Abstract
Purpose
Intervertebral kinematic assessments have been used to investigate mechanical causes when back pain is resistant to treatment, and recent studies have identified intervertebral motion markers that discriminate patients from controls. However, such patients are a heterogeneous group, some of whom have structural disruption, but the effects of this on intervertebral kinematics are unknown.
Methods
Thirty-seven patients with treatment-resistant back pain referred for quantitative fluoroscopy were matched to an equal number of pain-free controls for age and sex. All received passive recumbent flexion assessments for intervertebral motion sharing inequality (MSI), variability (MSV), laxity and translation. Comparisons were made between patient subgroups, between patients and controls and against normative levels from a separate group of controls.
Results
Eleven patients had had surgical or interventional procedures, and ten had spondylolisthesis or pars defects. Sixteen had no disruption. Patients had significantly higher median MSI values (0.30) than controls (0.27, p = 0.010), but not MSV (patients 0.08 vs controls 0.08, p = 0.791). Patients who received invasive procedures had higher median MSI values (0.37) than those with bony defects (0.30, p = 0.018) or no disruption (0.28, p = 0.0007). Laxity and translation above reference limits were not more prevalent in patients.
Conclusion
Patients with treatment-resistant nonspecific back pain have greater MSI values than controls, especially if the former have received spinal surgery. However, excessive laxity, translation and MSV are not more prevalent in these patients. Thus, MSI should be investigated as a pain mechanism and for its possible value as a prognostic factor and/or target for treatment in larger patient populations.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Background
Nonspecific low back pain that persists and is unresponsive to treatment (CNSLBP) constitutes the largest part of the health and socioeconomic impact of this problem [1]. However, risk-based subgroupings give little insight into how individual cases should be managed when treatment has failed [2]. While important advances have been made in explaining the mechanisms involved in central pain modulation in CNSLBP patients, there have been few in relation to the biomechanical factors driving peripheral pain stimuli [3]. Thus, health professionals often have difficulty in identifying the biological mechanisms in CNSLBP and as a result may rely overly on psychosocial management [3, 4].
As most back pain has come to be regarded as mechanical and related to function, back motion studies have been central in the search for functional biomarkers [5,6,7,8,9]. Here, intervertebral motion data provide more intrinsic information than surface studies and data from fluoroscopic sequences have been found to differentiate groups of patients with chronic nonspecific low back pain (CNSLBP) from healthy controls by virtue of the patterns of segmental motion [10, 11]. Discriminating variables have been identified as intervertebral laxity (measured as the rate of displacement of a vertebra from its neutral position) and the motion sharing inequality and variability during passive flexion (MSI and MSV) [10,11,12].
Laxity denotes a loss of restraint in the mid-range [13]. It is an indicator of increased neutral zone length and may or may not be accompanied by increased range of intervertebral motion [14]. Motion sharing inequality (MSI) means an increased average difference between the segment that accepts the least proportion of the motion during the bending sequence and that which accepts the most [11]. This may be caused by stiffness at one or more levels, with or without hypermobility and/or mid-range laxity at others. Motion sharing variability (MSV), on the other hand, refers to erratic motion of individual vertebrae during the sequence [11]. (The numerical derivations of MSI and MSV are described in “Methods” and Supplementary material.) Recent studies using MSI and MSV [11] have tended to support relationships between CNSLBP and the integrated dynamic function of spinal motion segments hypothesised in the 1990s [13, 15]. Sagittal translation (or sliding as opposed to tilting motion) is typically also measured when instability is suspected—especially in patients with spondylolisthesis, but there is little evidence that it plays a role in CNSLBP [16].
Studies that measure multi-segmental continuous motion distribution in vivo are rare, it being traditional to measure motion individually at single levels quasi-statically, either using finite element (FE) modelling or laboratory specimens [17, 18]. However, in vivo individualised, dynamic, multi-segmental studies are needed for the clinical validation of both laboratory and FE modelling outputs and to investigate relationships between spinal mechanics and clinical outcomes [19,20,21].
Although intervertebral laxity and motion co-ordination have been investigated in CNSLBP, they have never been measured in treatment-resistant populations whose back pain is thought to be substantially mechanical in nature, yet this is where such investigations are more likely to be requested. A recent study found that lumbar intervertebral motion sharing (L2–S1) was correlated with the overall degree of disc degeneration in patients with CNSLBP, but not in controls [11]. However, patients with structural defects such as spondylolisthesis, or a history of invasive therapeutic procedures, such as surgery, were excluded from these studies. As patients with treatment-resistant back pain are probably more likely to have received surgical or other invasive interventions, it is necessary to assess the intervertebral kinematics in this population.
The aim of the present study was to investigate the degree of intervertebral laxity, MSI, MSV and sagittal translation during passive recumbent lumbar flexion and return motion in the lumbar spines of CNSLBP patients whose pain had failed to respond to treatment. Patients who had bony defects, invasive treatments and conservative care were included in the study. The main hypothesis was that these patients would have greater evidence of aberrant lumbar motion than pain-free healthy controls and that patients with bony disruption or a history of spinal surgery would have greater intervertebral motion dysfunction than those without.
Methods
Participants The referral forms and imaging reports of 86 patients who had been referred for quantitative fluoroscopy investigations to investigate intervertebral motion in treatment-resistant chronic, nonspecific low back pain between 2010 and 2017 were interrogated. A standardised image acquisition protocol was used throughout this period [22]. In order to compare results with previous studies that investigated differences in MSI and MSV between patients with CNSLBP and controls, only those patients who received passive recumbent flexion and return fluoroscopy examinations were included [10, 11] (Fig. 1). These were matched for age and sex to an equal number of healthy volunteer participants who had the same imaging investigations. Patients had to have been referred to investigate treatment-resistant back pain of longer than 3-month duration as specified by the referrer. Patients whose back pain was associated with nerve compression or serious spinal pathology were excluded. Controls had to have been free of any back pain that limited their normal activity for more than 1 day in the previous year. All participants had to have a BMI of less than 30, be aged between 18 and 70 years, have had no medical radiation exposure of > 8 mSV in the previous 2 years, no pregnancy (females) and have given informed consent. The study was carried out following a favourable ethical opinion (National Research Ethics Service South West 3, REC reference 10/H0106/65).
Data collection Patient age and sex, duration of complaint, the main intervention and any record of disruption, either anatomical or as a result of an invasive therapeutic procedure, were extracted from the referral forms. Intervertebral kinematic data were retrieved from patient records and re-analysed to measure laxity, MSI, MSV and translation against matched controls.
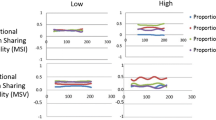
Laxity was measured as the ratio of the slopes of trunk motion to intervertebral motion in the initial 10o of movement from the start position [23]. MSI was the average filtered proportional range contribution to the motion across all points in each sequence and MSV the square root of the variance of these distances [11] (Fig. 2). A graphical illustration of high and low MSI and MSV is shown in Fig. 3. (For details of these variables and methodology, please see Supplementary material.) Translation was measured using the method of Frobin et al. [24] as the maximum change in position relative to the vertebra below in vertebral body units, which were then converted to millimetres using a standard vertebral body depth of 35 mm [25].
Derivation of MSI and MSV. Example of the measurement of continuous proportional intervertebral range of motion (flexion). The range was calculated for each data point on the x-axis (black lines). Motion share inequality (MSI) was calculated as the mean of all the ranges in the sequence and motion share variability (MSV) was their RMS value (see also “Appendix”)
Data analysis Kinematic variables were compared between patients and controls for all patients and then between subsets who had invasive procedures and bony defects (i.e. pars defects and/or spondylolisthesis). The prevalence of patient variables exceeding the upper reference range of each variable (mean + 1.96 SD) was determined by comparing each patient value with that derived from a separate cohort of healthy pain-free controls (n = 54) who had been imaged using the same protocol. The study primarily tested the one-tailed hypothesis that MSI and MSV would be higher in patients. It also compared laxity and translation at individual levels from L2–S1 as a two-tailed hypothesis.
Statistical analysis Prior to analysis, all continuous data were tested for normality using the Shapiro–Wilk test. As most variables were not normally distributed, one- and two-sided differences were tested with unpaired Mann–Whitney tests and correlations with Spearman’s rho. The significance of proportions of patient data that exceeded the upper reference range was determined using one- and two-sided Fisher’s exact tests.
Results
Thirty-seven patients (females 14 and males 23) who met the entry criteria were identified and matched for age [mean (SD); patients 47.5 (10.87), controls 49.0 (10.88) p = 0.940] and sex to an equal number of healthy volunteer participants. The durations of their conditions, main interventions and main types of structural disruption are given in Table 1. Most patients had received conservative therapies, but 12 had received spinal surgery or other interventional procedures. Six had a spondylolisthesis and four had pars defects with no slip. One patient had both a pars defect without slip and had received prolotherapy. This patient was analysed as having had an interventional procedure.
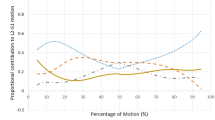
MSI and MSV Median MSI was significantly greater in patients (0.30) than in controls (0.27, p = 0.010), as well as in the subset that had invasive treatments (p = 0.016) (Table 2). It was also higher in the subsets with bony defects and those with intact segments and no disruption, but these did not reach significance. This supports the hypothesis that patients have greater evidence of aberrant lumbar motion than healthy controls. MSI was also significantly higher in patients who had had invasive interventions (0.37) than in those who only had pars defects or spondylolistheses (0.30, p = 0.005) and those with no structural change (0.28, p = 0.013). As spinal fusion targets intervertebral motion at specific segments, it is perhaps not surprising that the sharing of motion by the lumbar segments would be affected by it. By contrast, there was no significant difference in MSI between patients with bony defects and no structural change (p = 0.612) (Fig. 4).
Three patients had MSI levels that were higher than the upper reference range (0.50) as opposed to none in controls (p = 0.060, two-sided Fisher’s exact) (Table 3). All three had undergone complex spinal surgery (disc replacement, resected fusion, discectomy). By contrast, patients with pars defects and spondylolistheses ranged towards lower MSI values which were nonsignificantly higher than controls (Table 1 and Fig. 5). This suggests that excessively unequal motion sharing is more prevalent in patients who have undergone spinal surgery and remain in pain. MSI was not related to the duration of the complaint (rho = − 0.07, p = 0.672) in patients, or to age in both patients (rho = − 0.10, p = 0.0.552) and controls (rho = 0.12, p = 0.491).
Median MSV, although having a trend towards being higher in the subgroup that received invasive treatments, was not significantly so (Table 2). This is consistent with previous studies of passive flexion, which found that only when combining passive left, right flexion and extension motion, did CNSLBP patients have significantly higher MSV levels [10, 11]. In the present studies, median MSV was also not significantly higher in patients who had invasive treatments (0.09) than those with bony abnormalities (0.08) (p = 0.230) and was not correlated with age (Rho = 0.39, p = 0.644) or complaint duration (Rho = − 0.20, p = 0.244). Furthermore, an equal number of patients and controls (3) had MSVs that exceeded the reference limits (Table 3). This suggests that motion sharing variability (MSV) in passive flexion motion is a weaker dynamic biomechanical construct for discrimination between patients and controls than motion sharing inequality (MSI).
Laxity Laxity tended to be higher in controls than in patients for levels L3–S!, but this did not reach significance (Table 4). Laxity exceeded its reference range in 13/139 levels in ten patients and 12/139 levels for 12 controls (one-sided Fisher’s exact, p = 0.838) (Table 3). Five of these patients had had an invasive procedure, two had bony defects, one had both and four had neither. Laxity was also not more frequent in operated patients (5/10) or those with bony defects (2/10) than in matched controls (4/10). It was also not significantly higher in controls than in patients (Table 4). Thus, laxity, a variable denoting reduction in restraint and suggesting disco-ligamentous sub-failure, did not appear to be a marker in CNSLBP.
Translation Sagittal translation was included in this study as a variable preferred by many for the investigation of spine stability [16]. The results are given in Table 4. Significantly higher values were found in controls than in patients at L3–4 (p = 0.011) and L4–5 (p = 0.020). However, levels that exceeded their reference ranges were not significantly more prevalent in controls (12 vs 2, two-sided Fisher’s exact, p = 0.124) (Table 3). This supports the impression that treatment-resistant nonspecific back pain is more often associated with stiffness than loss of restraint, and excessive translation appears to be infrequent in such patient populations.
Discussion
The hypothesis that passive recumbent MSI would be greater in these patients than in controls was supported, as was the hypothesis that patients who had received surgery would have higher values for this than those who had not. This tends both to confirm previous studies that found passive recumbent MSI to be a biomarker for CNSLBP [11] and to suggest a link to spinal stabilisation surgery. However, the degree of difference was no greater than in previous studies in populations that excluded patients who had body defects and invasive procedures [10, 11]. In the present study, there were also significantly higher MSI values in patients who had invasive procedures than in those with bony defects (p = 0.005), while MSIs in patients with bony defects were not significantly different from those with no disruption (p = 0.612) (Fig. 4). Structural change (e.g. due to injury, degeneration and/or invasive treatments), pain and MSI therefore seem to be linked, although the mechanism by which this happens is unclear. Intuitively, it may be related to combinations of microstrain, muscle fatigue and/or metabolite build-up, which might also help to explain the pain relief felt by some patients following spinal manipulation and mobilisation, which may increase the mobility of restricted segments, more evenly distributing their contributions to the motion and improving blood flow [26, 27].
We did not study weight-bearing motion, where previous studies found strong correlations between MSV and disc degeneration, as well as between MSI and MSV, but only weak associations with CNSLBP [11]. However, such weight-bearing studies have found associations between laxity and CNSLBP [12]. In the present studies, conducted with participants in passive recumbent motion, there was a trend for MSV to be higher in patients who had had invasive treatments than in controls (Table 2). This suggests that MSV may be associated with intervertebral disc disruption if this is sufficiently severe. The fact that these correlations were present in weight-bearing motion in other studies suggests that these associations may be mediated by motor control and/or loading [11]. This could be explored by concurrently acquiring electromyography data in low back pain patients [28]. On the other hand, while the reliability of the measurement of translation, laxity and MSI in this configuration has been found to be acceptable, MSV changes over time in the individual were not, making it potentially less useful as a measure [23, 25, 29]. However, MSV may be helpful in investigating the therapeutic actions of motor control and strengthening exercises at an intervertebral level [30,31,32,33,34].
Laxity, on the other hand, is a surrogate indicator of neutral zone length and therefore of disco-ligamentous sub-failure [14, 35]. When present in patients whose back pain is thought mechanical, it could be considered a contraindication to manipulation and an indication for stabilisation. The passive recumbent motion configuration would seem to be suitable for future clinical studies of the relationships of such factors to pain and disability and their outcomes. However, the results for both laxity and translation in the present cohort suggest that their roles may be more amenable to the identification of subgroups of patients whose pain is associated with loss of restraint. Laxity may also be a useful biomechanical measure for the investigation of adjacent segment disease (ASD), for which biomechanical changes are thought to be responsible, and for adding to the understanding the biomechanical effects of dynamic stabilisation systems and their clinical validation [36,37,38].
In summary, what this means for the clinician is that these investigations have explanatory value for such patients, indicating whether abnormal biomechanics is part of the clinical picture, whether there are motion segments with reduced restraint and whether consideration should be given to surgical stabilisation in selected cases. However, although a number of academic units have performed research studies with similar technologies, there are few clinical services outside of North America that offer them.
Limitations The main limitations of this study were its retrospective nature and small patient population. However, patient referral for QF was justified by the need for better diagnostic information to inform treatment: a legal requirement under the Ionising Radiation (medical exposure) Regulations [39], and the criterion of treatment-resistant back pain was assured through discussion at the point of referral.
Future work Clinical studies are needed to improve our understanding of the role of these markers and in patient outcomes, for example, in surgical populations. Kinematic and clinical profiles could be compared and scrutinised for associations in key patient groups (e.g. occupational back pain), and baseline examinations could be studied for relationships between these kinematic variables and prognosis [40]. At a measurement level, weight-bearing studies that combine kinematic and MRI-generated individualised FE model data to provide stress loading information during motion have begun and should be progressed [41]. Further work is also needed to investigate the relationships between disc degeneration, symptoms and these biomechanical factors as is further replication of this work in prospective studies [42, 43].
Conclusion
Mechanical factors appear to be prominent in treatment-resistant back pain. In this study, motion sharing inequality (MSI) was greater in such patients, especially if they had undergone spinal surgery. Laxity was not more prevalent in patients than controls including post-surgery. This might suggest that MSI is associated with pain from muscle fatigue and metabolite build-up, whereas laxity that reflects pain from diminished restraint due to true disco-ligamentous sub-failure is unusual in this population [35]. Further clinical studies are needed to investigate these theories.
References
C.S.A.G. (1994) Epidemiology review: the epidemiology and cost of back pain. In: Department of health, London
Saragiotto BT, Maher CG, Hancock MJ, Koes BW (2017) Subgrouping patients with nonspecific low back pain: Hope or Hype? J Orthop Sports Phys Ther 47:44–48
Hancock MJ, Maher CG, Laslett M, Hay E, Koes B (2011) Discussion paper: what happened to the ‘bio’ in the bio-psycho-social model of low back pain? Eur Spine J 20:2105–2110
Deane JA, McGregor AH (2016) Current and future perspectives on lumbar degenerative disc disease: a UK survey exploring specialist multidisciplinary clinical opinion. BMJ Open 2017:e011075. https://doi.org/10.1136/bmjopen-2016011075
Hemming R, Sheeran L, van Deursen R, Martin RW, Sparkes V (2015) Regional spinal kinematics during static postures and functional tasks in people with non-specific chronic low back pain. Int J Ther Rehabil 22:S8
Tsang SMH, Szeto GPY, Li LMK, Wong DCM, Yip MMP, Lee RYW (2017) The effects of bending speed on the lumbo-pelvic kinematics and movement pattern during forward bending in people with and without low back pain. BMC Musculoskelet Disord 18:157
Mieritz RM, Hartvigsen J, Boyle E, Jakobsen MD, Aagaard P, Bronfort G (2014) Lumbar motion changes in chronic low back pain patients: a secondary analysis of data from a randomized clinical trial. Spine J 14:2618–2627
Borenstein D (2013) Mechanical low back pain—a rheumatologist’s view. Nat Rev Rheumatol 9:643–653
Barz T, Melloh M, Lord SJ, Kasch R, Merk HR, Staub LP (2014) A conceptual model of compensation/decompensation in lumbar segmental instability. Med Hypotheses 83:312–316
Mellor FE, Thomas P, Thompson P, Breen AC (2014) Proportional lumbar spine inter-vertebral motion patterns: a comparison of patients with chronic non-specific low back pain and healthy controls. Eur Spine J 23:2059–2067. https://doi.org/10.1007/s00586-014-3273-3
Breen A, Breen A (2018) Uneven intervertebral motion sharing is related to disc degeneration and is greater in patients with chronic, non-specific low back pain: an in vivo, cross-sectional cohort comparison of intervertebral dynamics using quantitative fluoroscopy. Eur Spine J 27:145–153. https://doi.org/10.1007/s00586-017-5155-y
Teyhen DS, Flynn TW, Childs JD, Kuklo TR, Rosner MK, Polly DW, Abraham LD (2007) Fluoroscopic video to identify aberrant lumbar motion. Spine 32:E220–E229
Panjabi MM (1992) The stabilising system of the spine—part 2: neutral zone and instability hypothesis. J Spinal Disord 5:390–397
Breen AC, Dupac M, Osborne N (2015) Attainment rate as a surrogate indicator of the intervertebral neutral zone length in lateral bending: an in vitro proof of concept study. Chiropr Manual Ther 23:28. https://doi.org/10.1186/s12998-015-0073-8
Kanayama M, Abumi K, Kaneda K, Tadano S, Ukai T (1996) Phase lag of the intersegmental motion in flexion-extension of the lumbar and lumbosacral spine: an in vivo study. Spine 21:1416–1422
Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L (2007) Lumbar intervertebral instability: a review. Radiology 245:62–77
Zander T, Rohlmann A, Klockner C, Bergmann G (2002) Comparison of the mechanical behavior of the lumbar spine following mono- and bisegmental stabilization. Clin Biomech 17:439–445
Kettler A, Rohlmann F, Ring C, Mack C, Wilke HJ (2011) Do early stages of lumbar intervertebral disc degeneration really cause instability? Evaluation of an in vitro database. Eur Spine J 20:578–584
Oxland TR (2016) Fundamental biomechanics of the spine—what we have learned in the past 25 years and future directions. J Biomech 49:817–832
Jones AC, Wilcox RK (2008) Finite element analysis of the spine: towards a framework of verification, validation and sensitivity analysis. Med Eng Phys 30:1287–1304
Crisco JJ, Fujita L, Spenciner DB (2007) The dynamic flexion/extension properties of the lumbar spine in vitro using a novel pendulum system. J Biomech 40:2767–2773
Breen AC, Teyhen DS, Mellor FE, Breen AC, Wong K, Deitz A (2012) Measurement of inter-vertebral motion using quantitative fluoroscopy: report of an international forum and proposal for use in the assessment of degenerative disc disease in the lumbar spine. Adv Orthop. https://doi.org/10.1155/2012/802350
du Rose A, Breen A (2016) Relationships between lumbar inter-vertebral motion and lordosis in healthy adult males: a cross sectional cohort study. BMC Musculoskelet Disord 17:121
Frobin W, Brinckmann P, Biggemann M, Tillotson M, Burton K (1997) Precision measurement of disc height, vertebral height and sagittal plane displacement from lateral radiographic views of the lumbar spine. Clin Biomech 12:S22–S30
Breen A, Breen A (2016) Accuracy and repeatability of quantitative fluoroscopy for the measurement of sagittal plane translation and instantaneous axis of rotation in the lumbar spine. Med Eng Phys 38:607–614
Edgecombe TL, Kawchuk GN, Long CR, Pickar JG (2015) The effect of application site of spinal manipulative therapy (SMT) on spinal stiffness. Spine J 15:1332–1338
Rosendal L, Blangsted AK, Kristiansen J, Sogaard K, Langberg H, Sjogaard G, Kjaer M (2004) Interstitial muscle lactate, pyruvate and potassium dynamics in the trapezius muscle during repetitive low-force arm movements, measured with microdialysis. Acta Physiol Scand 182:379–388
du Rose A, Breen A (2016) Relationships between paraspinal muscle activity and lumbar inter-vertebral range of motion. Healthcare. https://doi.org/10.3390/healthcare4010004
Breen AC, Breen AC (2017) Intra subject repeatability of intervertebral motion parameters for clinical studies. In: International back and neck pain research forum. Oslo
Couloumbe BJ, Games KE, Neil ER, Eberman LE (2017) Core stability exercise versus general exercise for chronic low back pain. J Athl Train 52:71–72
Saragiotto BT, Maher CG, Yamato TP, Costa LOP, Menezes Costa LC, Ostelo RWJG, Macedo LG (2016) Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012004
Shamsi M, Srragzadeh J, Jamshidi A, Arjmand N, Ghezelbash F (2017) Comparison of spinal stability following motor control and general exercises in nonspecific chronic low back pain patients. Clin Biomech 48:42–48
Shahvarpour A, Henry SM, Preuss R, Mecheri H, Lariviere C (2017) The effect of an 8-week stabilzation exercise program on the lumbopelvic rhythm and flexion-relaxation phenomenon. Clin Biomech 48:1–8
Pranta A, Perraton L, El-Ansary D, Clark R, Fortin K, Dettmann T, Brandham R, Bryant A (2017) Lumbar extensor muscle force control is associated with disability in people with chronic low back pain. Clin Biomech 46:46–51
Panjabi MM (2006) A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. Eur Spine J 15:668–676
Xia X-P, Chen H-L, Cheng H-B (2013) Prevalence of adjacent segment degeneration after spine surgery. Spine 38:597–608
Cheng BC, Bellotte JB, Yu A, Swidarski K, Whiting DM (2010) Historical overview and rationale for dynamic fusion. ArgoSpine News J 22:53–56
Park PMD, Garton HJMDM, Gala VCMD, Hoff JTMD, McGillicuddy JEMD (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine 29:1938–1944
Commission E (2000) Ionising radiation (medical exposure) Regulations2000 (as amended) Ionising (medical exposure regulations (Northern Ireland) 2000 (as amended), pp 1–21
Barzilay Y, Segal G, Lotau R, Regev G, Beer Y, Lonner BS, Mor A, Elbaz A (2016) Patients with chronic non-specific low back pain who reported reduction in pain and improvement in function also demonstrated an improvement in gait pattern. Eur Spine J 25:2761–2766. https://doi.org/10.1007/s00586-4004-0
Zanjani-Pour S, Meakin JR, Breen AX, Breen A (2018) Estimation of in vivo inter-vertebral loading during motion using fluoroscopic and magnetic resonance image informed finite element models. J Biomech 70:134–139
Von Forell GA, Stephens TK, Samartzis D, Bowden AE (2015) Low back pain: a biomechanical rationale based on “Patterns” of disc degeneration. Spine 40:1165–1172
Luoma K, Vehmas T, Kerttula L, Gronblad M, Rinne E (2016) Chronic low back pain in relation to Modic changes, bony endplate lesions, and disc degeneration in the prospective MRI Study. Eur Spine J 25:2873–2881
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix: Calculations of motion share heterogeneity
Appendix: Calculations of motion share heterogeneity
The proportional contribution of an individual intervertebral joint angle \( (L_{xi} ) \) to the total lumbar angle \( (CL_{xi} ) \) [where the intervertebral joint level designation (\( x \)) ranges from \( 1 \to n \)] for each image frame \( (i) \) is expressed as a fraction of the sum of the intervertebral joint angles at all levels (\( \mathop \sum \nolimits (L_{1i \to ni} ) \)) for that frame in the sequence, as described in Mellor et al. (2014).
To remove error amplification at the initial and final parts of the sequence, proportional values are filtered to include only the middle 80th percentile of the rate of change in \( CL_{xi} \) across all levels. This is calculated as the first derivative of a level’s \( (x) \) proportional contribution to position in an image frame \( (CL_{xi} ) \).
For each frame in the filtered proportional contribution (\( fCL_{xi} \)), the filtered range of the contributions of all levels \( fRC_{i} \) is calculated as the difference between the maximum and minimum contributions in that image.
Motion share inequality (MSI) is the mean of these ranges across all image frames which were not filtered out \( 1 \to N \)
Motion share variability (MSV) is the square root of the variance (σ2) of the ranges of \( fRC_{i} \) throughout the motion.
expressed as = σ, or \( \sqrt {\frac{{\mathop \sum \nolimits_{i = 1}^{N} (fRC_{i} - MSI)^{2} }}{N}} \)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Breen, A., Mellor, F. & Breen, A. Aberrant intervertebral motion in patients with treatment-resistant nonspecific low back pain: a retrospective cohort study and control comparison. Eur Spine J 27, 2831–2839 (2018). https://doi.org/10.1007/s00586-018-5666-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5666-1