Abstract
Purpose
To investigate, through a systematic review, the impact of the waiting time for Adolescent Idiopathic Scoliosis (AIS) surgical correction from the point of view of deformity evolution, treatment cost, and quality of life.
Methods
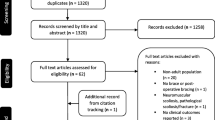
PubMed, Embase, LILACS, SciELO, Scopus, Web of Science, LIVIVO, and Cochrane Library databases were searched by two researchers to select the articles. The eligibility criteria were: Patients diagnosed with AIS with indication for surgical correction and submitted to waiting lists until treatment. The risks of bias were evaluated using the Risk Of Bias In Non-randomized Studies—Interventions (ROBINS-I) tool, and the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system was used to classify the level of the evidence for each outcome. The summary of the available evidence is presented in a narrative synthesis.
Results
Six observational studies were included. In a Canadian study, the primary outcome was the need for additional spine surgery in patients who had to wait more than three months due to spine deformity progression. American researchers presented a sample of premenarcheal and skeletally immature patients with AIS showing increased Cobb angle and attributed this to a six-month waiting for the surgical treatment. Another study included 177 patients with AIS with a mean waiting time of 225.7 days. There was a worsening average of 7.7° ± 8.6° in Cobb angle, and there was a change in surgical plan in 28 patients, which increased surgical time. Studies that evaluated the treatment cost showed significantly higher mean costs in those who waited longer than six months. Regarding the quality of life, while waiting for surgery, a retrospective study found that patients who underwent surgery earlier showed better results in a questionnaire that assessed their quality of life compared to those who were still waiting.
Conclusion
Observational studies show that, in individuals who are on waiting lists for AIS surgery, there is a worsening of the spinal deformity (substantial evidence), an increasing cost of treatment (moderate evidence) and it may negatively impact patients' quality of life (insufficient evidence). Performing better methodological quality studies to investigate these outcomes can violate good research practices since randomized clinical trials on this subject have ethical limitations to be carried out.
Trial registration
The authors declare that the systematic review protocol was registered at the international prospective register of systematic reviews (PROSPERO), CRD42020212134, and it was accepted for publication.


Similar content being viewed by others
References
Weinstein SL (2019) The natural history of adolescent idiopathic scoliosis. J Pediatr Orthop 39:S44–S46. https://doi.org/10.1097/BPO.0000000000001350
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371(9623):1527–1537. https://doi.org/10.1016/S0140-6736(08)60658-3
Yaman O, Dalbayrak S (2014) Idiopathic scoliosis. Turk Neurosurg 24(5):646–657. https://doi.org/10.5137/1019-5149.JTN.8838-13.0
Picault C, deMauroy JC, Mouilleseaux B, Diana G (1986) Natural history of idiopathic scoliosis in girls and boys. Spine 11(8):777–778. https://doi.org/10.1097/00007632-198610000-00004
Bunnell WP (1986) The natural history of idiopathic scoliosis before skeletal maturity. Spine 11(8):773–776. https://doi.org/10.1097/00007632-198610000-00003
Weinstein SL, Ponseti IV (1983) Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 65(4):447–455
Peterson LE, Nachemson AL (1995) Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. logistic regression analysis based on data from the brace study of the scoliosis research society. J Bone Joint Surg Am 77(6):823–7
Jada A, Mackel CE, Hwang SW, Samdani AF, Stephen JH, Bennett JT, Baaj AA (2017) Evaluation and management of adolescent idiopathic scoliosis: a review. Neurosurg Focus 43(4):E2. https://doi.org/10.3171/2017.7.FOCUS17297
Dickson JH, Mirkovic S, Noble PC, Nalty T, Erwin WD (1995) Results of operative treatment of idiopathic scoliosis in adults. J Bone Joint Surg Am 77(4):513–523. https://doi.org/10.2106/00004623-199504000-00003
Danielsson AJ (2013) Natural history of adolescent idiopathic scoliosis: a tool for guidance in decision of surgery of curves above 50°. J Child Orthop 7(1):37–41. https://doi.org/10.1007/s11832-012-0462-7
Bridwell KH, Anderson PA, Boden SD, Kim HJ, Vaccaro AR, Wang JC (2014) What’s new in spine surgery. J Bone Joint Surg Am 96(12):1048–1054. https://doi.org/10.2106/JBJS.N.00103
Brasil, Conselho Nacional de Secretários de Saúde (2007) Assistência de média e alta complexidade no SUS. https://bvsms.saude.gov.br/bvs/publicacoes/colec_progestores_livro9.pdf. Accessed 15 september 2020
Yoshihara H, Yoneoka D (2014) National trends in spinal fusion for pediatric patients with idiopathic scoliosis: demographics, blood transfusions, and in hospital outcomes. Spine 39(14):1144–1150. https://doi.org/10.1097/BRS.0000000000000354
Kim HJ, Cunningham ME, Boachie-Adjei O (2010) Revision spine surgery to manage pediatric deformity. J Am Acad Orthop Surg 18(12):739–748. https://doi.org/10.5435/00124635-201012000-00004
Sucato DJ (2010) Management of severe spinal deformity: scoliosis and kyphosis. Spine 35(25):2186–2192. https://doi.org/10.1097/BRS.0b013e3181feab19
Lykissas MG, Crawford AH, Jain VV (2013) Complications of surgical treatment of pediatric spinal deformities. Orthop Clin North Am 44(3):357–370. https://doi.org/10.1016/j.ocl.2013.03.007
Calman R, Smithers T, Rowan R (2013) Impact of surgical waiting time on paediatric spinal deformity patients. ANZ J Surg 83(12):929–932. https://doi.org/10.1111/ans.12196
Lima-Júnior PC, Pellegrino L, Caffaro MFS, Meves R, Landim E, Avanzi O (2011) Escoliose idiopática do adolescente (EIA): perfil clínico e radiográfico da lista de espera para tratamento cirúrgico em hospital terciário de alta complexidade do sistema público de saúde brasileiro. Coluna/Columna 10(2):111–115. https://doi.org/10.1590/S1808-18512011000200006
Oudhoff JP, Timmermans DR, Bijnen AB, van der Wal G (2004) Waiting for elective general surgery: physical, psychological and social consequences. ANZ J Surg 74(5):361–367. https://doi.org/10.1111/j.1445-1433.2004.02998.x
Tarrant RC, Queally JM, O’Loughlin PF, Sheeran P, Moore DP, Kiely PJ (2016) Preoperative curves of greater magnitude (>70°) in adolescent idiopathic scoliosis are associated with increased surgical complexity, higher cost of surgical treatment and a delayed return to function. Ir J Med Sci 185(2):463–471. https://doi.org/10.1007/s11845-015-1391-5
National Institute for Health Research. International prospective register of systematic reviews (PROSPERO). https://www.crd.york.ac.uk/prospero/ Accessed 11 November 2020
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ (2019) Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). www.training.cochrane.org/handbook/current. Accessed 06 september 2020
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C (2016) PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 75:40–46. https://doi.org/10.1016/j.jclinepi.2016.01.021
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
GRADEpro GDT https://www.gradepro.org Accessed 26 May 2022.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Ahn H, Kreder H, Mahomed N, Beaton D, Wright JG (2011) Empirically derived maximal acceptable wait time for surgery to treat adolescent idiopathic scoliosis. CMAJ 183(9):E565–E570. https://doi.org/10.1503/cmaj.101511
Fallatah S, Sait M, Almutairi F (2015) The effect of waiting for surgery on patients with adolescent idiopathic scoliosis. J Spine 4(2):1–4. https://doi.org/10.4172/2165-7939.1000224
Ramo B, Tran DP, Reddy A, Brown K, Niswander C, Erickson M, Garg S (2019) Delay to surgery greater than 6 months leads to substantial deformity progression and increased intervention in immature adolescent idiopathic scoliosis (AIS) patients: a retrospective cohort study. Spine Deform 7(3):428–435. https://doi.org/10.1016/j.jspd.2018.09.012
Tarrant R, Moore D, Kiely P (2016) Impact of longer surgical wait-list times on length of hospitalisation, return to function and cost of surgical treatment in patients with adolescent idiopathic scoliosis undergoing posterior spinal fusion. Global Spine J. https://doi.org/10.1055/s-0036-1583053
Lynch S, Devitt B, Conroy E, Moroney P, Taylor C, Noël J, Moore PK (2012) The cost implications of curve progression on scoliosis waiting list. Orthopaedic Proc British Editor Soc Bone Joint Surg 94(17):45
Parent S, Roy-Beaudry M, Coindet E, Joncas J, Mac-Thiong JM, Beauséjour M et al (2010) Should we worry about waiting times for idiopathic scoliosis surgery? Spine J Meet Abstr Paper 6:54
Miyanji F, Slobogean GP, Samdani AF, Betz RR, Reilly CW, Slobogean BL, Newton PO (2012) Is larger scoliosis curve magnitude associated with increased perioperative health-care resource utilization?: a multicenter analysis of 325 adolescent idiopathic scoliosis curves. J Bone Joint Surg Am 94(9):809–813. https://doi.org/10.2106/JBJS.J.01682
Yang JH, Bhandarkar AW, Rathanvelu B, Hwang JH, Hong JY, Modi HN, Suh SW (2014) Does delaying surgery in immature adolescent idiopathic scoliosis patients with progressive curve, lead to addition of fusion levels? Eur Spine J 23(12):2672–2679. https://doi.org/10.1007/s00586-014-3421-9
Kenner P, McGrath S, Woodland P (2019) What factors influence delayed referral to spinal surgeon in adolescent idiopathic scoliosis? Spine 44(22):1578–1584. https://doi.org/10.1097/BRS.0000000000003146
Bressan-Neto M, da Silva Herrero CFP, Pacola LM, Nunes AA, Defino HLA (2017) Community care administration of spinal deformities in the Brazilian public health system. Clinics 72(8):485–490. https://doi.org/10.6061/clinics/2017(08)06
Anthony A, Zeller R, Evans C, Dermott JA (2021) Adolescent idiopathic scoliosis detection and referral trends: impact treatment options. Spine Deform 9(1):75–84. https://doi.org/10.1007/s43390-020-00182-6
Lee JZ, Lam DJ, Lim KB (2014) Late presentation in adolescent idiopathic scoliosis: who, why, and how often? J Pediatr Orthop 23(1):6–14. https://doi.org/10.1097/01.bpb.0000434243.64440.13
Russell T, Dharia A, Folsom R, Kaki M, Shumbusho E, Fajardo RJ, Shah K, Shillingford-Cole V, Hogue GD (2020) Healthcare disparities in adolescent idiopathic scoliosis: the impact of socioeconomic factors on cobb angle. Spine Deform 8(4):605–611. https://doi.org/10.1007/s43390-020-00097-2
Funding
The project was funded by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), process 442639/2019–8. CNPq/MS/SCTIE/Decit number 27/2019–Research to strengthen the objectives and guidelines of the Care Network for People with Disabilities within the scope of the Unified Health System (SUS). Thematic line 3: Assessment of the health of people with Adolescent Idiopathic Scoliosis (AIS) and its repercussions for the Unified Health System.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A Detailing the search strategies
-
MEDLINE (via PubMed): 1164 studies
((wait* time) OR (wait* list) OR (delay* surgery) OR (late surgery)) AND ((scoliosis) OR (idiopathic scoliosis) OR (adolescent idiopathic scoliosis) OR (AIS)).
-
Embase: 62 studies
((wait* time) OR (wait* list) OR (delay* surgery)) AND (scoliosis).
-
LILACS: 8 studies
((waiting) OR (wait) OR (delay) OR (delaying)) AND (scoliosis).
-
SciELO: 6 studies
((wait*) OR (delay*)) AND (scoliosis).
-
Scopus: 258 studies
((wait*) OR (delay*)) AND (idiopathic scoliosis).
-
Web of Science: 5527 studies
((wait* time) OR (wait* list) OR (delay* surgery) OR (late surgery)) AND ((scoliosis) OR (idiopathic scoliosis) OR (adolescent idiopathic scoliosis) OR (AIS)).
-
LIVIVO: 265 studies
((wait*) OR (delay*)) AND (idiopathic scoliosis).
-
Cochrane Library: 606 studies
(adolescent idiopathic scoliosis).
-
Google Scholar: 2790 studies
((wait* time) OR (wait* list) OR (delay* surgery) OR (late surgery)) AND ((scoliosis) OR (idiopathic scoliosis) OR (adolescent idiopathic scoliosis) OR (AIS)).
-
ClinicalTrials.gov: 211 studies
(idiopathic scoliosis).
-
OpenGrey: 48 studies
(scoliosis).
Appendix B: Data extraction form
01) General information:
-
Title.
-
Authors.
-
Year of Publication.
-
Publication Format.
-
Country of Origin.
-
Study Design.
-
Place of Publication
02) Participants:
-
Age.
-
Sex.
03) Methodologies:
-
Goals.
-
Study Variables.
-
Randomization Techniques.
-
Intervention Techniques.
-
Control.
04) Results:
-
Number of Patients.
-
Measuring Tools.
-
Follow-up Time.
-
Waiting time for surgery.
-
Cobb angle at the time of registration in the waiting list.
-
Preoperative Cobb angle.
-
Change in surgical planning.
-
Quality of life assessment.
-
Cost assessment.
-
Statistical tests.
05) Other descriptors
06) Conclusions
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pontes, M.D.d., Soeira, T.P., Sampaio, M.L. et al. The impacts of waiting for surgical correction of Adolescent Idiopathic Scoliosis and its repercussions for publicly funded health systems: systematic review. Eur Spine J 32, 617–624 (2023). https://doi.org/10.1007/s00586-022-07487-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07487-2