Abstract
Purpose
To assess the responsiveness of the Zurich Claudication Questionnaire (ZCQ), the Oswestry Disability Index, the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire, the visual analog scale (VAS), the 8-Item Short Form Health Survey (SF-8), and the EuroQol 5 dimensions 5 level as methods of assessing outcomes of surgery for lumbar spinal stenosis.
Methods
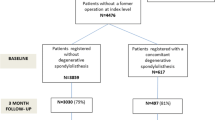
We analyzed 218 patients who had undergone lumbar surgery for spinal stenosis and completed one year of follow-up. The internal responsiveness of each questionnaire and any domains was assessed by the effect size and standardized response mean. External responsiveness was assessed by the Spearman rank correlation coefficient and the receiver operating characteristics (ROC) curve.
Results
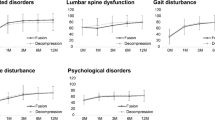
The most responsive assessments were “symptom severity” and “physical function” on the ZCQ, “walking ability” on the JOABPEQ, “leg pain” on the VAS, and “social function” on the JOABPEQ. The moderately responsive assessments were the physical component summary on the SF-8, the ODI, the EQ5D-5L, “low back pain” on the JOABPEQ, and “leg numbness” on the VAS. The least responsive assessments were “low back pain” on the VAS, “mental health” and “lumbar function” on the JOABPEQ, and the mental component summary on the SF-8.
Conclusions
Because of its high responsiveness, “symptom severity” on the ZCQ is recommended as a primary tool for assessing outcome when designing prospective studies for lumbar spinal stenosis.






Similar content being viewed by others
References
Forsth P, Olafsson G, Carlsson T, Frost A, Borgstrom F, Fritzell P, Ohagen P, Michaelsson K, Sanden B (2016) A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 374:1413–1423. https://doi.org/10.1056/NEJMoa1513721
Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VK, Barker FG 2nd, Benzel EC (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374:1424–1434. https://doi.org/10.1056/NEJMoa1508788
Cleland JA, Whitman JM, Houser JL, Wainner RS, Childs JD (2012) Psychometric properties of selected tests in patients with lumbar spinal stenosis. Spine J 12:921–931. https://doi.org/10.1016/j.spinee.2012.05.004
US Department of Health Human Services FDA Center for Drug Evaluation Research, US Department of Health Human Services FDA Center for Biologics Evaluation Research, US Department of Health Human Services FDA Center for Devices Radiological Health (2006) Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes 4:79. https://doi.org/10.1186/1477-7525-4-79
Fujimori T, Miwa T, Iwasaki M, Oda T (2018) Cost-effectiveness of lumbar fenestration surgery in the Japanese universal health insurance system. J Orthop Sci 23:889–894. https://doi.org/10.1016/j.jos.2018.06.020
Fujimori T, Miwa T, Iwasaki M, Oda T (2018) Cost-effectiveness of posterior lumbar interbody fusion in the Japanese universal health insurance system. J Orthop Sci 23:299–303. https://doi.org/10.1016/j.jos.2017.11.014
Jenis L (2012) Lumbar spinal stenosis and degenerative spondylolisthesis. In: Rao R (ed) orthopedic knowledge update - Spine American academy of Orthopaedic Surgeons, Chicago, IL. pp 329–335
Kreiner DS (2011) North American spine society clinical guidelines for multidisciplinary spine care diagnosis and treatment of degenerative lumbar spinal stenosis. North American Spine Society, Burr Ridge
Stucki G, Daltroy L, Liang MH, Lipson SJ, Fossel AH, Katz JN (1996) Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine(Phila Pa 1976) 21:796–803. https://doi.org/10.1097/00007632-199604010-00004
Fairbank JC (2000) The use of revised oswestry disability questionnaire. Spine (Phila Pa 1976) 25:2846–2847
Fukui M, Chiba K, Kawakami M, Kikuchi S, Konno S, Miyamoto M, Seichi A, Shimamura T, Shirado O, Taguchi T, Takahashi K, Takeshita K, Tani T, Toyama Y, Yonenobu K, Wada E, Tanaka T, Hirota Y (2009) JOA Back pain evaluation questionnaire (joabpeq)/joa cervical myelopathy evaluation questionnaire (joacmeq). the report on the development of revised versions. april 16, 2007. the subcommittee of the clinical outcome committee of the Japanese orthopaedic association on low back pain and cervical myelopathy evaluation. J Orthop Sci 14:348–365. https://doi.org/10.1007/s00776-009-1337-8
Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K (1998) Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol 51:1037–1044
Shiroiwa T, Ikeda S, Noto S, Igarashi A, Fukuda T, Saito S, Shimozuma K (2016) Comparison of value set based on DCE and/or TTO data: scoring for EQ-5D-5L health states in Japan. Value in Health 19:648–654. https://doi.org/10.1016/j.jval.2016.03.1834
Thiese MS, Hegmann KT, Wood EM, Garg A, Moore JS, Kapellusch J, Foster J, Ott U (2014) Prevalence of low back pain by anatomic location and intensity in an occupational population. BMC Musculoskelet Disord 15:283. https://doi.org/10.1186/1471-2474-15-283
Deyo RA, Mirza SK (2016) Clinical practice. herniated lumbar intervertebral disk. N Engl J Med 374:1763–1772. https://doi.org/10.1056/NEJMcp1512658
Griffin LY (ed) (2005) Essentials of musculoskeletal care. American Academy of Orthopaedic Surgeons, Rosemont, IL
Hara N, Matsudaira K, Masuda K, Tohnosu J, Takeshita K, Kobayashi A, Murakami M, Kawamura N, Yamakawa K, Terayama S, Ogihara S, Shiono H, Morii J, Hayakawa K, Kato S, Nakamura K, Oka H, Sawada T, Inuzuka K, Kikuchi N (2016) Psychometric assessment of the Japanese version of the Zurich claudication questionnaire (ZCQ): reliability and validity. PLoS ONE 11:e0160183. https://doi.org/10.1371/journal.pone.0160183
Hashimoto H, Komagata M, Nakai O, Morishita M, Tokuhashi Y, Sano S, Nohara Y, Okajima Y (2006) Discriminative validity and responsiveness of the Oswestry disability Index among Japanese outpatients with lumbar conditions. Eur Spine J 15:1645–1650. https://doi.org/10.1007/s00586-005-0022-7
Fukui M, Chiba K, Kawakami M, Kikuchi S, Konno S, Miyamoto M, Seichi A, Shimamura T, Shirado O, Taguchi T, Takahashi K, Takeshita K, Tani T, Toyama Y, Yonenobu K, Wada E, Tanaka T, Hirota Y (2007) Japanese orthopaedic association back pain evaluation Questionnaire. Part 2. Verification of its reliability: the subcommittee on low back pain and cervical myelopathy evaluation of the clinical outcome committee of the Japanese orthopaedic association. J Orthop Sci 12:526–532. https://doi.org/10.1007/s00776-007-1168-4
Guyatt G, Walter S, Norman G (1987) Measuring change over time: assessing the usefulness of evaluative instruments. J Chronic Dis 40:171–178
Husted JA, Cook RJ, Farewell VT, Gladman DD (2000) Methods for assessing responsiveness: a critical review and recommendations. J Clin Epidemiol 53:459–468
Guyatt GH, Deyo RA, Charlson M, Levine MN, Mitchell A (1989) Responsiveness and validity in health status measurement: a clarification. J Clin Epidemiol 42:403–408
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC (2007) Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 60:34–42. https://doi.org/10.1016/j.jclinepi.2006.03.012
Fujimori T, Miwa T, Oda T (2019) Responsiveness of the Japanese orthopaedic association back pain evaluation questionnaire in lumbar surgery and its threshold for indicating clinically important differences. Spine J 19:95–103. https://doi.org/10.1016/j.spinee.2018.05.013
Lang CE, Edwards DF, Birkenmeier RL, Dromerick AW (2008) Estimating minimal clinically important differences of upper-extremity measures early after stroke. Arch Phys Med Rehabil 89:1693–1700. https://doi.org/10.1016/j.apmr.2008.02.022
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36. https://doi.org/10.1148/radiology.143.1.7063747
Cohen J (1988) Statistical power analysis for the behavioral-sciences - cohen. J Percept Motor Skill 67:1007–1007
Lakens D (2013) Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol 4:863. https://doi.org/10.3389/fpsyg.2013.00863
Schober P, Boer C, Schwarte LA (2018) Correlation coefficients: appropriate use and interpretation. Anesth Analg 126:1763–1768. https://doi.org/10.1213/ANE.0000000000002864
Fairbank JC (2014) Why are there different versions of the Oswestry disability index? J Neurosurg Spine 20:83–86. https://doi.org/10.3171/2013.9.SPINE13344
Pratt RK, Fairbank JC, Virr, (2002) The reliability of the shuttle walking test, the Swiss spinal stenosis questionnaire, the Oxford spinal stenosis score, and the Oswestry disability index in the assessment of patients with lumbar spinal stenosis. Spine(Phila Pa 1976) 27:84–91. https://doi.org/10.1097/00007632-200201010-00020
Tonosu J, Takeshita K, Hara N, Matsudaira K, Kato S, Masuda K, Chikuda H (2012) The normative score and the cut-off value of the Oswestry Disability Index (ODI). Eur Spine J 21:1596–1602. https://doi.org/10.1007/s00586-012-2173-7
Fukushima M, Oka H, Oshima Y, Yuzawa Y, Matsudaira K, Tanaka S, Inanami H (2020) Evaluation of the minimum clinically important differences of the Zurich claudication questionnaire in patients with lumbar spinal stenosis. Clin Spine Surg 33:E499–E503. https://doi.org/10.1097/BSD.0000000000000983
Walsh TL, Hanscom B, Lurie JD, Weinstein JN (2003) Is a condition-specific instrument for patients with low back pain/leg symptoms really necessary? The responsiveness of the Oswestry Disability Index, MODEMS, and the SF-36. Spine (Phila Pa 1976) 28:607–615. https://doi.org/10.1097/01.BRS.0000050654.97387.DF
Streiner DL, Norman GR, Cairney J (2015) Health measurement scales: a practical guide to their development and use. Oxford University Press, Oxford
Norman G (2003) Hi! How are you? Response shift, implicit theories and differing epistemologies. Qual Life Res 12:239–249. https://doi.org/10.1023/a:1023211129926
Fujimori T, Okuda S, Iwasaki M, Yamasaki R, Maeno T, Yamashita T, Matsumoto T, Wada E, Oda T (2016) Validity of the Japanese Orthopaedic Association scoring system based on patient-reported improvement after posterior lumbar interbody fusion. Spine J 16:728–736. https://doi.org/10.1016/j.spinee.2016.01.181
Schwartz CE, Sprangers MA (1999) Methodological approaches for assessing response shift in longitudinal health-related quality-of-life research. Soc Sci Med 48:1531–1548. https://doi.org/10.1016/s0277-9536(99)00047-7
Kunze KN, Fontana MA, MacLean CH, Lyman S, McLawhorn AS (2021) Defining the patient acceptable symptom state for the HOOS JR and KOOS JR after primary total joint arthroplasty. J Bone Joint Surg Am. https://doi.org/10.2106/JBJS.21.00550
Fujimori T, Iwasaki M, Okuda S, Nagamoto Y, Sakaura H, Oda T, Yoshikawa H (2011) Patient satisfaction with surgery for cervical myelopathy due to ossification of the posterior longitudinal ligament. J Neurosurg Spine 14:726–733. https://doi.org/10.3171/2011.1.SPINE10649
Hattie JAC (2009) Visible learning a synthesis of over 800 meta-analyses relating to achievement. Visible learning a synthesis of over 800 meta-analyses relating to achievement. Routledge, Oxford
Funding
This work was supported by JSPS KAKENHI Grant Number JP21K20966.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest associated with this manuscript.
Ethics approval
This study was approved by the institutional review board of Japan Community Healthcare Organization, Osaka Hospital (IRB 2018–52).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fujimori, T., Ikegami, D., Sugiura, T. et al. Responsiveness of the Zurich Claudication Questionnaire, the Oswestry Disability Index, the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire, the 8-Item Short Form Health Survey, and the Euroqol 5 dimensions 5 level in the assessment of patients with lumbar spinal stenosis. Eur Spine J 31, 1399–1412 (2022). https://doi.org/10.1007/s00586-022-07236-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07236-5