Abstract
Purpose
Our study aimed to evaluate non-inferiority of ProDisc-C to anterior cervical discectomy and fusion (ACDF) in terms of clinical outcomes and incidence of adjacent segment disease (ASD) at 24-months post-surgery in Asian patients with symptomatic cervical disc disease (SCDD).
Methods
This multicentre, prospective, randomized controlled trial was initiated after ethics committee approval at nine centres (China/Hong Kong/Korea/Singapore/Taiwan). Patients with single-level SCDD involving C3-C7-vertebral segments were randomized (2:1) into: group-A treated with ProDisc–C and group-B with ACDF. Assessments were conducted at baseline, 6-weeks, 3/6/12/18/24-months post-surgery and annually thereafter till 84-months. Primary endpoint was overall success at 24-months, defined as composite of: (1) ≥ 20% improvement in neck disability index (NDI); (2) maintained/improved neurologic parameters; (3) no implant removal/revision/re-operation at index level; and (4) no adverse/severe/life-threatening events.
Results
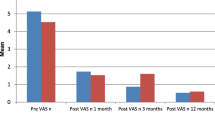
Of 120 patients (80ProDisc–C,40ACDF), 76 and 37 were treated as per protocol (PP). Overall success (PP) was 76.5% in group-A and 81.8% in group-B at 24-months (p = 0.12), indicating no clear non-inferiority of ProDisc-C to ACDF. Secondary outcomes improved for both groups with no significant inter-group differences. Occurrence of ASD was higher in group-B with no significant between-group differences. Range of motion (ROM) was sustained with ProDisc–C but lost with ACDF at 24-months.
Conclusion
Cervical TDR with ProDisc–C is feasible, safe, and effective for treatment of SCDD in Asians. No clear non-inferiority was demonstrated between ProDisc-C and ACDF. However, patients treated with ProDisc–C demonstrated significant improvement in NDI, neurologic success, pain scores, and 36-item-short-form survey, along with ROM preservation at 24-months. Enrolment difficulties resulted in inability to achieve pre-planned sample size to prove non-inferiority. Future Asian-focused, large-scale studies are needed to establish unbiased efficacy of ProDisc-C to ACDF.




Similar content being viewed by others
References
Zigler JE, Delamarter R, Murrey D, Spivak J, Janssen M (2013) ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. Spine (Phila Pa 1976) 38 (3):203–209. https://doi.org/10.1097/BRS.0b013e318278eb38
Hilibrand AS, Yoo JU, Carlson GD, Bohlman HH (1997) The success of anterior cervical arthrodesis adjacent to a previous fusion. Spine (Phila Pa 1976) 22 (14):1574–1579
Chung JY, Park JB, Seo HY, Kim SK (2016) adjacent segment pathology after anterior cervical fusion. Asian Spine J 10(3):582–592. https://doi.org/10.4184/asj.2016.10.3.582
Jaramillo-de la Torre JJ, Grauer JN, Yue JJ (2008) Update on cervical disc arthroplasty: where are we and where are we going? Curr Rev Musculoskelet Med 1(2):124–130. https://doi.org/10.1007/s12178-008-9019-2
Zhu Y, Zhang B, Liu H, Wu Y, Zhu Q (2016) Cervical disc arthroplasty versus anterior cervical discectomy and fusion for incidence of symptomatic adjacent segment disease: a meta-analysis of prospective randomized controlled trials. Spine (Phila Pa 1976) 41 (19):1493–1502. https://doi.org/10.1097/BRS.0000000000001537
Hu Y, Lv G, Ren S, Johansen D (2016) Mid-to long-term outcomes of cervical disc arthroplasty versus anterior cervical discectomy and fusion for treatment of symptomatic cervical disc disease: a systematic review and meta-analysis of eight prospective randomized controlled trials. PloS One 11 (2):e0149312
Luo J, Wang H, Peng J, Deng Z, Zhang Z, Liu S, Wang D, Gong M, Tang S (2018) Rate of adjacent segment degeneration of cervical disc arthroplasty versus fusion meta-analysis of randomized controlled trials. World Neurosurg 113:225–231. https://doi.org/10.1016/j.wneu.2018.02.113
Zhang Y, Lv N, He F, Pi B, Liu H, Chen AC, Yang H, Liu M, Zhu X (2020) Comparison of cervical disc arthroplasty and anterior cervical discectomy and fusion for the treatment of cervical disc degenerative diseases on the basis of more than 60 months of follow-up: a systematic review and meta-analysis. BMC Neurol 20(1):143. https://doi.org/10.1186/s12883-020-01717-0
Badhiwala JH, Platt A, Witiw CD, Traynelis VC (2020) Cervical disc arthroplasty versus anterior cervical discectomy and fusion: a meta-analysis of rates of adjacent-level surgery to 7-year follow-up. J Spine Surg 6(1):217–232. https://doi.org/10.21037/jss.2019.12.09
Murrey D, Janssen M, Delamarter R, Goldstein J, Zigler J, Tay B, Darden B (2009) Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J 9(4):275–286. https://doi.org/10.1016/j.spinee.2008.05.006
Delamarter RB, Zigler J (2013) Five-year reoperation rates, cervical total disc replacement versus fusion, results of a prospective randomized clinical trial. Spine (Phila Pa 1976) 38 (9):711–717. https://doi.org/10.1097/BRS.0b013e3182797592
Loumeau TP, Darden BV, Kesman TJ, Odum SM, Van Doren BA, Laxer EB, Murrey DB (2016) A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease (SCDD) following ProDisc-C total disc arthroplasty (TDA) versus anterior cervical discectomy and fusion (ACDF). Eur Spine J 25(7):2263–2270. https://doi.org/10.1007/s00586-016-4431-6
Janssen ME, Zigler JE, Spivak JM, Delamarter RB, Darden BV, 2nd, Kopjar B (2015) ProDisc-C total disc replacement versus anterior cervical discectomy and fusion for single-level symptomatic cervical disc disease: seven-year follow-up of the prospective randomized u.s. food and drug administration investigational device exemption study. J Bone Joint Surg Am 97 (21):1738–1747. https://doi.org/10.2106/JBJS.N.01186
Kapadia BH, Decker SI, Boylan MR, Shah NV, Paulino CB (2019) Risk factors for cerebrospinal fluid leak following anterior cervical discectomy and fusion. Clin Spine Surg 32(2):E86-e90. https://doi.org/10.1097/bsd.0000000000000732
Elsamadicy AA, Koo AB, Lee M, David WB, Kundishora AJ, Robert SM, Kuzmik GA, Coutinho PO, Kolb L, Laurans M, Abbed K (2020) Associated risk factors for extended length of stay following anterior cervical discectomy and fusion for cervical spondylotic myelopathy. Clin Neurol Neurosurg 195:105883. https://doi.org/10.1016/j.clineuro.2020.105883
Poorman GW, Moon JY, Horn SR, Jalai C, Zhou PL, Bono O, Passias PG (2018) Rates of mortality in cervical spine surgical procedures and factors associated with its occurrence over a 10-year period: a study of 342 477 patients on the nationwide inpatient sample. Int J Spine Surg 12(2):276–284. https://doi.org/10.14444/5034
Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA (2007) Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine 6(3):198–209. https://doi.org/10.3171/spi.2007.6.3.198
Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, Coric D, Cauthen JC, Riew DK (2009) Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 34 (2):101–107. https://doi.org/10.1097/BRS.0b013e31818ee263
Vaccaro A, Beutler W, Peppelman W, Marzluff JM, Highsmith J, Mugglin A, DeMuth G, Gudipally M, Baker KJ (2013) Clinical outcomes with selectively constrained SECURE-C cervical disc arthroplasty: two-year results from a prospective, randomized, controlled, multicenter investigational device exemption study. Spine (Phila Pa 1976) 38 (26):2227–2239. https://doi.org/10.1097/BRS.0000000000000031
Phillips FM, Lee JY, Geisler FH, Cappuccino A, Chaput CD, DeVine JG, Reah C, Gilder KM, Howell KM, McAfee PC (2013) A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. 2-year results from the US FDA IDE clinical trial. Spine (Phila Pa 1976) 38 (15):E907–918. https://doi.org/10.1097/BRS.0b013e318296232f
Galbraith JG, Butler JS, Dolan AM, O’Byrne JM (2012) Operative outcomes for cervical myelopathy and radiculopathy. Adv Orthop 2012:919153. https://doi.org/10.1155/2012/919153
Bertalanffy H, Eggert HR (1988) Clinical long-term results of anterior discectomy without fusion for treatment of cervical radiculopathy and myelopathy. A follow-up of 164 cases. Acta Neurochir (Wien) 90 (3–4):127–135. https://doi.org/10.1007/bf01560567
Skeppholm M, Henriques T, Tullberg T (2017) Higher reoperation rate following cervical disc replacement in a retrospective, long-term comparative study of 715 patients. Eur Spine J 26(9):2434–2440. https://doi.org/10.1007/s00586-017-5218-0
Blumenthal SL, Ohnmeiss DD, Guyer RD, Zigler JE (2013) Reoperations in cervical total disc replacement compared with anterior cervical fusion: results compiled from multiple prospective food and drug administration investigational device exemption trials conducted at a single site. Spine (Phila Pa 1976) 38 (14):1177–1182. https://doi.org/10.1097/BRS.0b013e31828ce774
Rozankovic M, Marasanov SM, Vukic M (2016) Cervical disc replacement with discover versus fusion in a single level cervical disc disease: a prospective single center randomized trial with a minimum two-year follow-up. Clin Spine Surg. https://doi.org/10.1097/BSD.0000000000000170
Skeppholm M, Lindgren L, Henriques T, Vavruch L, Lofgren H, Olerud C (2015) The Discover artificial disc replacement versus fusion in cervical radiculopathy–a randomized controlled outcome trial with 2-year follow-up. Spine J 15(6):1284–1294. https://doi.org/10.1016/j.spinee.2015.02.039
Nunley PD, Kerr EJ 3rd, Cavanaugh DA, Utter PA, Campbell PG, Wadhwa R, Frank KA, Marshall KE, Stone MB (2020) adjacent segment pathology after treatment with cervical disc arthroplasty or anterior cervical discectomy and fusion, part 2: clinical results at 7-year follow-Up. Int J Spine Surg 14(3):278–285. https://doi.org/10.14444/7037
Nunley PD, Kerr EJ 3rd, Cavanaugh DA, Utter PA, Campbell PG, Wadhwa R, Frank KA, Marshall KE, Stone MB (2020) Adjacent segment pathology after treatment with cervical disc arthroplasty or anterior cervical discectomy and fusion, part 1: radiographic results at 7-year follow-up. Int J Spine Surg 14(3):269–277. https://doi.org/10.14444/7036
Acknowledgements
We would like to acknowledge the administrative support provided by Keith Gerard Lopez, Sridharan Alathur Ramakrishnan, and Dr Nandika Naresh for the development of the manuscript.
Funding
The study was sponsored by DePuy Synthes. The sponsor had no role in the conduction of the study or the compilation of the study report/manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Ethics approval
The study was conducted after receiving approval from the Institutional Review Board or Ethics Committee at each of the nine study centres.
Consent to participate
A signed informed consent form was obtained from the patients prior to participation in the study.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These affiliations are during the active phase of the study, and hence represent the study centres at which the study was conducted.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kumar, N., Liu, Z.J., Poon, W.S. et al. ProDisc–C versus anterior cervical discectomy and fusion for the surgical treatment of symptomatic cervical disc disease: two-year outcomes of Asian prospective randomized controlled multicentre study. Eur Spine J 31, 1260–1272 (2022). https://doi.org/10.1007/s00586-021-07055-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-07055-0