Abstract
Purpose
The mean potential of lordosis restoration by transforaminal lumbar interbody fusion (TLIF) is supposed to be low in general. In contrast, clinical experience shows a wide range of segmental lordosis correction. In this study, the predictability of lordosis correction should be investigated.
Methods
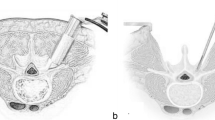
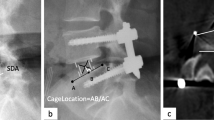
Prospectively collected register data were analyzed retrospectively. One hundred twenty-one consecutive patients (2014–2016) operated with single-level TLIF L4/5 (10°-lordotic cage). Segmental lordosis (L4/5) and overall lordosis (L1–S1) were measured on lumbar X-rays: preoperatively (pre), after 3–5 days (post), at least 24 months postoperatively (2yFU). Outcome and satisfaction of patients were assessed. Parameters were statistically compared by students t-tests (a = 0.05). In addition, predictors of correction were analyzed.
Results
Age was 60.7 years, rate of 2yFU 41.3% (n = 50). Lordosis correction L4/5 was statistically significant with (post–pre) 4.9 ± 5.7° (p < 0.01), but not significant for L1–S1 (post–pre) 1.6 ± 8.0° (p = 0.3). A strong–moderate correlation of lordosis L4/5 (pre) and lordosis correction L4/5 (post–pre) was shown (r = − 0.6, p < 0,01). In a rising range of preoperative lordosis L4/5 from 15–30° the likelihood of lordosis loss increased. In 2yFU correction, L4/5 was significant with (post–pre) 5.4 ± 5.4° (p < 0.01), no significant long-term change (2yFU-postop) − 1.5 ± 4.9° (p = 0.2). No correlation (r = − 0.1) of correction and ODI. VAS-B improved by means of 2.9, VAS-L by 2.5, ODI by 19.1% (pre vs. 2yFU), each statistically significant (p < 0.01).
Conclusion
Significant segmental relordosation can be performed by TLIF L4/5. The potential of correction strongly correlates with preoperative lordosis. Therefore, TLIF technique should be considered carefully in cases with a preoperative segmental lordosis of more than 15° and additional need of lordosation.





Similar content being viewed by others
References
Quante M, Kesten H, Richter A, Halm H (2012) Transforaminal lumbar interbody fusion for the treatment of degenerative spondylolisthesis. Orthopade 41(2):153–162. https://doi.org/10.1007/s00132-011-1832-4
Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, Liu JC (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7(4):379–386. https://doi.org/10.3171/SPI-07/10/379
Ajiboye RM, Alas H, Mosich GM, Sharma A, Pourtaheri S (2018) Radiographic and clinical outcomes of anterior and transforaminal lumbar interbody fusions: a systematic review and meta-analysis of comparative studies. Clin Spine Surg 31(4):E230–E238. https://doi.org/10.1097/BSD.0000000000000549
Dorward IG, Lenke LG, Bridwell KH, O’Leary PT, Stoker GE, Pahys JM, Kang MM, Sides BA, Koester LA (2013) Transforaminal versus anterior lumbar interbody fusion in long deformity constructs: a matched cohort analysis. Spine (Phila Pa 1976) 38(12):E755-762. https://doi.org/10.1097/BRS.0b013e31828d6ca3
Kim JS, Lee KY, Lee SH, Lee HY (2010) Which lumbar interbody fusion technique is better in terms of level for the treatment of unstable isthmic spondylolisthesis? J Neurosurg Spine 12(2):171–177. https://doi.org/10.3171/2009.9.SPINE09272
Robertson PA, Armstrong WA, Woods DL, Rawlinson JJ (2018) Lordosis recreation in transforaminal and posterior lumbar interbody fusion. Spine 43(22):E1350–E1357. https://doi.org/10.1097/brs.0000000000002705
Zhu C, Qiu X, Zhuang M, Cheng D, Liu Z (2018) Surgical outcomes of single-level transforaminal lumbar interbody fusion for degenerative spondylolisthesis with and without kyphotic alignment. World Neurosurg 117:e396–e402. https://doi.org/10.1016/j.wneu.2018.06.042
Pesenti S, Lafage R, Stein D, Elysee JC, Lenke LG, Schwab FJ, Kim HJ, Lafage V (2018) The amount of proximal lumbar lordosis is related to pelvic incidence. Clin Orthop Relat Res 476(8):1603–1611. https://doi.org/10.1097/CORR.0000000000000380
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30(3):346–353. https://doi.org/10.1097/01.brs.0000152379.54463.65
Crandall DG, Revella RN (2009) Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis. Spine (Phila Pa 1976) 34(20):2126–2133. https://doi.org/10.1097/BRS.0b013e3181b612db
Tempel ZJ, Gandhoke GS, Bolinger BD, Khattar NK, Parry PV, Chang YF, Okonkwo DO, Kanter AS (2017) The influence of pelvic incidence and lumbar lordosis mismatch on development of symptomatic adjacent level disease following single-level transforaminal lumbar interbody fusion. Neurosurgery 80(6):880–886. https://doi.org/10.1093/neuros/nyw073
Hemanta D, Jiang X-x, Feng Z-z, Chen Z-x, Cao Y-w (2016) Etiology for degenerative disc disease. Chin Med Sci J 31(3):185–191. https://doi.org/10.1016/s1001-9294(16)30049-9
Koreckij TD, Fischgrund JS (2015) Degenerative spondylolisthesis. J Spinal Disord Tech 28(7):236–241. https://doi.org/10.1097/BSD.0000000000000298
Matz PG, Meagher RJ, Lamer T, Tontz WL Jr, Annaswamy TM, Cassidy RC, Cho CH, Dougherty P, Easa JE, Enix DE, Gunnoe BA, Jallo J, Julien TD, Maserati MB, Nucci RC, O’Toole JE, Rosolowski K, Sembrano JN, Villavicencio AT, Witt JP (2016) Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J 16(3):439–448. https://doi.org/10.1016/j.spinee.2015.11.055
Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U (2005) Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 14(6):551–558. https://doi.org/10.1007/s00586-004-0830-1
Harms JG, Jeszensky D (1998) Die posteriore, lumbale, interkorporelle Fusion in unilateraler transforaminaler Technik. Orthop Traumatol 10:1998. https://doi.org/10.1007/s00064-006-0112-7
Javernick MA, Kuklo TR, Polly DW (2003) Transforaminal lumbar interbody fusion: unilateral versus bilateral disk removal-an in vivo study. Am J Orthop 32(7):344–348
Schwab F, Blondel B, Chay E, Demakakos J, Lenke L, Tropiano P, Ames C, Smith JS, Shaffrey CI, Glassman S, Farcy JP, Lafage V (2014) The comprehensive anatomical spinal osteotomy classification. Neurosurgery 74(1):112–120. https://doi.org/10.1227/NEU.0000000000000182o
Schomacher J (2008) Gütekriterien der visuellen Analogskala zur Schmerzbewertung. Physioscience 4(03):125–133. https://doi.org/10.1055/s-2008-1027685
Fairbank JC, Pynsent PB (2000) The oswestry disability index. Spine (Phila Pa 1976) 25(22):2940–2952. https://doi.org/10.1097/00007632-200011150-00017
Asher AL, Kerezoudis P, Mummaneni PV, Bisson EF, Glassman SD, Foley KT, Slotkin JR, Potts EA, Shaffrey ME, Shaffrey CI, Coric D, Knightly JJ, Park P, Fu KM, Devin CJ, Archer KR, Chotai S, Chan AK, Virk MS, Bydon M (2018) Defining the minimum clinically important difference for grade I degenerative lumbar spondylolisthesis: insights from the quality outcomes database. Neurosurg Focus 44(1):E2. https://doi.org/10.3171/2017.10.FOCUS17554
Kim JS, Kang BU, Lee SH, Jung B, Choi YG, Jeon SH, Lee HY (2009) Mini-transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion augmented by percutaneous pedicle screw fixation: a comparison of surgical outcomes in adult low-grade isthmic spondylolisthesis. J Spinal Disord Tech 22(2):114–121. https://doi.org/10.1097/BSD.0b013e318169bff5
Rhee C, Visintini S, Dunning CE, Oxner WM, Glennie RA (2017) Does restoration of focal lumbar lordosis for single level degenerative spondylolisthesis result in better patient-reported clinical outcomes? A systematic literature review. J Clin Neurosci 44:95–100. https://doi.org/10.1016/j.jocn.2017.06.039
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The author(s) declared no potential conflicts of interest with respect to research, authorship and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Berlin, C., Zang, F., Halm, H. et al. Preoperative lordosis in L4/5 predicts segmental lordosis correction achievable by transforaminal lumbar interbody fusion. Eur Spine J 30, 1277–1284 (2021). https://doi.org/10.1007/s00586-020-06710-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06710-2