Abstract
Objective
To identify the impact of osteoporosis (OS) on postoperative outcomes in Medicare patients undergoing ASD surgery.
Background
Patients with OP and advanced age experience higher than average rates of ASD. However, poor bone density could undermine the durability of a deformity correction.
Methods
We queried the MarketScan Medicare Supplemental database to identify patients Medicare patients who underwent ASD surgery from 2007 to 2016.
Results
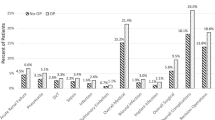
A total of 2564 patients met the inclusion criteria of this study, of whom n = 971 (61.0%) were diagnosed with osteoporosis. Patients with OP had a similar 90-day postoperative complication rates (OP: 54.6% vs. non-OP: 49.2%, p = 0.0076, not significant after multivariate regression correction). This was primarily driven by posthemorrhagic anemia (37.6% in OP, vs. 33.1% in non-OP). Rates of revision surgery were similar at 90 days (non-OP 15.0%, OP 16.8%), but by 2 years, OP patients had a significantly higher reoperation rate (30.4% vs. 22.9%, p < 0.0001). In multivariate regression analysis, OP increased odds for revision surgery at 1 year (OR 1.4) and 2 years (OR 1.5) following surgery (all p < 0.05). OP was also an independent predictor of readmission at all time points (90 days, OR 1.3, p < 0.005).
Conclusion
Medicare patients with OP had elevated rates of complications, reoperations, and outpatient costs after undergoing primary ASD surgery.
Similar content being viewed by others
References
Albert TJ, Purtill J, Mesa J, McIntosh T, Balderston RA (1995) Health outcome assessment before and after adult deformity surgery. A Prospective Study Spine 20(18):2002-p2005. https://doi.org/10.1097/00007632-199509150-00009
Bess S, Boachie-Adjei O, Burton D, Cunningham M, Shaffrey C, Shelokov A, Hostin R, Schwab F, Wood K, Akbarnia B & International Spine Study Group (2009) Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine 34(20):2186–2190
Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS (2002) Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine 27(7):776–786. https://doi.org/10.1097/00007632-200204010-00017
Lehman RA Jr, Kang DG, Wagner SC (2015) Management of osteoporosis in spine surgery. J Am Acad Orthop Surg 23(4):253–263. https://doi.org/10.5435/JAAOS-D-14-00042
Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M (2007) Glucocorticoid-induced osteoporosis: a systematic review and cost-utility analysis. Health Technol Assess (Winchester, England) 11(7):iii–231. https://doi.org/10.3310/hta11070
Martín-Fernández M, López-Herradón A, Piñera AR, Tomé-Bermejo F, Duart JM, Vlad MD, Rodríguez-Arguisjuela MG, Alvarez-Galovich L (2017) Potential risks of using cement-augmented screws for spinal fusion in patients with low bone quality. Spine J Official J North Am Spine Soc 17(8):1192–1199. https://doi.org/10.1016/j.spinee.2017.04.029
Weiser L, Huber G, Sellenschloh K, Viezens L, Püschel K, Morlock MM, Lehmann W (2017) Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur Spine J 26(11):2891–2897. https://doi.org/10.1007/s00586-017-5091-x
Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS 3rd, Cook SD (1994) Effects of bone mineral density on pedicle screw fixation. Spine 19(21):2415–2420. https://doi.org/10.1097/00007632-199411000-00008
Johnsson KE, Willner S, Johnsson K (1986) Postoperative instability after decompression for lumbar spinal stenosis. Spine 11(2):107–110. https://doi.org/10.1097/00007632-198603000-00001
Aihara T, Endo K, Sawaji Y, Suzuki H, Urushibara M, Kojima A, Matsuoka Y, Takamatsu T, Murata K, Kusakabe T, Maekawa A, Yamamoto K (2020) Five-year Reoperation Rates and Causes for Reoperations Following Lumbar Microendoscopic Discectomy and Decompression. Spine 45(1):71–77. https://doi.org/10.1097/BRS.0000000000003206
Wang M, Luo XJ, Ye YJ, Zhang Z (2019) Does Concomitant Degenerative Spondylolisthesis Influence the Outcome of Decompression Alone in Degenerative Lumbar Spinal Stenosis? A Meta-Analysis of Comparative Studies. World neurosurgery 123:226–238. https://doi.org/10.1016/j.wneu.2018.11.246
Manson NA, Phillips FM (2007) Minimally invasive techniques for the treatment of osteoporotic vertebral fractures. Instr Course Lect 56:273–285
Manson NA, Phillips FM (2006) Minimally invasive techniques for the treatment of osteoporotic vertebral fractures. J Bone Joint Surg 88(8):1862–1872
Poole KE, Compston JE (2006) Osteoporosis and its management BMJ (Clinical research ed) 333(7581):1251–1256
Thompson PW (2000) A fracture risk profile using single-site bone density assessment and clinical risk factors. J Clin Densitometry 3(1):73–77. https://doi.org/10.1385/jcd:3:1:073
Glassman SD, Alegre GM (2003) Adult spinal deformity in the osteoporotic spine: options and pitfalls. Instr Course Lect 52:579–588
Passias PG, Poorman GW, Bortz CA, Qureshi R, Diebo BG, Paul JC, Horn SR, Segreto FA, Pyne A, Jalai CM, Lafage V, Bess S, Schwab FJ, Hassanzadeh H (2018) Predictors of adverse discharge disposition in adult spinal deformity and associated costs. The Spine J 18(10):1845–1852. https://doi.org/10.1016/j.spinee.2018.03.022
Soroceanu, A., Burton, D. C., Oren, J. H., Smith, J. S., Hostin, R., Shaffrey, C. I., Akbarnia, B. A., Ames, C. P., Errico, T. J., Bess, S., Gupta, M. C., Deviren, V., Schwab, F. J., Lafage, V., & International Spine Study Group (2016) Medical Complications After Adult Spinal Deformity Surgery: Incidence, Risk Factors, and Clinical Impact. Spine 41(22):1718–1723. https://doi.org/10.1097/BRS.0000000000001636
Guzman JZ, Feldman ZM, McAnany S, Hecht AC, Qureshi SA, Cho SK (2016) Osteoporosis in Cervical Spine Surgery. Spine 41(8):662–668. https://doi.org/10.1097/BRS.0000000000001347
Girardi FP, Parvataneni HK, Sandhu HS, Cammisa FP Jr, Grewal H, Schneider R, Lane JM (2001) Correlation between vertebral body rotation and two-dimensional vertebral bone density measurement. Osteoporosis Int 12(9):738–740. https://doi.org/10.1007/s001980170049
Naresh-Babu J, Viswanadha AK, Ito M, Park JB (2019) What Should an Ideal Adult Spinal Deformity Classification System Consist of?: Review of the Factors Affecting Outcomes of Adult Spinal Deformity Management. Asian Spine J 13(4):694–703
Diebo BG, Shah NV, Boachie-Adjei O, Zhu F, Rothenfluh DA, Paulino CB, Schwab FJ, Lafage V (2019) Adult spinal deformity. Lancet (London, England) 394(10193):160–172. https://doi.org/10.1016/S0140-6736(19)31125-0
Good CR, Auerbach JD, O’Leary PT, Schuler TC (2011) Adult spine deformity. Curr Rev Musculoskelet Med 4(4):159–167. https://doi.org/10.1007/s12178-011-9101-z
Hoffmann MF, Jones CB, Sietsema DL (2016) Recombinant Human Bone Morphogenetic Protein-2 in Posterolateral Spinal Fusion: What’s the Right Dose? Asian spine journal 10(3):457–464. https://doi.org/10.4184/asj.2016.10.3.457
Bianco, K., Norton, R., Schwab, F., Smith, J. S., Klineberg, E., Obeid, I., Mundis, G., Jr, Shaffrey, C. I., Kebaish, K., Hostin, R., Hart, R., Gupta, M. C., Burton, D., Ames, C., Boachie-Adjei, O., Protopsaltis, T. S., Lafage, V., & International Spine Study Group (2014) Complications and intercenter variability of three-column osteotomies for spinal deformity surgery: a retrospective review of 423 patients. Neurosurg Focus 36(5):E18. https://doi.org/10.3171/2014.2.FOCUS1422
Cho KJ, Suk SI, Park SR, Kim JH, Kang SB, Kim HS, Oh SJ (2010) Risk factors of sagittal decompensation after long posterior instrumentation and fusion for degenerative lumbar scoliosis. Spine 35(17):1595–1601. https://doi.org/10.1097/BRS.0b013e3181bdad89
Schwab, F. J., Hawkinson, N., Lafage, V., Smith, J. S., Hart, R., Mundis, G., Burton, D. C., Line, B., Akbarnia, B., Boachie-Adjei, O., Hostin, R., Shaffrey, C. I., Arlet, V., Wood, K., Gupta, M., Bess, S., Mummaneni, P. V., & International Spine Study Group (2012) Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. European Spine J 21(12):2603–2610. https://doi.org/10.1007/s00586-012-2370-4
Auerbach JD, Lenke LG, Bridwell KH, Sehn JK, Milby AH, Bumpass D, Crawford CH 3rd, OʼShaughnessy, B. A., Buchowski, J. M., Chang, M. S., Zebala, L. P., & Sides, B. A. (2012) Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine 37(14):1198–1210. https://doi.org/10.1097/BRS.0b013e31824fffde
Pietschmann P, Rauner M, Sipos W, Kerschan-Schindl K (2009) Osteoporosis: an age-related and gender-specific disease–a mini-review. Gerontology 55(1):3–12. https://doi.org/10.1159/000166209
DeWald CJ, Stanley T (2006) Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine 31(19 Suppl):S144–S151. https://doi.org/10.1097/01.brs.0000236893.65878.39
Demir T, Camuşcu N, Türeyen K (2012) Design and biomechanical testing of pedicle screw for osteoporotic incidents. Proc Institut Mech Eng Part H J Eng Med 226(3):256–262
Formby PM, Kang DG, Helgeson MD, Wagner SC (2016) Clinical and Radiographic Outcomes of Transforaminal Lumbar Interbody Fusion in Patients with Osteoporosis. Global Spine J 6(7):660–664. https://doi.org/10.1055/s-0036-1578804
Inceoglu S, Ferrara L, McLain RF (2004) Pedicle screw fixation strength: pullout versus insertional torque. Spine J 4(5):513–518. https://doi.org/10.1016/j.spinee.2004.02.006
Bernstein DN, Kurucan E, Menga EN, Molinari RW, Rubery PT, Mesfin A (2018) Comparison of adult spinal deformity patients with and without rheumatoid arthritis undergoing primary non-cervical spinal fusion surgery: a nationwide analysis of 52,818 patients. Spine J 18(10):1861–1866. https://doi.org/10.1016/j.spinee.2018.03.020
Bjerke BT, Zarrabian M, Aleem IS, Fogelson JL, Currier BL, Freedman BA, Bydon M, Nassr A (2018) Incidence of Osteoporosis-Related Complications Following Posterior Lumbar Fusion. Global Spine J 8(6):563–569. https://doi.org/10.1177/2192568217743727
Yagi M, King AB, Boachie-Adjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis Minimum 5 years of follow-up. Spine 37(17):1479–1489
Pan ML, Chen LR, Tsao HM, Chen KH (2017) Iron Deficiency Anemia as a Risk Factor for Osteoporosis in Taiwan: A Nationwide Population-Based Study. Nutrients 9(6):616. https://doi.org/10.3390/nu9060616
Toxqui L, Vaquero MP (2015) Chronic iron deficiency as an emerging risk factor for osteoporosis: a hypothesis. Nutrients 7(4):2324–2344. https://doi.org/10.3390/nu7042324
Puvanesarajah V, Jain A, Cancienne JM, Stein BE, Novicoff WM, Shimer AL, Shen F, Hassanzadeh H (2017) BMP Use and the Risk of Revision Surgery After Long Posterolateral Fusions in the Elderly. Clinical Spine Surg 30(7):E931–E937. https://doi.org/10.1097/BSD.0000000000000489
Varshneya K, Pendharkar AV, Azad TD, Ratliff JK, Veeravagu A (2019) A Descriptive Analysis of Spinal Cord Arteriovenous Malformations: Clinical Features, Outcomes, and Trends in Management. World Neurosurg 131:e579–e585. https://doi.org/10.1016/j.wneu.2019.08.010
Azad TD, Vail D, Bentley J, Han SS, Suarez P, Varshneya K, Mittal V, Veeravagu A, Desai M, Bhattacharya J, Ratliff JK (2019) Initial Provider Specialty Is Associated With Long-term Opiate Use in Patients With Newly Diagnosed Low Back and Lower Extremity Pain. Spine 44(3):211–218. https://doi.org/10.1097/BRS.0000000000002840
Azad TD, Varshneya K, Ho AL, Veeravagu A, Sciubba DM, Ratliff JK (2019) Laminectomy Versus Corpectomy for Spinal Metastatic Disease-Complications, Costs, and Quality Outcomes. World Neurosurg 131:e468–e473. https://doi.org/10.1016/j.wneu.2019.07.206
Varshneya K, Stienen MN, Ho AL, Medress ZA, Fatemi P, Pendharkar AV, Ratliff JK, Veeravagu A (2020) Evaluating the Impact of Spinal Osteotomy on Surgical Outcomes of Thoracolumbar Deformity Correction. World Neurosurg 144:e774–e779. https://doi.org/10.1016/j.wneu.2020.09.072
Varshneya K, Jokhai RT, Fatemi P, Stienen MN, Medress ZA, Ho AL, Ratliff JK, Veeravagu A (2020) Predictors of 2-year reoperation in Medicare patients undergoing primary thoracolumbar deformity surgery. J Neurosurg Spine. https://doi.org/10.3171/2020.5.SPINE191425
Varshneya K, Medress ZA, Stienen MN, Nathan J, Ho A, Pendharkar AV, Loo S, Aikin J, Li G, Desai A, Ratliff JK, Veeravagu A (2021) A Comparative Analysis of Patients Undergoing Fusion for Adult Cervical Deformity by Approach Type. Global Spine J 11(5):626–632. https://doi.org/10.1177/2192568220915717
Varshneya K, Wadhwa H, Stienen MN, Ho AL, Medress ZA, Herrick DB, Desai A, Ratliff JK, Veeravagu A (2021) Single vs Multistage Surgical Management of Single and Two-Level Lumbar Degenerative Disease. World Neurosurg. https://doi.org/10.1016/j.wneu.2021.05.115
Varshneya K, Jokhai R, Medress ZA, Stienen MN, Ho A, Fatemi P, Ratliff JK, Veeravagu A (2021) Factors which predict adverse events following surgery in adults with cervical spinal deformity. The Bone & Joint J. https://doi.org/10.1302/0301-620X.103B4.BJJ-2020-0845.R2
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no financial interest in the subject under discussion.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Varshneya, K., Bhattacharjya, A., Jokhai, R.T. et al. The impact of osteoporosis on adult deformity surgery outcomes in Medicare patients. Eur Spine J 31, 88–94 (2022). https://doi.org/10.1007/s00586-021-06985-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06985-z