Abstract
Purpose
The current investigation aimed to compare the sensorimotor integration, sensorimotor control, and cost of cognitive-motor dual task during walking, in persons with chronic WAD as compared to matched chronic idiopathic neck pain and normal healthy controls.
Methods
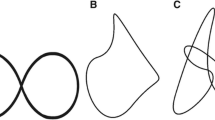
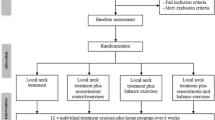
A cross-sectional, case control design comparing 30 participants in each of two study groups (chronic WAD and chronic idiopathic neck pain) to a matched control group was conducted. Measurements included: (1) the cranio-vertebral angle (CVA), (2) left and right rotation head repositioning accuracy (HRA), (3) frontal N30 amplitudes to assess sensorimotor integration, (4) dual cognitive gait cost (DCGC).
Results
A statistically significant difference for the CVA was found between groups: WAD 36.8° ± 3.4, chronic pain 44.5° ± 1.5, and controls 47.1° ± 4; p < 0.05. MANOVA revealed significant group differences for the N30 amplitude (p < 0.05), where the WAD group had the greatest amplitude. Statistically significant differences among the three groups were found for HRA left and right where the WAD group had the greatest error, (p < 0.05). Post hoc tests revealed that the WAD group had the highest dual-task cost during walking, (p < 0.05). Significant linear correlations between the CVA and N30 amplitude, HRA, and DCGC were identified in all 3 groups, (p < 0.05).
Conclusions
Compared to both a matched control group and chronic neck pain group, whiplash-injured persons have greater forward head posture, greater error in sensorimotor control, and an altered ability to perform a motor task with a simultaneous cognitive task.


Similar content being viewed by others
Data availability
All data analyzed during the current study are available at https://figshare.com/account/home. https://doi.org/10.6084/m9.figshare.19999994.
References
Cecchi F, Molino-Lova R, Paperini A et al (2011) Predictors of short- and long-term outcome in patients with chronic non-specific neck pain undergoing an exercise-based rehabilitation program: a prospective cohort study with 1 year follow-up. Intern Emerg Med 6:413–421. https://doi.org/10.1007/s11739-010-0499-x
Kazeminasab S, Nejadghaderi SA, Amiri P et al (2022) Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. https://doi.org/10.1186/S12891-021-04957-4
Ris I, Juul-Kristensen B, Boyle E et al (2017) Chronic neck pain patients with traumatic or non-traumatic onset: differences in characteristics. A cross-sectional study Scand J Pain 14:1–8. https://doi.org/10.1016/J.SJPAIN.2016.08.008/XML
Rodriquez AA, Barr KP, Burns SP (2004) Whiplash: pathophysiology, diagnosis, treatment, and prognosis. Muscle Nerve 29:768–781. https://doi.org/10.1002/MUS.20060
Sturzenegger M, Radanov BP, Winter P et al (2008) MRI-based brain volumetry in chronic whiplash patients: no evidence for traumatic brain injury. Acta Neurol Scand 117:49–54. https://doi.org/10.1111/J.1600-0404.2007.00939.X
Dancey E, Murphy B, Srbely J, Yielder P (2014) The effect of experimental pain on motor training performance and sensorimotor integration. Exp Brain Res 232:2879–2889. https://doi.org/10.1007/S00221-014-3966-1
Moustafa IM, Diab AA, Hegazy F (2021) Harrison DE (2021) Demonstration of central conduction time and neuroplastic changes after cervical lordosis rehabilitation in asymptomatic subjects: a randomized, placebo-controlled trial. Sci Rep 111(11):1–13. https://doi.org/10.1038/s41598-021-94548-z
Machado D, Bastos VH, Cunha M et al (2009) Efectos del bromacepam en el desarrollo de una actividad sensoriomotora: un estudio electroencefalográfico. Rev Neurol 49:295–299. https://doi.org/10.33588/rn.4906.2008471
Krakauer JW, Mazzoni P, Ghazizadeh A et al (2006) Generalization of motor learning depends on the history of prior action. PLoS Biol 4:e316. https://doi.org/10.1371/journal.pbio.0040316
Grosso MJ, Hwang R, Mroz T et al (2013) Relationship between degree of focal kyphosis correction and neurological outcomes for patients undergoing cervical deformity correction surgery. J Neurosurg Spine 18:537–544
Sterling M (2014) Physiotherapy management of whiplash-associated disorders (WAD). J Physiother 60:5–12. https://doi.org/10.1016/j.jphys.2013.12.004
Kessels RPC, Aleman A, Verhagen WIM, Van Luijtelaar ELJM (2000) Cognitive functioning after whiplash injury: a meta-analysis. J Int Neuropsychol Soc 6:271–278. https://doi.org/10.1017/S1355617700633027
Strober LB, Becker A, Randolph JJ (2018) Role of positive lifestyle activities on mood, cognition, well-being, and disease characteristics in multiple sclerosis. Appl Neuropsychol Adult 25:304–311. https://doi.org/10.1080/23279095.2018.1458518
Gurumoorthy D, Twomey L, Cassidy JD, Skovron ML (1996) The Quebec task force on whiplash-associated disorders. Spine (Phila Pa 1976) 21:897–898. https://doi.org/10.1097/00007632-199604010-00027
Van Niekerk SM, Louw Q, Vaughan C et al (2008) Photographic measurement of upper-body sitting posture of high school students: a reliability and validity study. BMC Musculoskelet Disord 9:113. https://doi.org/10.1186/1471-2474-9-113
Moustafa IM, Diab AA, Hegazy F, Harrison DE (2021) Demonstration of central conduction time and neuroplastic changes after cervical lordosis rehabilitation in asymptomatic subjects: a randomized, placebo-controlled trial. Sci Rep. https://doi.org/10.1038/S41598-021-94548-Z
Andrew D, Haavik H, Dancey E, Yielder P, Murphy B (2015) Somatosensory evoked potentials show plastic changes following a novel motor training task with the thumb. Clin Neurophysiol 126:575–580
Kanovský P, Bares M, Rektor I (2003) The selective gating of the N30 cortical component of the somatosensory evoked potentials of median nerve is different in the mesial and dorsolateral frontal cortex: evidence from intracerebral recordings. Clin Neurophysiol 114:981–991
Grip H, Sundelin G, Gerdle B, Karlsson JS (2007) Variations in the axis of motion during head repositioning: a comparison of subjects with whiplash-associated disorders or non-specific neck pain and healthy controls. Clin Biomech (Bristol, Avon) 22:865–873. https://doi.org/10.1016/J.CLINBIOMECH.2007.05.008
Leone C, Patti F, Feys P (2015) Measuring the cost of cognitive-motor dual tasking during walking in multiple sclerosis. Mult Scler 21:123–131. https://doi.org/10.1177/1352458514547408
Pleger B, Ragert P, Schwenkreis P et al (2006) Patterns of cortical reorganization parallel impaired tactile discrimination and pain intensity in complex regional pain syndrome. Neuroimage 32:503–510. https://doi.org/10.1016/J.NEUROIMAGE.2006.03.045
Waberski TD, Buchner H, Perkuhn M et al (1999) N30 and the effect of explorative finger movements: a model of the contribution of the motor cortex to early somatosensory potentials. Clin Neurophysiol 110:1589–1600. https://doi.org/10.1016/S1388-2457(99)00092-9
Rossi S, Della Volpe R, Ginanneschi F et al (2003) Early somatosensory processing during tonic muscle pain in humans: relation to loss of proprioception and motor “defensive” strategies. Clin Neurophysiol 114:1351–1358. https://doi.org/10.1016/S1388-2457(03)00073-7
Chien A, Sterling M (2010) Sensory hypoaesthesia is a feature of chronic whiplash but not chronic idiopathic neck pain. Man Ther 15:48–53. https://doi.org/10.1016/J.MATH.2009.05.012
Costigan M, Scholz J, Woolf CJ (2009) Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci 32:1. https://doi.org/10.1146/ANNUREV.NEURO.051508.135531
Daligadu J, Haavik H, Yielder PC et al (2013) Alterations in cortical and cerebellar motor processing in subclinical neck pain patients following spinal manipulation. J Manipulative Physiol Ther 36:527–537. https://doi.org/10.1016/j.jmpt.2013.08.003
Moustafa IM, Youssef A, Ahbouch A et al (2020) Is forward head posture relevant to autonomic nervous system function and cervical sensorimotor control? Cross Sect Study Gait Posture. https://doi.org/10.1016/j.gaitpost.2020.01.004
Moustafa IM, Diab AA, Harrison DE (2017) The effect of normalizing the sagittal cervical configuration on dizziness, neck pain, and cervicocephalic kinesthetic sensibility: a 1 year randomized controlled study. Eur J Phys Rehabil Med 53:57–71. https://doi.org/10.23736/S1973-9087.16.04179-4
Moustafa I, Youssef ASA, Ahbouch A, Harrison D (2021) Demonstration of autonomic nervous function and cervical sensorimotor control after cervical lordosis rehabilitation: a randomized controlled trial. J Athl Train. https://doi.org/10.4085/1062-6050-0481.19
Hishinuma M, Yamaguchi T (1990) Axonal projection of descending pathways responsible for eliciting forelimb stepping into the cat cervical spinal cord. Exp Brain Res 82:597–605. https://doi.org/10.1007/BF00228801
Killane I, Donoghue OA, Savva GM et al (2014) Relative association of processing speed, short-term memory and sustained attention with task on gait speed: a study of community-dwelling people 50 years and older. J Gerontol A Biol Sci Med Sci 69:1407–1414. https://doi.org/10.1093/GERONA/GLU140
Buneo CA, Andersen RA (2006) The posterior parietal cortex: sensorimotor interface for the planning and online control of visually guided movements. Neuropsychologia 44:2594–2606. https://doi.org/10.1016/J.NEUROPSYCHOLOGIA.2005.10.011
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest. All authors declare no other relationships or activities that could appear to have influenced the submitted work.
Ethical standard
The trial was approved by the local ethics committee of the Cairo University, Egypt ((CA-REC-22–3-21).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moustafa, I.M., Diab, A., Shousha, T. et al. Sensorimotor integration, cervical sensorimotor control, and cost of cognitive-motor dual tasking: Are there differences in patients with chronic whiplash-associated disorders and chronic idiopathic neck pain compared to healthy controls?. Eur Spine J 31, 3452–3461 (2022). https://doi.org/10.1007/s00586-022-07390-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07390-w