Abstract
Purpose
To investigate the impact of lumbar fusion on spinopelvic sagittal alignment from standing to sitting position and the influencing factors of postoperative functional limitations due to lumbar stiffness.
Methods
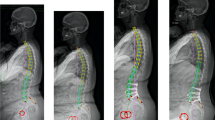
A total of 107 patients who undertook posterior lumbar interbody fusion were included. Patients were divided into two groups: Group A (lumbosacral fusion; n = 43) and Group B (floating fusion; n = 64). Spinopelvic parameters in standing and sitting position including pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), lumbar lordosis (LL), fusion segment lordosis (FSL), upper residual lordosis (URL), lower residual lordosis (LRL), thoracic kyphosis (TK), thoracolumbar kyphosis (TLK), sagittal vertical axis (SVA) and T1 pelvic angle (TPA) were measured before and after lumbar fusion. The Lumbar Stiffness Disability Index (LSDI) was used to assess functional limitations due to lumbar stiffness.
Results
Accompanied by increased postoperative LSDI, the values of changes from standing to sitting (∆) were reduced in some parameters compared with the preoperative values. ∆PT and ∆SS significantly decreased in both two groups. In Group A, ∆LL significantly decreased with increased ∆URL. In Group B, ∆LL, ∆URL and ∆LRL showed no significant difference before and after surgery. Multiple linear regression analysis showed that age and ∆PT independently influenced the postoperative LSDI in Group A.
Conclusion
After lumbar fusion, changes of lumbopelvic sagittal parameters from standing to sitting would be restricted. Adjacent segment lordosis could partially compensate for this restriction. For patients with lumbosacral fusion, postoperative functional limitations due to lumbar stiffness were related to age and the postoperative ∆PT from standing to sitting.



Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Al Jammal OM, Delavar A, Maguire KR, Hirshman BR, Wali AR, Kazzaz M, Pham MH (2019) National trends in the surgical management of lumbar spinal stenosis in adult spinal deformity patients. Spine (Phila Pa 1976) 44:369–378. https://doi.org/10.1097/BRS.0000000000003155
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1:2–18. https://doi.org/10.3978/j.issn.2414-469X.2015.10.05
Kimura H, Fujibayashi S, Otsuki B, Takahashi Y, Nakayama T, Matsuda S (2016) Effects of lumbar stiffness after lumbar fusion surgery on activities of daily living. Spine (Phila Pa 1976) 41:719–727. https://doi.org/10.1097/BRS.0000000000001300
Daniels AH, Smith JS, Hiratzka J, Ames CP, Bess S, Shaffrey CI, Schwab FJ, Lafage V, Klineberg EO, Burton D, Mundis GM, Line B, Hart RA (2015) International spine study g functional limitations due to lumbar stiffness in adults with and without spinal deformity. Spine 40:1599–1604. https://doi.org/10.1097/BRS.0000000000001090
Hart RA, Gundle KR, Pro SL, Marshall LM (2013) Lumbar stiffness disability index: pilot testing of consistency, reliability, and validity. Spine J 13:157–161. https://doi.org/10.1016/j.spinee.2012.12.001
Hart RA, Pro SL, Gundle KR, Marshall LM (2013) Lumbar stiffness as a collateral outcome of spinal arthrodesis: a preliminary clinical study. Spine J 13:150–156. https://doi.org/10.1016/j.spinee.2012.10.014
Durand WM, Daniels AH, Hamilton DK, Passias PG, Kim HJ, Protopsaltis T, Lafage V, Smith JS, Shaffrey C, Gupta M, Kelly MP, Klineberg E, Schwab F, Burton D, Bess S, Ames C, Hart R (2019) International spine study G younger patients are differentially affected by stiffness-related disability following adult spinal deformity surgery. World Neurosurg 132:e297–e304. https://doi.org/10.1016/j.wneu.2019.08.169
Tokida R, Uehara M, Ikegami S, Takahashi J, Nishimura H, Sakai N, Kato H (2019) association between sagittal spinal alignment and physical function in the Japanese general elderly population: a Japanese cohort survey randomly sampled from a basic resident registry. J Bone Joint Surg Am 101:1698–1706. https://doi.org/10.2106/JBJS.18.01384
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine(Phila Pa 1976) 37:1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2
Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38:E803-812. https://doi.org/10.1097/BRS.0b013e318292b7b9
Shin EK, Kim CH, Chung CK, Choi Y, Yim D, Jung W, Park SB, Moon JH, Heo W, Kim SM (2017) Sagittal imbalance in patients with lumbar spinal stenosis and outcomes after simple decompression surgery. Spine J 17:175–182. https://doi.org/10.1016/j.spinee.2016.08.023
Hey HWD, Teo AQA, Tan KA, Ng LWN, Lau LL, Liu KG, Wong HK (2017) How the spine differs in standing and in sitting-important considerations for correction of spinal deformity. Spine J 17:799–806. https://doi.org/10.1016/j.spinee.2016.03.056
Endo K, Suzuki H, Nishimura H, Tanaka H, Shishido T, Yamamoto K (2012) Sagittal lumbar and pelvic alignment in the standing and sitting positions. J Orthop Sci 17:682–686. https://doi.org/10.1007/s00776-012-0281-1
Wang S, Zhou Q, Xu L, Wang M, Qiu Y, Zhu Z, Wang B, Sun X (2021) Impact of lumbar fusion on sitting spinopelvic balance: multisegmental versus monosegmental. Clin Neurol Neurosurg 209:106905. https://doi.org/10.1016/j.clineuro.2021.106905
Hart RA, Marshall LM, Hiratzka SL, Kane MS, Volpi J, Hiratzka JR (2014) Functional limitations due to stiffness as a collateral impact of instrumented arthrodesis of the lumbar spine. Spine (Phila Pa 1976) 39:E1468-1474. https://doi.org/10.1097/BRS.0000000000000595
Sielatycki JA, Metcalf T, Koscielski M, Devin CJ, Hodges S (2021) Seated lateral X-ray is a better stress radiograph of the lumbar spine compared to standing flexion. Glob Spine J 11:1099–1103. https://doi.org/10.1177/2192568220939527
Lazennec JY, Clark IC, Folinais D, Tahar IN, Pour AE (2017) What is the impact of a spinal fusion on acetabular implant orientation in functional standing and sitting positions? J Arthroplast 32:3184–3190. https://doi.org/10.1016/j.arth.2017.04.051
Patwardhan AG, Sielatycki JA, Havey RM, Humphreys SC, Hodges SD, Blank KR, Muriuki MG (2021) Loading of the lumbar spine during transition from standing to sitting: effect of fusion versus motion preservation at L4–L5 and L5–S1. Spine J 21:708–719. https://doi.org/10.1016/j.spinee.2020.10.032
Sun Z, Zhou S, Wang W, Zou D, Li W (2020) Differences in standing and sitting spinopelvic sagittal alignment for patients with posterior lumbar fusion: important considerations for the changes of unfused adjacent segments lordosis. BMC Musculoskelet Disord 21:760. https://doi.org/10.1186/s12891-020-03777-2
Bagheri SR, Alimohammadi E, ZamaniFroushani A, Abdi A (2019) Adjacent segment disease after posterior lumbar instrumentation surgery for degenerative disease: incidence and risk factors. J Orthop Surg (Hong Kong). https://doi.org/10.1177/2309499019842378
Haffer H, AdlAmini D, Perka C, Pumberger M (2020) The impact of spinopelvic mobility on arthroplasty: implications for hip and spine surgeons. J Clin Med. https://doi.org/10.3390/jcm9082569
Stefl M, Lundergan W, Heckmann N, McKnight B, Ike H, Murgai R, Dorr LD (2017) Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J 99-b:37–45. https://doi.org/10.1302/0301-620x.99b1.Bjj-2016-0415.R1
Funding
This article is supported by the National Natural Science Foundation of China (Grant No. 81871807).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethics approval
This study was approved by the institutional review board of the hospital. For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, S., Qiu, W., Wang, W. et al. Impact of lumbar fusion on spinopelvic sagittal alignment from standing to sitting position: which factor is associated with postoperative functional limitations due to lumbar stiffness?. Eur Spine J 32, 345–352 (2023). https://doi.org/10.1007/s00586-022-07438-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07438-x