Abstract
Purpose
The traditional teaching has been that proper function of a cervical disc replacement is dependent upon appropriate placement, which includes centering the device in the coronal plane. The purpose of this study was to identify the most reliable anatomical landmark for determining midline placement of an implant within the cervical disc space under fluoroscopy.
Methods
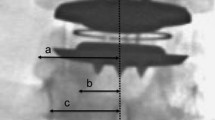
Digital fluoroscopy images were taken for each cervical level at 0 °, 2.5 °, 5 °, 7.5 °, 10 °, and 15 ° from the mid-axis by rotating the C-arm beam of six cadavers. Thin-slice CT scanning of the same levels was subsequently performed. Three independent reviewers measured the distance between anatomic structures: (a) tip of the right uncinate; (b) medial border of the right pedicle; and (c) center of the spinous processes for different x-ray angles across cervical levels C3–7.
Results
Both the uncinate and pedicle demonstrated superior overall accuracy to that of the spinous process (p ≤ 0.02) at all angles except at 0 ° for the pedicle where the difference was not statistically significant. Overall (pooled C3–7), the accuracy of the uncinate did not differ significantly from that of the pedicle at any fluoroscopic angle. The center of the spinous process measurement was particularly sensitive to deviations from the perfect anteroposterior fluoroscopy image.
Conclusions
The results of this investigation suggest that the tip of the uncinate and the medial border of the pedicle are more accurate measures of midline in the cervical spine than the center of the spinous process and are less susceptible to inadvertent off-axis imaging.



Similar content being viewed by others
References
Kerezoudis P, Alvi MA, Goyal A, Ubl DS, Meyer J, Habermann EB, Currier BL, Bydon M (2018) Commentary: utilization trends of cervical disk replacement in the United States. Oper Neurosurg Hagerstown 15:40–43. https://doi.org/10.1093/ons/opy181
Wang QL, Tu ZM, Hu P, Kontos F, Li YW, Li L, Dai YL, Lv GH, Wang B (2020) Long-term results comparing cervical disc arthroplasty to anterior cervical discectomy and fusion: a systematic review and meta-analysis of randomized controlled trials. Orthop Surg 12:16–30. https://doi.org/10.1111/os.12585
Finn MA, Boylan A, Anderson PA (2016) Chapter 7: Cervical disc replacement. In: Rhee JM, Boden SD, Weisel SW (eds) In: Operative techniques in spine surgery. Wolters Kluwer, Netherlands, pp 60–72
McAfee PC, Cunningham B, Holsapple G, Adams K, Blumenthal S, Guyer RD, Dmietriev A, Maxwell JH, Regan JJ (1976) A prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part II: evaluation of radiographic outcomes and correlation of surgical technique accuracy with clinical outcome. Spine Phila Pa 1976 30:1576–1583 (discussion E1388–1590)
Han KS, Kim K, Park WM, Lim DS, Kim YH (2013) Effect of centers of rotation on spinal loads and muscle forces in total disk replacement of lumbar spine. Proc Inst Mech Eng H 227:543–550. https://doi.org/10.1177/0954411912474742
Rohlmann A, Lauterborn S, Dreischarf M, Schmidt H, Putzier M, Strube P, Zander T (2013) Parameters influencing the outcome after total disc replacement at the lumbosacral junction. part 1: misalignment of the vertebrae adjacent to a total disc replacement affects the facet joint and facet capsule forces in a probabilistic finite element analysis. Eur Spine J 22:2271–2278. https://doi.org/10.1007/s00586-013-2909-z
Strube P, Hoff EK, Schurings M, Schmidt H, Dreischarf M, Rohlmann A, Putzier M (2013) Parameters influencing the outcome after total disc replacement at the lumbosacral junction. part 2: distraction and posterior translation lead to clinical failure after a mean follow-up of 5 years. Eur Spine J 22:2279–2287. https://doi.org/10.1007/s00586-013-2967-2
Zigler JE, Delamarter RB (2012) Five-year results of the prospective, randomized, multicenter, food and drug administration investigational device exemption study of the prodisc-L total disc replacement versus circumferential arthrodesis for the treatment of single-level degenerative disc disease. J Neurosurg Spine 17:493–501. https://doi.org/10.3171/2012.9.SPINE11498
Mikhael M, Brooks JT, Akpolat YT, Cheng WK (2017) Rotation effect and anatomic landmark accuracy for midline placement of lumbar artificial disc under fluoroscopy. Eur Spine J 26:794–798. https://doi.org/10.1007/s00586-015-3990-2
Wagner SC, Formby PM, Kang DG, Van Blarcum GS, Cody JP, Tracey RW, Lehman RA Jr (2016) Persistent axial neck pain after cervical disc arthroplasty: a radiographic analysis. Spine J 16:851–856. https://doi.org/10.1016/j.spinee.2016.02.043
Aronson N, Filtzer DL, Bagan M (1968) Anterior cervical fusion by the smith-robinson approach. J Neurosurg 29:396–404
Guyer RD, Voronov LI, Havey RM, Khayatzadeh S, Carandang G, Blank KR, Werner S, Rubin J, Padovani N, Patwardhan AG (2018) Kinematic assessment of an elastic-core cervical disc prosthesis in one and two-level constructs. JOR Spine 1:e1040. https://doi.org/10.1002/jsp2.1040
Rihn JA, Radcliff K, Hipp J, Vaccaro AR, Hilibrand AS, Anderson DG, Albert TJ (2015) Radiographic variables that may predict clinical outcomes in cervical disk replacement surgery. J Spinal Disord Tech 28:106–113. https://doi.org/10.1097/BSD.0b013e31826a0c84
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethical standards
I have no potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Derman, P.B., Waldorff, E., Zhang, N. et al. Accuracy of various fluoroscopic landmarks for determination of midline implant placement within the cervical disc space. Eur Spine J 30, 554–559 (2021). https://doi.org/10.1007/s00586-020-06638-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06638-7