ohnmeiss DD (2014) Comparison of 2 lumbar total disc replacements: results of a prospective, randomized, controlled multicenter food and drug administration trial with 24-month follow-up. Spine 39(12):925–931. https://doi.org/10.1097/BRS.0000000000000319
Zigler J, Delamarter R, Spivak JM, Linovitz RJ, Danielson GO 3rd, Haider TT, Cammisa F, Zuchermann J, Balderston R, Kitchel S, Foley K, Watkins R, Bradford D, Yue J, Yuan H, Herkowitz H, Geiger D, Bendo J, Peppers T, Sachs B, Girardi F, Kropf M, Goldstein J (2007) Results of the prospective, randomized, multicenter food and drug administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine 32(11):1155–1162. https://doi.org/10.1097/BRS.0b013e318054e377
Gornet MF, Burkus JK, Dryer RF, Peloza JH (2011) Lumbar disc arthroplasty with MAVERICK Disc versus stand-alone interbody fusion: a prospective, randomized, controlled, multicenter investigational device exemption trial. Spine 36(25):E1600–E1611. https://doi.org/10.1097/BRS.0b013e318217668f
Geisler FH, Guyer RD, Blumenthal SL, McAfee PC, Cappuccino A, Bitan F, Regan JJ (2008) Effect of previous surgery on clinical outcome following 1-level lumbar arthroplasty. J Neurosurg Spine 8(2):108–114. https://doi.org/10.3171/SPI/2008/8/2/108
Leahy M, Zigler JE, Ohnmeiss DD, Rashbaum RF, Sachs BL (2008) Comparison of results of total disc replacement in postdiscectomy patients versus patients with no previous lumbar surgery. Spine 33(15):1690–1693. https://doi.org/10.1097/BRS.0b013e31817bd2f0
Blondel B, Tropiano P, Gaudart J, Marnay T (2011) Clinical results of total lumbar disc replacement regarding to various aetiologies of the disc degeneration: a study with a 2 years minimal follow-up. Spine 36(5):E313–E319. https://doi.org/10.1097/BRS.0b013e3181dfbc4e
Li YZ, Sun P, Chen D, Tang L, Chen C, Wu AM (2020) Artificial total disc replacement versus fusion for lumbar degenerative disc disease: an update systematic review and meta-analysis. Turk Neurosurg 30(1):1–10. https://doi.org/10.5137/1019-5149.jtn.24799-18.2
Bai DY, Liang L, Zhang BB, Zhu T, Zhang HJ, Yuan ZG, Chen YF (2019) Total disc replacement versus fusion for lumbar degenerative diseases—a meta-analysis of randomized controlled trials. Medicine 98(29):e16460. https://doi.org/10.1097/md.0000000000016460
Bertagnoli R, Yue JJ, Fenk-Mayer A, Eerulkar J, Emerson JW (2006) Treatment of symptomatic adjacent-segment degeneration after lumbar fusion with total disc arthroplasty by using the prodisc prosthesis: a prospective study with 2-year minimum follow up. J Neurosurg Spine 4(2):91–97. https://doi.org/10.3171/spi.2006.4.2.91
Hähnle UR, Sliwa K, Weinberg IR, Sweet BMBE, de Villiers M, Candy GP (2007) Lumbar disc replacement for junctional decompensation after fusion surgery: clinical and radiological outcome at an average follow-up of 33 months. SAS J 1(3):83–95. https://doi.org/10.1016/SASJ-2007-0006-RR
Zehnder P, Aghayev E, Fekete TF, Haschtmann D, Pigott T, Mannion AF (2016) Influence of previous surgery on patient-rated outcome after surgery for degenerative disorders of the lumbar spine. Eur Spine J 25(8):2553–2562. https://doi.org/10.1007/s00586-016-4383-x
Guyer RD, Patterson M, Ohnmeiss DD (2006) Failed back surgery syndrome: diagnostic evaluation. J Am Acad Orthop Surg 14(9):534–543. https://doi.org/10.5435/00124635-200609000-00003
Block A, Ohnmeiss D, Ben-Porath YS, Burchett D (2011) Presurgical psychological screening: a new algorithm, including the MMPI-2-RF, for predicting surgery results. Spine J 11(10):S137–S138. https://doi.org/10.1016/j.spinee.2011.08.333
Marek RJ, Block AR, Ben-Porath YS (2017) Validation of a psychological screening algorithm for predicting spine surgery outcomes. Assessment 26(5):915–928. https://doi.org/10.1177/1073191117719512
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Conflict of interest statement None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Blumenthal, S.L., Guyer, R.D., Zigler, J.E. et al. Impact of previous lumbar spine surgery on the outcome of lumbar total disc replacement: analysis of prospective 5-year follow-up study data. Eur Spine J 32, 797–802 (2023). https://doi.org/10.1007/s00586-022-07492-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07492-5