Abstract
Introduction
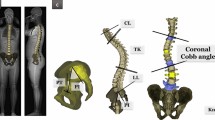
Standing radiographs allow analysis of spinal segments and their relative positioning. However, it requires a specific positioning influencing spinal alignment. Knowledge of trunk movements when walking is therefore an essential step to evaluate dynamic sagittal balance. Our objective was to define spinal junction kinematics and their correlations during gait in a healthy population.
Method
This is a prospective, single-center study. Between 2015 and 2017, 25 healthy volunteers were included. The measurements were taken in a motion analysis laboratory. Several kinematic parameters were studied, including spinal junction movements in the three planes and dynamic sagittal vertical axis (Dyn-SVA). Pearson correlation coefficients were calculated to determine the interactions between the spinal junctions.
Results
In the sagittal plane, the average amplitude of variation of the dyn-SVA was 25.5 cm (SD = 8.9). The average range of motion of the lumbosacral and thoracolumbar junction was approximately 3°, they operated in anti-phase during the gait cycle and were strongly correlated (r = −0.5069, p = 0.01). In the transverse plane, the anti-rotation of the upper body relative to the pelvis was mainly ensured by the opposite movements of the lumbosacral and thoracolumbar junction (r = 0.5689, p = 0.003). In the frontal plane, the lateral inclination in the lumbar region was made in the opposite direction from the pelvis toward the carrying member.
Conclusion
Although there is substantial inter-subject variability, our study characterized the angular movements in the three planes of the different spinal junctions, of the pelvis and the lower limbs during a gait cycle in a healthy population.






Similar content being viewed by others
References
Le Huec J-C, Gille O, Fabre T (2018) Sagittal balance and spine-pelvis relation: a French speciality? Orthop Traumatol Surg Res 104(5):551–554
Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V (2015) Sagittal alignment of the spine: what do you need to know? Clin Neurol Neurosurg 139:295–301
Dubousset J, Charpak G, Skalli W, Lavaste F, Kalifa G (2005) A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull Acad Natl Med 189:287–297
Hasegawa K, Okamoto M, Hatsushikano S, Shimoda H, Ono M, Watanabe K (2016) Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J 25(11):3675–3686
Lafage R, Schwab F, Challier V, Henry JK, Gum J, Smith J et al (2016) Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine 41(1):62–68
Moal B, Lafage V, Smith JS, Ames CP, Mundis G, Terran JS et al (2015) Clinical improvement through surgery for adult spinal deformity: what can be expected and who is likely to benefit most? Spine Deform 3(6):566–574
Lee NJ, Kothari P, Kim JS, Shin JI, Phan K, Di Capua J et al (2017) Early complications and outcomes in adult spinal deformity surgery: an NSQIP study based on 5803 patients. Glob Spine J 7(5):432–440
Smith JS, Klineberg E, Schwab F, Shaffrey CI, Moal B, Ames CP et al (2013) Change in classification grade by the SRS-Schwab adult spinal deformity classification predicts impact on health-related quality of life measures: prospective analysis of operative and nonoperative treatment. Spine (Phila Pa 1976) 38(19):1663–71
Smith JS, Klineberg E, Schwab F, Shaffrey CI, Moal B, Ames CP et al (2013) Change in classification grade by the SRS-Schwab adult spinal deformity classification predicts impact on health-related quality of life measures: prospective analysis of operative and nonoperative treatment. Spine 38(19):1663–1671
Pesenti S, Prost S, Pomero V, Authier G, Roscigni L, Viehweger E, Blondel B, Jouve JL (2020) Does static trunk motion analysis reflect its true position during daily activities in adolescent with idiopathic scoliosis? Orthop Traumatol Surg Res 106(7):1251-1256
Blonde B, Viehweger E, Fuentes S, Bollini G et al (2015) Postural spinal balance defined by net intersegmental moments: results of a biomechanical approach and experimental errors measurement. World J Orthop 6(11):983–990
Sutherland DH (2002) The evolution of clinical gait analysis: part II kinematics. Gait Posture 16(2):159–179
Charnley J (1966) La Marche et les Boiteries. Étude des Marches Normales et Pathologiques. (A Study of Normal and Abnormal Gait.). J Bone Joint Surg Br 48-B(2):403–403
Waters RL, Morris J, Perry J (1973) Translational motion of the head and trunk during normal walking. J Biomech 6(2):167–172
Crosbie J, Vachalathiti R, Smith R (1997) Patterns of spinal motion during walking. Gait Posture 5(1):6–12
Crosbie J, Vachalathiti R, Smith R (1997) Age, gender and speed effects on spinal kinematics during walking. Gait Posture 5(1):13–20
Blondel B, Pomero V, Moal B, Lafage V, Jouve J-L, Tropiano P et al (2012) Sagittal spine posture assessment: feasibility of a protocol based on intersegmental moments. Orthop Traumatol Surg Res 98(1):109–113
Pesenti S, Prost S, Blondel B, Pomero V, Severyns M, Roscigni L et al (2019) Correlations linking static quantitative gait analysis parameters to radiographic parameters in adolescent idiopathic scoliosis. Orthop Traumatol Surg Res 105(3):541–545
Mulroy S, Gronley J, Weiss W, Newsam C, Perry J (2003) Use of cluster analysis for gait pattern classification of patients in the early and late recovery phases following stroke. Gait Posture 18(1):114–125
Pesenti S, Blondel B, Peltier E, Viehweger E, Pomero V, Authier G et al (2017) Spinal alignment evolution with age: a prospective gait analysis study. World J Orthop 8(3):256–263
Oh CH, Yoon SH (2017) Whole spine disc degeneration survey according to the ages and sex using pfirrmann disc degeneration grades. Korean J Spine 14(4):148–154
Jean D, Pierre D, Robert D. (1968) Walking and limping; a study of normal and pathological walking [by] Robert Ducroquet, Jean Ducroquet [and] Pierre Ducroquet, with the collaboration of Marcel Saussez. Illustrated by Marcel Dudouet. Pref. by Emanuel Kaplan. Translated by William S. Hunter and Jep Hunter. Philadelphia: Lippincott. 284 p
Ceccato J-C, de Sèze M, Azevedo C, Cazalets J-R (2009) Comparison of trunk activity during gait initiation and walking in humans. PLoS ONE 4(12):e8193
Bruijn SM, Meijer OG, van Dieën JH, Kingma I, Lamoth CJC (2008) Coordination of leg swing, thorax rotations, and pelvis rotations during gait: the organisation of total body angular momentum. Gait Posture 27(3):455–462
Seay JF, Van Emmerik REA, Hamill J (2011) Low back pain status affects pelvis-trunk coordination and variability during walking and running. Clin Biomech 26(6):572–578
Lamoth CJC, Beek PJ, Meijer OG (2002) Pelvis–thorax coordination in the transverse plane during gait. Gait Posture 16(2):101–114
Selles RW, Wagenaar RC, Smit TH, Wuisman PIJM (2001) Disorders in trunk rotation during walking in patients with low back pain: a dynamical systems approach. Clin Biomech 16(3):175–181
Pesenti S, Pomero V, Prost S, Severyns M, Authier G, Roscigni L et al (2020) Curve location influences spinal balance in coronal and sagittal planes but not transversal trunk motion in adolescents with idiopathic scoliosis: a prospective observational study. Eur Spine J. https://doi.org/10.1007/s00586-020-06361-3 (Epub ahead of print)
Wu WH, Lin XC, Meijer OG, Gao JT, Hu H, Prins MR et al (2014) Effects of experimentally increased trunk stiffness on thorax and pelvis rotations during walking. Hum Mov Sci 33:194–202
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest related to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Prost, S., Blondel, B., Pomero, V. et al. Description of spine motion during gait in normal adolescents and young adults. Eur Spine J 30, 2520–2530 (2021). https://doi.org/10.1007/s00586-021-06918-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06918-w