Abstract
Purpose
Inappropriate use of MRI leads to increasing interventions and surgeries for low back pain (LBP). We probed the potential effects of a routine MRI report on the patient’s perception of his spine and functional outcome of treatment. An alternate ‘clinical reporting’ was developed and tested for benefits on LBP perception.
Methods
In Phase-I, 44 LBP patients were randomized to Group A who had a factual explanation of their MRI report or Group B, who were reassured that the MRI findings showed normal changes. The outcome was compared at 6 weeks by VAS, PSEQ-2, and SF-12. In Phase-II, clinical reporting was developed, avoiding potential catastrophizing terminologies. In Phase-III, 20 MRIs were reported by both routine and clinical methods. The effects of the two methods were tested on four categories of health care professionals (HCP) who read them blinded on their assessment of severity of disease, possible treatment required, and the probability of surgery.
Results
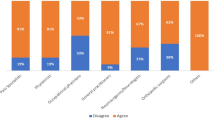
Both groups were comparable initial by demographics and pain. After 6 weeks of treatment, Group A had a more negative perception of their spinal condition, increased catastrophization, decreased pain improvement, and poorer functional status(p = significant for all). The alternate method of clinical reporting had significant benefits in assessment of lesser severity of the disease, shift to lesser severity of intervention and surgery in three groups of HCPs.
Conclusion
Routine MRI reports produce a negative perception and poor functional outcomes in LBP. Focussed clinical reporting had significant benefits, which calls for the need for ‘clinical reporting’ rather than ‘Image reporting’.







Similar content being viewed by others
References
Chou R, Qaseem A, Snow V et al (2007) Diagnosis and treatment of low back pain: a joint clinical practice guideline from the american college of physicians and the american pain society. Ann Intern Med 147:478–491. https://doi.org/10.7326/0003-4819-147-7-200710020-00006
Andersen JC (2011) Is immediate imaging important in managing low back pain? J Athl Train 46:99–102. https://doi.org/10.4085/1062-6050-46.1.99
Lurie JD, Birkmeyer NJ, Weinstein JN (2003) Rates of advanced spinal imaging and spine surgery. Spine 28:616–620. https://doi.org/10.1097/01.BRS.0000049927.37696.DC
Martin BI, Mirza SK, Comstock BA et al (2007) Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine 32:382–387. https://doi.org/10.1097/01.brs.0000254104.55716.46
Mafi JN, McCarthy EP, Davis RB, Landon BE (2013) Worsening trends in the management and treatment of back pain. JAMA Intern Med 173:1573–1581. https://doi.org/10.1001/jamainternmed.2013.8992
Weinstein JN, Lurie JD, Olson PR et al (2006) United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine 31:2707–2714. https://doi.org/10.1097/01.brs.0000248132.15231.fe
Shreibati JB, Baker LC (2011) The relationship between low back magnetic resonance imaging, surgery, and spending: impact of physician self-referral status. Health Serv Res 46:1362–1381. https://doi.org/10.1111/j.1475-6773.2011.01265.x
Verrilli D, Welch HG (1996) The impact of diagnostic testing on therapeutic interventions. JAMA 275:1189–1191
Emery DJ, Shojania KG, Forster AJ et al (2013) Overuse of magnetic resonance imaging. JAMA Intern Med 173:823–825. https://doi.org/10.1001/jamainternmed.2013.3804
Chou R, Fu R, Carrino JA, Deyo RA (2009) Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet. https://doi.org/10.1016/S0140-6736(09)60172-0
Hartvigsen J, Hancock MJ, Kongsted A et al (2018) What low back pain is and why we need to pay attention. Lancet 391:2356–2367. https://doi.org/10.1016/S0140-6736(18)30480-X
Buchbinder R, van Tulder M, Öberg B et al (2018) Low back pain: a call for action. Lancet 391:2384–2388. https://doi.org/10.1016/S0140-6736(18)30488-4
Wu A, March L, Zheng X et al (2020) Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. https://doi.org/10.21037/atm.2020.02.175
Majid K, Truumees E (2008) Epidemiology and natural history of low back pain. Semin Spine Surg 20:87–92. https://doi.org/10.1053/j.semss.2008.02.003
Tonosu J, Oka H, Higashikawa A et al (2017) The associations between magnetic resonance imaging findings and low back pain: a 10-year longitudinal analysis. PLoS ONE. https://doi.org/10.1371/journal.pone.0188057
Webster BS, Bauer AZ, Choi Y et al (2013) Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain. Spine 38:1939–1946. https://doi.org/10.1097/BRS.0b013e3182a42eb6
Galambos A, Szabó E, Nagy Z et al (2019) A systematic review of structural and functional MRI studies on pain catastrophizing. J Pain Res 12:1155–1178. https://doi.org/10.2147/JPR.S192246
Lehnert BE, Bree RL (2010) Analysis of appropriateness of outpatient CT and MRI referred from primary care clinics at an academic medical center: how critical is the need for improved decision support? J Am Coll Radiol JACR 7:192–197. https://doi.org/10.1016/j.jacr.2009.11.010
Flynn TW, Smith B, Chou R (2011) Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good. J Orthop Sports Phys Ther 41:838–846. https://doi.org/10.2519/jospt.2011.3618
Chou R, Deyo RA, Jarvik JG (2012) Appropriate use of lumbar imaging for evaluation of low back pain. Radiol Clin N Am 50:569–585. https://doi.org/10.1016/j.rcl.2012.04.005
You JJ, Levinson W, Laupacis A (2009) Attitudes of family physicians, specialists and radiologists about the use of computed tomography and magnetic resonance imaging in ontario. Healthc Policy 5:54–65
Downie A, Hancock M, Jenkins H et al (2020) How common is imaging for low back pain in primary and emergency care? Systematic review and meta-analysis of over 4 million imaging requests across 21 years. Br J Sports Med 54:642–651. https://doi.org/10.1136/bjsports-2018-100087
Wáng YXJ, Wu A-M, Ruiz Santiago F, Nogueira-Barbosa MH (2018) Informed appropriate imaging for low back pain management: a narrative review. J Orthop Transl 15:21–34. https://doi.org/10.1016/j.jot.2018.07.009
Chou R, Qaseem A, Owens DK, Shekelle P (2011) Diagnostic imaging for low back pain: advice for high-value health care from the american college of physicians. Ann Intern Med 154:181–189. https://doi.org/10.7326/0003-4819-154-3-201102010-00008
Turk DC, Fillingim RB, Ohrbach R, Patel KV (2016) Assessment of psychosocial and functional impact of chronic pain. J Pain 17(9):T21–T49
Farivar SS, Cunningham WE, Hays RD (2007) Correlated physical and mental health summary scores for the SF-36 and SF-12 Health Survey, vol 1. Health Qual Life Outcomes 5:54. https://doi.org/10.1186/1477-7525-5-54
Garland EL (2012) Pain processing in the human nervous system: a selective review of nociceptive and biobehavioral pathways. Prim Care 39:561–571. https://doi.org/10.1016/j.pop.2012.06.013
Lim YZ, Chou L, Au RT et al (2019) People with low back pain want clear, consistent and personalised information on prognosis, treatment options and self-management strategies: a systematic review. J Physiother 65:124–135. https://doi.org/10.1016/j.jphys.2019.05.010
Tonsaker T, Bartlett G, Trpkov C (2014) Health information on the Internet. Can Fam Physician 60:407–408
Vismara M, Caricasole V, Starcevic V et al (2020) Is cyberchondria a new transdiagnostic digital compulsive syndrome? A systematic review of the evidence. Compr Psychiatry. https://doi.org/10.1016/j.comppsych.2020.152167
Rhodes LA, McPhillips-Tangum CA, Markham C, Klenk R (1999) The power of the visible: the meaning of diagnostic tests in chronic back pain. Soc Sci Med 48:1189–1203. https://doi.org/10.1016/S0277-9536(98)00418-3
Karran EL, Medalian Y, Hillier SL, Moseley GL (2017) The impact of choosing words carefully: an online investigation into imaging reporting strategies and best practice care for low back pain. PeerJ. https://doi.org/10.7717/peerj.4151
Ash LM, Modic MT, Obuchowski NA et al (2008) Effects of diagnostic information, per se, on patient outcomes in acute radiculopathy and low back pain. Am J Neuroradiol 29:1098–1103. https://doi.org/10.3174/ajnr.A0999
Bentley TGK, Effros RM, Palar K, Keeler EB (2008) Waste in the U.S. health care system: a conceptual framework. Milbank Q 86:629–659. https://doi.org/10.1111/j.1468-0009.2008.00537.x
Acknowledgements
All authors had significant contribution for the study. SR conceptualised and oversaw the study with writing of the manuscript. DCR was involved in conducting the study and preparing the manuscript. PBT was involved in Phase-II and Phase-III and was instrumental in devising enhanced method of reporting. RMK and APS provided the clinical inputs and participated in manuscript preparation.
Funding
The project was funded by Ganga Orthopaedic Research & Education Foundation (GOREF 2016–07).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was performed after approval of the IRB committee.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rajasekaran, S., Dilip Chand Raja, S., Pushpa, B.T. et al. The catastrophization effects of an MRI report on the patient and surgeon and the benefits of ‘clinical reporting’: results from an RCT and blinded trials. Eur Spine J 30, 2069–2081 (2021). https://doi.org/10.1007/s00586-021-06809-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06809-0