Abstract
Background
Hip and spine pathology can alter the biomechanics of spino-pelvic mobility. Lumbar spine fusions can reduce the mobility of the lumbar spine and therefore result in compensatory femoral motion, contributing towards dislocations of THA.
Purpose
This meta-analysis aims to determine the effect of pre-existing spine fusions on THA outcomes, and complication profile including hip dislocations, all-cause revisions and all complications.
Methods
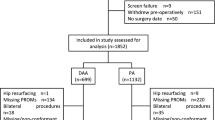
A multi-database search was performed according to PRISMA guidelines. All studies that compared patients who underwent THA with and without prior SF were included in the analysis.
Results
Ten studies were included in this review, consisting of 28,396 SF THA patients and 1,550,291 non-SF THA patients. There were statistically significant higher rates of hip dislocation (OR 2.20, 95% CI 1.71–2.85, p < 0.001), all-cause revision (OR 3.43, 95% CI 1.96–6.00, p < 0.001) and all complications (OR 2.83, 95% CI 1.28–6.24, p = 0.01) in SF than in non-SF THA patients. When registry data were excluded, these rates were approximately doubled. Subgroup analysis of revisions for dislocations was not statistically significant (OR 5.28, 95% CI 0.76–36.87, p = 0.09). While no meta-analysis was performed on clinical outcomes due to heterogeneous parameter reporting, individual studies reported significantly poorer outcomes in SF patients than in non-SF patients.
Conclusion
THA patients with SF are at higher risks of hip dislocations, all-cause revisions and all complications, which may adversely affect patient-reported outcomes. Surgeons should be aware of these risks and appropriately plan to account for altered spino-pelvic biomechanics, in order to reduce the risks of hip dislocations and other complications.
Level of evidence
II (Meta-analysis of non-homogeneous studies).
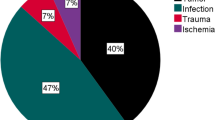
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.











Similar content being viewed by others
References
Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW (2016) What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res 474(2):386–391
An VVG, Phan K, Sivakumar BS, Mobbs RJ, Bruce WJ (2018) Prior lumbar spinal fusion is associated with an increased risk of dislocation and revision in total hip arthroplasty: a meta-analysis. J Arthroplasty 33(1):297–300
Archbold HA, Mockford B, Molloy D, McConway J, Ogonda L, Beverland D (2006) The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement: a preliminary study of 1000 cases investigating postoperative stability. J Bone Joint Surg Br 88(7):883–886
Barrey C, Darnis A (2015) Current strategies for the restoration of adequate lordosis during lumbar fusion. World J Orthop 6(1):117–126
Barry JJ, Sing DC, Vail TP, Hansen EN (2017) Early outcomes of primary total hip arthroplasty after prior lumbar spinal fusion. J Arthroplasty 32(2):470–474
Bedard NA, Martin CT, Slaven SE, Pugely AJ, Mendoza-Lattes SA, Callaghan JJ (2016) Abnormally high dislocation rates of total hip arthroplasty after spinal deformity surgery. J Arthroplasty 31(12):2884–2885
Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stockl B (2005) Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br 87(6):762–769
Bourne RB, Mehin R (2004) The dislocating hip: what to do, what to do. J Arthroplasty 19(4 Suppl 1):111–114
Buckland AJ, Puvanesarajah V, Vigdorchik J, Schwarzkopf R, Jain A, Klineberg EO et al (2017) Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Joint J 99-b(5):585–591
Button KS, Ioannidis JPA, Mokrysz C, Nosek BA, Flint J, Robinson ESJ et al (2013) Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci 14:365
Chen X, Xiong J, Wang P, Zhu S, Qi W, Peng H et al (2018) Robotic-assisted compared with conventional total hip arthroplasty: systematic review and meta-analysis. Postgrad Med J 94(1112):335
Dandachli W, Ul Islam S, Richards R, Hall-Craggs M, Witt J (2013) The influence of pelvic tilt on acetabular orientation and cover: a three-dimensional computerised tomography analysis. Hip Int 23(1):87–92
Dargel J, Oppermann J, Brüggemann G-P, Eysel P (2014) Dislocation following total hip replacement. Deutsch Arztebl Int 111(51–52):884–890
Dorr LD, Malik A, Dastane M, Wan Z (2009) Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res 467(1):119–127
Eneqvist T, Bulow E, Nemes S, Brisby H, Garellick G, Fritzell P et al (2018) Patients with a previous total hip replacement experience less reduction of back pain following lumbar back surgery. J Orthop Res 36(9):2484–2490
Fessy MH, Putman S, Viste A, Isida R, Ramdane N, Ferreira A et al (2017) What are the risk factors for dislocation in primary total hip arthroplasty? A multicenter case–control study of 128 unstable and 438 stable hips. Orthop Traumatol Surg Res 103(5):663–668
Gliklich RE, Dreyer NA, Leavy MB (2014) 201 Registries for evaluating patient outcomes: a user’s guide, chapter 13, 3rd edn. Agency for Healthcare Research and Quality (US), Rockville
Heckmann N, McKnight B, Stefl M, Trasolini NA, Ike H, Dorr LD (2018) Late dislocation following total hip arthroplasty: spinopelvic imbalance as a causative factor. J Bone Joint Surg Am 100(21):1845–1853
Hiddema WB, van der Merwe JF, van der Merwe W (2016) The transverse acetabular ligament as an intraoperative guide to cup abduction. J Arthroplasty 31(7):1609–1613
Ike H, Dorr LD, Trasolini N, Stefl M, McKnight B, Heckmann N (2018) Spine–pelvis–hip relationship in the functioning of a total hip replacement. JBJS 100(18):1606–1615
Kiran M, Johnston LR, Sripada S, McLeod GG, Jariwala AC (2018) Cemented total hip replacement in patients under 55 years. Acta Orthop 89(2):152–155
Koenig L, Zhang Q, Austin MS, Demiralp B, Fehring TK, Feng C et al (2016) Estimating the societal benefits of THA after accounting for work status and productivity: a Markov model approach. Clin Orthop Relat Res 474(12):2645–2654
Krushell R, Bhowmik-Stoker M, Kison C, O’Connor M, Cherian JJ, Mont MA (2016) Characterization of patient expectations and satisfaction after total hip arthroplasty. J Long Term Eff Med Implants 26(2):123–132
Lazennec J-Y, Brusson A, Rousseau M-A (2011) Hip–spine relations and sagittal balance clinical consequences. Eur Spine J 20(Suppl 5):686–698
Lazennec JY, Riwan A, Gravez F, Rousseau MA, Mora N, Gorin M et al (2007) Hip spine relationships: application to total hip arthroplasty. Hip Int 17(Suppl 5):S91–S104
Lazennec JY, Charlot N, Gorin M, Roger B, Arafati N, Bissery A et al (2004) Hip–spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat 26(2):136–144
Lazennec JY, Boyer P, Gorin M, Catonne Y, Rousseau MA (2011) Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop Relat Res 469(4):1103–1109
Lembeck B, Mueller O, Reize P, Wuelker N (2005) Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop 76(4):517–523
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60(2):217–220
Loh JLM, Jiang L, Chong HC, Yeo SJ, Lo NN (2017) Effect of spinal fusion surgery on total hip arthroplasty outcomes: a matched comparison study. J Arthroplasty 32(8):2457–2461
Lum ZC, Coury JG, Cohen JL, Dorr LD (2018) The current knowledge on spinopelvic mobility. J Arthroplasty 33(1):291–296
Malkani AL, Garber AT, Ong KL, Dimar JR, Baykal D, Glassman SD et al (2018) Total hip arthroplasty in patients with previous lumbar fusion surgery: are there more dislocations and revisions? J Arthroplasty 33(4):1189–1193
Mannion AF, Impellizzeri FM, Leunig M, Jeszenszy D, Becker HJ, Haschtmann D et al (2018) EUROSPINE 2017 FULL PAPER AWARD: time to remove our rose-tinted spectacles: a candid appraisal of the relative success of surgery in over 4500 patients with degenerative disorders of the lumbar spine, hip or knee. Eur Spine J 27(4):778–788
McLawhorn AS, Sculco PK, Weeks KD, Nam D, Mayman DJ (2016) Targeting a new safe zone: a step in the development of patient-specific component positioning for total hip arthroplasty. Am J Orthop (Belle Mead NJ) 44(6):270–276
Meek RM, Allan DB, McPhillips G, Kerr L, Howie CR (2006) Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res 447:9–18
Meek RM, Allan DB, McPhillips G, Kerr L, Howie CR (2008) Late dislocation after total hip arthroplasty. Clin Med Res 6(1):17–23
Meftah M, Yadav A, Wong AC, Ranawat AS, Ranawat CS (2013) A novel method for accurate and reproducible functional cup positioning in total hip arthroplasty. J Arthroplasty 28(7):1200–1205
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Noordin S, Lakdawala R, Masri BA (2012) Primary total hip arthroplasty: staying out of trouble intraoperatively. Ann Med Surg 2018(29):30–33
Palazzo C, Jourdan C, Descamps S, Nizard R, Hamadouche M, Anract P et al (2014) Determinants of satisfaction 1 year after total hip arthroplasty: the role of expectations fulfilment. BMC Musculoskelet Disord 15:53
Pearce CJ, Sexton SA, Davies DC, Khaleel A (2008) The transverse acetabular ligament may be used to align the acetabular cup in total hip arthroplasty. Hip Int 18(1):7–10
Perfetti DC, Schwarzkopf R, Buckland AJ, Paulino CB, Vigdorchik JM (2017) Prosthetic dislocation and revision after primary total hip arthroplasty in lumbar fusion patients: a propensity score matched-pair analysis. J Arthroplasty 32(5):1635–1640.e1631
Phan K, Nazareth A, Hussain AK, Dmytriw AA, Nambiar M, Nguyen D et al (2018) Relationship between sagittal balance and adjacent segment disease in surgical treatment of degenerative lumbar spine disease: meta-analysis and implications for choice of fusion technique. Eur Spine J 27(8):1981–1991
Pierrepont J, Stambouzou C, Miles B, O’Connor P, Ellis A, Molnar R et al (2016) Patient-specific component alignment in total hip arthroplasty. Reconstr Rev 6(4):7
Ranawat CS, Maynard MJ (1991) Modern technique of cemented total hip arthroplasty. Tech Orthop 6(3):17–25
Renner L, Janz V, Perka C, Wassilew GI (2016) What do we get from navigation in primary THA? EFORT Open Rev 1(5):205–210
Ryan JA, Jamali AA, Bargar WL (2010) Accuracy of computer navigation for acetabular component placement in THA. Clin Orthop Relat Res 468(1):169–177
Salib CG, Reina N, Perry KI, Taunton MJ, Berry DJ, Abdel MP (2019) Lumbar fusion involving the sacrum increases dislocation risk in primary total hip arthroplasty. Bone Joint J 101-b(2):198–206
Sing DC, Barry JJ, Aguilar TU, Theologis AA, Patterson JT, Tay BK et al (2016) Prior lumbar spinal arthrodesis increases risk of prosthetic-related complication in total hip arthroplasty. J Arthroplasty 31(9 Suppl):227–232.e221
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Spencer-Gardner L, Pierrepont J, Topham M, Bare J, McMahon S, Shimmin AJ (2016) Patient-specific instrumentation improves the accuracy of acetabular component placement in total hip arthroplasty. Bone Joint J 98-b(10):1342–1346
Stefl M, Lundergan W, Heckmann N, McKnight B, Ike H, Murgai R et al (2017) Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J 99-b(1 Supple A):37–45
van Stralen GM, Struben PJ, van Loon CJ (2003) The incidence of dislocation after primary total hip arthroplasty using posterior approach with posterior soft-tissue repair. Arch Orthop Trauma Surg 123(5):219–222
von Engelhardt LV, Breil-Wirth A, Kothny C, Seeger JB, Grasselli C, Jerosch J (2018) Long-term results of an anatomically implanted hip arthroplasty with a short stem prosthesis (MiniHip(TM)). World J Orthop 9(10):210–219
Waddell BS, Mohamed S, Glomset JT, Meyer MS (2016) A detailed review of hip reduction maneuvers: a focus on physician safety and introduction of the Waddell technique. Orthop Rev 8(1):6253
Weeden SH, Paprosky WG, Bowling JW (2003) The early dislocation rate in primary total hip arthroplasty following the posterior approach with posterior soft-tissue repair. J Arthroplasty 18(6):709–713
York PJ, McGee AW Jr, Dean CS, Hellwinkel JE, Kleck CJ, Dayton MR et al (2018) The relationship of pelvic incidence to post-operative total hip arthroplasty dislocation in patients with lumbar fusion. Int Orthop 42(10):2301–2306
Zahar A, Rastogi A, Kendoff D (2013) Dislocation after total hip arthroplasty. Curr Rev Musculoskelet Med 6(4):350–356
Author information
Authors and Affiliations
Contributions
JRO contributed to idea conception, literature search, data collection, statistics, manuscript writing and editing. MN contributed to idea conception, manuscript writing and editing. JO contributed to literature search, data collection, statistics, figures and tables, and manuscript writing. KP contributed to statistics, figures and manuscript writing. AA, SB and RH contributed to manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was primarily performed in Box Hill Hospital, Victoria, Australia.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Onggo, J.R., Nambiar, M., Onggo, J.D. et al. Clinical outcomes and complication profile of total hip arthroplasty after lumbar spine fusion: a meta-analysis and systematic review. Eur Spine J 29, 282–294 (2020). https://doi.org/10.1007/s00586-019-06201-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06201-z