Abstract
Purpose
The purpose of this study was to compare the degeneration of sacroiliac joints (SIJs) between adult spinal deformity (ASD) patients with sagittal imbalance and an age- and sex-matched lumbar spinal stenosis (LSS) patients without sagittal imbalance.
Materials and methods
The age- and sex-matched case–control study consists of two groups: the ASD group and the other group consisting of patients with LSS (LSS group). The study population consisted of 98 patients in each group. The spinopelvic parameters such as pelvic incidence (PI), sacral slope, pelvic tilt, lumbar lordosis, and sagittal vertical axis (SVA) were measured. To evaluate degeneration of SIJ, two protocols (Backlund's grade and Eno’s classification) were used.
Result
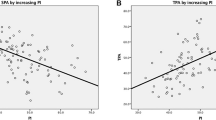
SIJ degeneration in the ASD group was more severe than that in the LSS group, as assessed by both Backlund’s grade and Eno’s classification (P < 0.001 for both). Age correlated significantly with PI in both the ASD and LSS groups (r = 0.285; P = 0.005, r = 0.218; P = 0.031, respectively). The total Backlund’s grading score and the SVA were significantly correlated with PI in the ASD group (r = 0.344; P < 0.001, r = 0.276; P = 0.007, respectively), but not in the LSS group (r = 0.156; P = 0.126, r = 0.189; P = 0.067, respectively).
Conclusions
ASD patients with sagittal imbalance demonstrated more severe SIJ degeneration compared to the age- and sex-matched LSS group. PI was significantly correlated with both SIJ degeneration and SVA only in the ASD group.




Similar content being viewed by others
References
Ailon T, Smith JS, Shaffrey CI, Lenke LG, Brodke D, Harrop JS, Fehlings M, Ames CP (2015) Degenerative spinal deformity. Neurosurgery 77(4):S75–91. https://doi.org/10.1227/neu.0000000000000938
Celestre PC, Dimar JR 2nd, Glassman SD (2018) Spinopelvic parameters: lumbar lordosis, pelvic incidence, pelvic tilt, and sacral slope: what does a spine surgeon need to know to plan a lumbar deformity correction? Neurosurg Clin N Am 29(3):323–329. https://doi.org/10.1016/j.nec.2018.03.003
Makhni MC, Shillingford JN, Laratta JL, Hyun SJ, Kim YJ (2018) Restoration of sagittal balance in spinal deformity surgery. J Korean Neurosurg Soc 61(2):167–179. https://doi.org/10.3340/jkns.2017.0404.013
Chaleat-Valayer E, Mac-Thiong JM, Paquet J, Berthonnaud E, Siani F, Roussouly P (2011) Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J 20(Suppl 5):634–640. https://doi.org/10.1007/s00586-011-1931-2
Pumberger M, Schmidt H, Putzier M (2018) Spinal deformity surgery: a critical review of alignment and balance. Asian Spine J 12(4):775–783. https://doi.org/10.31616/asj.2018.12.4.775
Kim WJ, Ma CH, Kim SH, Min YS, Lee JW, Chang SH, Park KH, Park KY, Song DG, Choy WS (2019) Prevention of adjacent segmental disease after fusion in degenerative spinal disorder: correlation between segmental lumbar lordosis ratio and pelvic incidence-lumbar lordosis mismatch for a minimum 5-year follow-up. Asian Spine J 13(4):654–662. https://doi.org/10.31616/asj.2018.0279
Schwab F, Lafage V, Patel A (1828) Farcy JP (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine 34(17):1833. https://doi.org/10.1097/BRS.0b013e3181a13c08
Bao H, Liabaud B, Varghese J, Lafage R, Diebo BG, Jalai C, Ramchandran S, Poorman G, Errico T, Zhu F, Protopsaltis T, Passias P, Buckland A, Schwab F, Lafage V (2018) Lumbosacral stress and age may contribute to increased pelvic incidence: an analysis of 1625 adults. Eur Spine J 27(2):482–488. https://doi.org/10.1007/s00586-017-5324-z
Jentzsch T, Geiger J, Bouaicha S, Slankamenac K, Nguyen-Kim TD, Werner CM (2013) Increased pelvic incidence may lead to arthritis and sagittal orientation of the facet joints at the lower lumbar spine. BMC Med Imaging 13:34. https://doi.org/10.1186/1471-2342-13-34
Kiapour A, Joukar A, Elgafy H, Erbulut DU, Agarwal AK, Goel VK (2020) Biomechanics of the sacroiliac joint: anatomy, function, biomechanics, sexual dimorphism, and causes of pain. Int J Spine Surg 14(Suppl 1):3–13. https://doi.org/10.14444/6077
Legaye J, Duvalbeaupere G (2008) Gravitational forces and sagittal shape of the spine. Clinical estimation of their relations. Int Orthop 32(6):809–816. https://doi.org/10.1007/s00264-007-0421-y
Legaye J (2014) Influence of age and sagittal balance of the spine on the value of the pelvic incidence. Eur Spine J 23(7):1394–1399. https://doi.org/10.1007/s00586-014-3207-0
Gebhart JJ, Weinberg DS, Bohl MS, Liu RW (2016) Relationship between pelvic incidence and osteoarthritis of the hip. Bone Joint Res 5(2):66–72. https://doi.org/10.1302/2046-3758.52.2000552
Ivanov AA, Kiapour A, Ebraheim NA, Goel V (2009) Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine 34(5):E162–E169. https://doi.org/10.1097/BRS.0b013e3181978ea3
Eno JJ, Boone CR, Bellino MJ, Bishop JA (2015) The prevalence of sacroiliac joint degeneration in asymptomatic adults. J Bone Joint Surg Am 97(11):932–936. https://doi.org/10.2106/JBJS.N.01101
Backlund J, Clewett Dahl E, Skorpil M (2017) Is CT indicated in diagnosing sacroiliac joint degeneration? Clin Radiol 72(8):e699–e693. https://doi.org/10.1016/j.crad.2017.03.006
Merrill RK, Kim JS, Leven DM, Kim JH, Meaike JJ, Bronheim RS, Suchman KI, Nowacki D, Gidumal SS, Cho SK (2018) Differences in fundamental sagittal pelvic parameters based on age, sex, and race. Clin Spine Surg 31(2):E109–E114. https://doi.org/10.1097/bsd.0000000000000555
Jacobs E, van Royen BJ, van Kuijk SMJ, Merk JMR, Stadhouder A, van Rhijn LW, Willems PC (2019) Prediction of mechanical complications in adult spinal deformity surgery-the GAP score versus the Schwab classification. Spine J 19(5):781–788. https://doi.org/10.1016/j.spinee.2018.11.013
Bari TJ, Ohrt-Nissen S, Hansen LV, Dahl B, Gehrchen M (2019) Ability of the global alignment and proportion score to predict mechanical failure following adult spinal deformity surgery—validation in 149 patients with two-year follow-up. Spine Deform 7(2):331–337. https://doi.org/10.1016/j.jspd.2018.08.002
Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstuck F, Perez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A, European Spine Study G (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99(19):1661–1672. https://doi.org/10.2106/JBJS.16.01594
Naresh-Babu J, Viswanadha A-K, Ito M, Park J-B (2019) What Should an ideal adult spinal deformity classification system consist of?: review of the factors affecting outcomes of adult spinal deformity management. Asian Spine J 13(4):694–703. https://doi.org/10.31616/asj.2018.0309
Buckland AJ, Vira S, Oren JH, Lafage R, Harris BY, Spiegel MA, Diebo BG, Liabaud B, Protopsaltis TS, Schwab FJ, Lafage V, Errico TJ, Bendo JA (2016) When is compensation for lumbar spinal stenosis a clinical sagittal plane deformity? Spine J 16(8):971–981. https://doi.org/10.1016/j.spinee.2016.03.047
Sarkar M, Goyal M, Samuel AJ (2020) Comparing the effectiveness of the muscle energy technique and kinesiotaping in mechanical sacroiliac joint dysfunction: a non-blinded, two-group, pretest-posttest randomized clinical trial protocol. Asian Spine J. https://doi.org/10.31616/asj.2019.0300
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kwon, BT., Kim, HJ., Yang, HJ. et al. Comparison of sacroiliac joint degeneration between patients with sagittal imbalance and lumbar spinal stenosis. Eur Spine J 29, 3038–3043 (2020). https://doi.org/10.1007/s00586-020-06558-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06558-6