Abstract
Purpose
To update evidence of diagnostic potential for identification of lumbar spinal stenosis (LSS) based on demographic and patient history, clinical findings, and physical tests, and report posttest probabilities associated with test findings.
Methods
An electronic search of PubMed, CINAHL and Embase was conducted combining terms related to low back pain, stenosis and diagnostic accuracy. Prospective or retrospective studies investigating diagnostic accuracy of LSS using patient history, clinical findings and/or physical tests were included. The risk of bias and applicability were assessed using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS 2) tool. Diagnostic accuracy including sensitivities (SN), specificities (SP), likelihood ratios (+LR and −LR) and posttest probabilities (+PTP and −PTP) with 95% confidence intervals were summarized.
Results
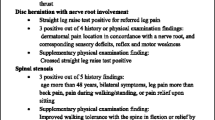
Nine studies were included (pooled n = 36,228 participants) investigating 49 different index tests (30 demographic and patient history and 19 clinical findings/physical tests). Of the nine studies included, only two exhibited a low risk of bias and seven exhibited good applicability according to QUADAS 2. The demographic and patient history measures (self-reported history questionnaire, no pain when seated, numbness of perineal region) and the clinical findings/physical tests (two-stage treadmill test, symptoms after a March test and abnormal Romberg test) highly improved positive posttest probability by > 25% to diagnose LSS.
Conclusion
Outside of one study that was able to completely rule out LSS with no functional neurological changes none of the stand-alone findings were strong enough to rule in or rule out LSS.
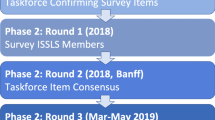
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.



Similar content being viewed by others
References
Katz JN, Harris MB (2008) Clinical practice. Lumbar spinal stenosis. N Engl J Med 358(8):818–825. https://doi.org/10.1056/nejmcp0708097
Kalichman L, Cole R, Kim DH, Li L, Suri P, Guermazi A, Hunter DJ (2009) Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J 9(7):545–550. https://doi.org/10.1016/j.spinee.2009.03.005
Singh K, Samartzis D, Vaccaro AR, Nassr A, Andersson GB, Yoon ST, Phillips FM, Goldberg EJ, An HS (2005) Congenital lumbar spinal stenosis: a prospective, control-matched, cohort radiographic analysis. Spine J 5(6):615–622. https://doi.org/10.1016/j.spinee.2005.05.385
De Villiers PD, Booysen EL (1976) Fibrous spinal stenosis. A report on 850 myelograms with a water-soluble contrast medium. Clin Orthop Relat Res 115:140–144
Roberson GH, Llewellyn HJ, Taveras JM (1973) The narrow lumbar spinal canal syndrome. Radiology 107(1):89–97. https://doi.org/10.1148/107.1.89
Fanuele JC, Birkmeyer NJ, Abdu WA, Tosteson TD, Weinstein JN (2000) The impact of spinal problems on the health status of patients: have we underestimated the effect? Spine (Phila Pa 1976) 25(12):1509–1514
de Graaf I, Prak A, Bierma-Zeinstra S, Thomas S, Peul W, Koes B (2006) Diagnosis of lumbar spinal stenosis: a systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976) 31(10):1168–1176. https://doi.org/10.1097/01.brs.0000216463.32136.7b
de Schepper EI, Overdevest GM, Suri P, Peul WC, Oei EH, Koes BW, Bierma-Zeinstra SM, Luijsterburg PA (2013) Diagnosis of lumbar spinal stenosis: an updated systematic review of the accuracy of diagnostic tests. Spine 38(8):E469–E481. https://doi.org/10.1097/brs.0b013e31828935ac
Whiting P, Rutjes AW, Dinnes J, Reitsma J, Bossuyt PM, Kleijnen J (2004) Development and validation of methods for assessing the quality of diagnostic accuracy studies. Health Technol Assess 8(25):1–234
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, Group Q (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
McInnes MDF, Moher D, Thombs BD, McGrath TA, Bossuyt PM, Clifford T, Cohen JF, Deeks JJ, Gatsonis C, Hooft L, Hunt HA, Hyde CJ, Korevaar DA, Leeflang MMG, Macaskill P, Reitsma JB, Rodin R, Rutjes AWS, Salameh JP, Stevens A, Takwoingi Y, Tonelli M, Weeks L, Whiting P, Willis BH (2018) Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA 319(4):388–396. https://doi.org/10.1001/jama.2017.19163
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. https://doi.org/10.1136/bmj.j4008
Bossuyt P, Leeflang M (2008) Chapter 6: developing criteria for including studies. Cochrane handbook for systematic reviews of diagnostic test accuracy version 04 [updated September 2008] The Cochrane Collaboration
Worster A, Carpenter C (2008) Incorporation bias in studies of diagnostic tests: how to avoid being biased about bias. Can J Emerg Med 10(2):174–175
Wayne J (2005) Mosby’s dicfionary of complementary & alternafive medicine. Mosby, St Louis
Harris P, Nagy S, Vardaxis N (2014) ) Mosby’s Dictionary of Medicine, Nursing and Health Professions-Australian & New Zealand Edition. Elsevier Health Sciences, Amsterdam
Bossuyt PM, Reitsma JB, Linnet K, Moons KG (2012) Beyond diagnostic accuracy: the clinical utility of diagnostic tests. Clin Chem 58(12):1636–1643. https://doi.org/10.1373/clinchem.2012.182576
Cook C, Hegedus EJ (2008) Orthopedic physical examination tests: an evidence-based approach. Prentice Hall, New York
Toolbox E-BM (2018) EBM calculators. https://ebm-tools.knowledgetranslation.net/calculator
Analysis wCT (2018) 2-way contingency table analysis. http://statpages.info/ctab/2x2.html
Calculation E (2018) Diagnostic post test probability of disease calculation. https://www.easycalculation.com/statistics/post-test-probability.php
Cook C, Brown C, Michael K, Isaacs R, Howes C, Richardson W, Roman M, Hegedus E (2011) The clinical value of a cluster of patient history and observational findings as a diagnostic support tool for lumbar spine stenosis. Physiother Res Int 16(3):170–178. https://doi.org/10.1002/pri.500
Dobbs R, May S, Hope P (2016) The validity of a clinical test for the diagnosis of lumbar spinal stenosis. Man Ther 25:27–34. https://doi.org/10.1016/j.math.2016.05.332
Fritz JM, Erhard RE, Delitto A, Welch WC, Nowakowski PE (1997) Preliminary results of the use of a two-stage treadmill test as a clinical diagnostic tool in the differential diagnosis of lumbar spinal stenosis. J Spinal Disord 10(5):410–416
Jensen OH, Schmidt-Olsen S (1989) A new functional test in the diagnostic evaluation of neurogenic intermittent claudication. Clin Rheumatol 8(3):363–367
Kato K, Sekiguchi M, Yonemoto K, Kakuma T, Nikaido T, Watanabe K, Otani K, Yabuki S, Kikuchi S, Konno S (2015) Diagnostic accuracy of the Self-administered, Self-reported History Questionnaire for lumbar spinal stenosis patients in Japanese primary care settings: a multicenter cross-sectional study (DISTO-project). J Orthop Sci 20(5):805–810. https://doi.org/10.1007/s00776-015-0740-6
Katz JN, Dalgas M, Stucki G, Katz NP, Bayley J, Fossel AH, Chang LC, Lipson SJ (1995) Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum 38(9):1236–1241
Konno S, Hayashino Y, Fukuhara S, Kikuchi S, Kaneda K, Seichi A, Chiba K, Satomi K, Nagata K, Kawai S (2007) Development of a clinical diagnosis support tool to identify patients with lumbar spinal stenosis. Eur Spine J 16(11):1951–1957. https://doi.org/10.1007/s00586-007-0402-2
Roach KE, Brown MD, Albin RD, Delaney KG, Lipprandi HM, Rangelli D (1997) The sensitivity and specificity of pain response to activity and position in categorizing patients with low back pain. Phys Ther 77(7):730–738
Sugioka T, Hayashino Y, Konno S, Kikuchi S, Fukuhara S (2008) Predictive value of self-reported patient information for the identification of lumbar spinal stenosis. Fam Pract 25(4):237–244. https://doi.org/10.1093/fampra/cmn031
Simel DL, Rennie D (2016) Low back pain, lumbar spinal stenosis. In: The rational clinical examination: evidence-based clinical diagnosis. McGraw-Hill Education, New York, NY,
O’Connell NE, Cook CE, Wand BM, Ward SP (2016) Clinical guidelines for low back pain: a critical review of consensus and inconsistencies across three major guidelines. Best Pract Res Clin Rheumatol 30(6):968–980. https://doi.org/10.1016/j.berh.2017.05.001
Rutjes AW, Reitsma JB, Di Nisio M, Smidt N, van Rijn JC, Bossuyt PM (2006) Evidence of bias and variation in diagnostic accuracy studies. CMAJ 174(4):469–476. https://doi.org/10.1503/cmaj.050090
Leeflang MM, Deeks JJ, Takwoingi Y, Macaskill P (2013) Cochrane diagnostic test accuracy reviews. Systematic reviews 2(1):82
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix 1: PRISMA-DTA checklist—based on blinded manuscript

Appendix 2: AMSTAR-2 checklist


Appendix 3
PubMed search strategy
-
1.
Population: low back pain
low back pain [ti/ab] OR lumbar paraspinal [ti/ab] OR pain [ti/ab] OR back-pain [ti/ab] OR back pain [ti/ab] OR backache [ti/ab] OR back ache [ti/ab] OR dorsalgia [ti/ab] OR lumbago [ti/ab] OR lumbar [ti/ab] OR lumbosacral [ti/ab] OR sciatic [ti/ab] OR radicular [ti/ab] OR lumbar vertebrae [ti/ab] OR spine [ti/ab] OR spinal [ti/ab]
- 2.
Target condition: lumbar spinal stenosis
Stenosis [ti/ab] OR stenosis [ti/ab] OR canal stenosis [ti/ab] OR lumbar spinal stenosis [ti/ab] OR spinal stenosis [ti/ab] OR spine stenosis [ti/ab] OR lss [ti/ab] OR claudication [ti/ab] OR claudicant [ti/ab] OR neurogen* [ti/ab] OR canal compression [ti/ab] OR canal compressing [ti/ab]
- 3.
Index test
Diagnostic [ti/ab] OR diagnosis [ti/ab]
- 4.
Methodological filter
sensitivity [ti/ab] OR specificity [ti/ab] OR sensitive test [ti/ab] OR specific test [ti/ab] OR screening [ti/ab] OR false positive [ti/ab] OR false negative [ti/ab] OR accuracy [ti/ab] OR predictive value [ti/ab] OR predictive values [ti/ab] OR reference value [ti/ab] OR reference values [ti/ab] OR reference standard [ti/ab] OR roc [ti/ab] OR likelihood [ti/ab]
Searches (combination): #1 AND #2 AND #3 AND 4
Embase search strategy
-
1.
Population and target condition: lumbar spinal stenosis
‘low back pain’:ta,ab OR ’back’:ab,ta OR ’backache’:ab,ta OR ’lumbar spine’:ta,ab OR ’lumbosacral spine’:ab,ta AND ‘stenosis’:ta,ab OR ’vertebral canal’:ta,ab OR ’vertebral canal stenosis’:ta,ab OR ’claudication’:ta,ab OR ’spinal cord compression’:ta,ab)
- 2.
Index test and methodological filter
(‘diagnosis’:ta,ab OR ’diagnostic procedure’:ta,ab) AND (‘sensitivity and specificity’:ta,ab OR ’screening’:ta,ab OR ’false positive result’:ta,ab OR ’false negative result’:ta,ab OR ’diagnostic accuracy’:ta,ab OR ’predictive value’:ta,ab OR ’reference value’:ta,ab OR ’standard’:ta,ab OR ’likelihood ratio’:ta,ab) AND [humans]/lim
Searches (combination): #1 AND #2
CINAHL search strategy
-
1.
Population and target condition: lumbar spinal stenosis
(low back pain OR back pain OR lumbar pain OR back OR backache OR back ache OR dorsalgia OR lumbago OR lumbar OR lumbosacral) AND (stenosis OR stenosis spinal OR canal stenosis OR spinal stenosis OR claudication OR claudicant)
- 2.
Index test and methodological filter
(diagnostic OR diagnosis) AND (sensitivity OR specificity OR specificity and sensitivity OR screening OR false positive OR false negative OR accuracy OR predictive value OR reference values OR reference standards OR likelihood ratio)
Searches (combination): #1 AND #2
Appendix 4: List of excluded studies/reasons for exclusion
-
1.
Adachi S, Nakano A, Kin A, Baba I, Kurokawa Y, Neo M (2018) The tibial nerve compression test for the diagnosis of lumbar spinal canal stenosis—a simple and reliable physical examination for use by primary care physicians. Acta Orthop Traumatol Turc 52(1):12–16. https://doi.org/10.1016/j.aott.2017.04.007
Reason for exclusion: Included patients were pre-diagnosed with LSS.
- 2.
Aizawa T, Tanaka Y, Yokoyama T, Shimada Y, Yamazaki K, Takei H, Konno S, Kawahara C, Itoi E, Kokubun S (2016) New diagnostic support tool for patients with leg symptoms caused by lumbar spinal stenosis and lumbar intervertebral disc herniation: a self-administered, self-reported history questionnaire. J Orthop Sci 21(5):579–585. https://doi.org/10.1016/j.jos.2016.07.012
Reason for exclusion: Included patients were pre-diagnosed with LSS.
- 3.
Ando M, Tamaki T, Kawakami M, Minamide A, Nakagawa Y, Maio K, Enyo Y, Yoshida M (2013) Electrophysiological diagnosis using sensory nerve action potential for the intraforaminal and extraforaminal L5 nerve root entrapment. Eur Spine J 22(4):833–839. https://doi.org/10.1007/s00586-012-2592-5
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
- 4.
Annunziata, CC, Lauerman, WC (1999). When back surgery fails: what’s the next step? Diagnostic findings must be interpreted within the clinical context. J. Musculosk Medicine
Reason for exclusion: Other study designs.
- 5.
Arce D, Sass P, Abul-Khoudoud H (2001). Recognizing spinal cord emergencies. Am Fam Physician
Reason for exclusion: Other study designs.
- 6.
Barz T, Staub LP, Melloh M, Hamann G, Lord SJ, Chatfield MD, Bossuyt PM, Lange J, Merk HR (2014) Clinical validity of the nerve root sedimentation sign in patients with suspected lumbar spinal stenosis. Spine J 14(4):667–674. https://doi.org/10.1016/j.spinee.2013.06.105
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
- 7.
Bosscher HA, Heavner JE (2012) Diagnosis of the vertebral level from which low back or leg pain originates. A comparison of clinical evaluation, MRI and epiduroscopy. Pain Pract 12(7):506–512. https://doi.org/10.1111/j.1533-2500.2012.00549.x
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
- 8.
Chien JJ, Bajwa ZH (2008). What is mechanical back pain and how best to treat it? Curr Pain Headache Rep
Reason for exclusion: Other study designs.
- 9.
Dvonch V, Scarff T, Bunch WH, Smith D, Boscardin J, Lebarge H, Ibrahim K (1984) Dermatomal somatosensory evoked potentials: their use in lumbar radiculopathy. Spine (Phila Pa 1976) 9(3):291–293
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
- 10.
Esmailiejah AA, Abbasian M, Bidar R, Esmailiejah N, Safdari F, Amirjamshidi A (2018) Diagnostic efficacy of clinical tests for lumbar spinal instability. Surg Neurol Int 9:17. https://doi.org/10.4103/sni.sni_359_17
Reason for exclusion: Included patients were pre-diagnosed with LSS.
- 11.
Faciszewski T, Broste SK, Fardon D (1997) Quality of data regarding diagnoses of spinal disorders in administrative databases. A multicenter study. J Bone Joint Surg Am 79(10):1481–1488
Reason for exclusion: Included other causes of LBP.
- 12.
Genevay S, Courvoisier DS, Konstantinou K, Kovacs FM, Marty M, Rainville J, Norberg M, Kaux JF, Cha TD, Katz JN, Atlas SJ (2018) Clinical classification criteria for neurogenic claudication caused by lumbar spinal stenosis. The N-CLASS criteria. Spine J 18(6):941–947. https://doi.org/10.1016/j.spinee.2017.10.003
Reason for exclusion: Included patients were pre-diagnosed with LSS.
- 13.
Haig AJ, Tong HC, Yamakawa KS, Quint DJ, Hoff JT, Chiodo A, Miner JA, Choksi VR, Geisser ME (2005) The sensitivity and specificity of electrodiagnostic testing for the clinical syndrome of lumbar spinal stenosis. Spine (Phila Pa 1976) 30(23):2667–2676
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
- 14.
Hayashi H, Toribatake Y, Murakami H, Yoneyama T, Watanabe T, Tsuchiya H (2015) Gait analysis using a support vector machine for lumbar spinal stenosis. Orthopedics 38(11):e959–e964. https://doi.org/10.3928/01477447-20151020-02
Reason for exclusion: Included healthy volunteers.
- 15.
Kato Y, Kawakami T, Kifune M, Kishimoto T, Nibu K, Oda H, Shirasawa K, Tominaga T, Toyoda K, Tsue K, Taguchi T (2009) Validation study of a clinical diagnosis support tool for lumbar spinal stenosis. J Orthop Sci 14(6):711–718. https://doi.org/10.1007/s00776-009-1391-2
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
- 16.
Konno S, Kikuchi S, Tanaka Y, Yamazaki K, Shimada Y, Takei H, Yokoyama T, Okada M, Kokubun S (2007) A diagnostic support tool for lumbar spinal stenosis: a self-administered, self-reported history questionnaire. BMC Musculoskelet Disord 8:102. https://doi.org/10.1186/1471-2474-8-102
Reason for exclusion: Included other causes of LBP.
- 17.
Laslett M, McDonald B, Tropp H, Aprill CN, Oberg B (2005) Agreement between diagnoses reached by clinical examination and available reference standards: a prospective study of 216 patients with lumbopelvic pain. BMC Musculoskelet Disord 6:28. https://doi.org/10.1186/1471-2474-6-28
Reason for exclusion: Included other causes of LBP.
- 18.
Lee JH, Lee SH (2012) Physical examination, magnetic resonance imaging, and electrodiagnostic study of patients with lumbosacral disc herniation or spinal stenosis. Journal of Rehabilitation Medicine 44(10):845–850
Reason for exclusion: Included other causes of LBP.
- 19.
Leng GC, Fowkes FG (1992) The Edinburgh Claudication Questionnaire: an improved version of the WHO/Rose Questionnaire for use in epidemiological surveys. J Clin Epidemiol 45(10):1101–1109
Reason for exclusion: Included other causes of LBP.
- 20.
Lin JH, Hsieh YC, Chen YC, Wang Y, Chen CC, Chiang YH (2017) Diagnostic accuracy of standardised qualitative sensory test in the detection of lumbar lateral stenosis involving the L5 nerve root. Sci Rep 7(1):10598. https://doi.org/10.1038/s41598-017-10641-2
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
- 21.
Mann NH, 3rd, Brown MD, Enger I (1992) Expert performance in low-back disorder recognition using patient pain drawings. J Spinal Disord 5(3):254–259
Reason for exclusion: Included other causes of LBP.
- 22.
Martin BI, Lurie JD, Tosteson AN, Deyo RA, Tosteson TD, Weinstein JN, Mirza SK (2014) Indications for spine surgery: validation of an administrative coding algorithm to classify degenerative diagnoses. Spine (Phila Pa 1976) 39(9):769–779. https://doi.org/10.1097/brs.0000000000000275
Reason for exclusion: Other study designs.
- 23.
Nayeb Aghaei H, Azimi P, Shahzadi S, Azhari S, Mohammadi HR (2015) Role of the Self-Administered, Self-Reported History Questionnaire to identify types of Lumbar spinal stenosis: a sensitivity analysis. Asian Spine J 9(5):689–693. https://doi.org/10.4184/asj.2015.9.5.689
Reason for exclusion: Other study designs.
- 24.
Ohtori S, Sekiguchi M, Yonemoto K, Kakuma T, Takahashi K, Konno S (2014) Awareness and use of diagnostic support tools for lumbar spinal stenosis in Japan. J Orthop Sci 19(3):412–417. https://doi.org/10.1007/s00776-014-0551-1
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
- 25.
Papadakis NC, Christakis DG, Tzagarakis GN, Chlouverakis GI, Kampanis NA, Stergiopoulos KN, Katonis PG (2009) Gait variability measurements in lumbar spinal stenosis patients: part A. Comparison with healthy subjects. Physiol Meas 30(11):1171–1186. https://doi.org/10.1088/0967-3334/30/11/003
Reason for exclusion: Included healthy volunteers.
- 26.
Shevelev IN, Konovalov NA, Cherkashov AM, Molodchenkov AA, Sharamko TG, Asiutin DS, Nazarenko AG (2013) [Virtual clinical diagnosis support system of degenerative stenosis of the lumbar spinal canal]. Zh Vopr Neirokhir Im N N Burdenko 77(5):38–43; discussion 43
Reason for exclusion: Other study designs.
- 27.
Thomas SA (2003). Spinal stenosis: history and physical examination. Phys Med Rehabil Clin N Am
Reason for exclusion: Other study designs.
- 28.
Tomkins-Lane CC, Quint DJ, Gabriel S, Melloh M, Haig AJ (2013) Nerve root sedimentation sign for the diagnosis of lumbar spinal stenosis: reliability, sensitivity, and specificity. Spine (Phila Pa 1976) 38(24):E1554–E1560. https://doi.org/10.1097/brs.0b013e3182a8c2da
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
- 29.
Yamada H, Oka H, Iwasaki H, Endo T, Kioka M, Ishimoto Y, Nagata K, Takiguchi N, Hashizume H, Minamide A, Nakagawa Y, Kawai M, Tsutsui S, Yoshida M (2015) Development of a support tool for the clinical diagnosis of symptomatic lumbar intra- and/or extra-foraminal stenosis. J Orthop Sci 20(5):811–817. https://doi.org/10.1007/s00776-015-0743-3
Reason for exclusion: Other study designs.
- 30.
Zhang L, Chen R, Liu B, Zhang W, Zhu Y, Rong L (2017) The nerve root sedimentation sign for differential diagnosis of lumbar spinal stenosis: a retrospective, consecutive cohort study. Eur Spine J 26(10):2512–2519. https://doi.org/10.1007/s00586-016-4435-2
Reason for exclusion: Included diagnostic accuracy of tests not related to the scope of this review.
Rights and permissions
About this article
Cite this article
Cook, C.J., Cook, C.E., Reiman, M.P. et al. Systematic review of diagnostic accuracy of patient history, clinical findings, and physical tests in the diagnosis of lumbar spinal stenosis. Eur Spine J 29, 93–112 (2020). https://doi.org/10.1007/s00586-019-06048-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06048-4