Abstract
Purpose
Radiation exposure is a necessary component of minimally invasive spine procedures to augment limited visualization of anatomy. The surgeon’s exposure to ionizing radiation is not easily recognizable without a digital dosimeter—something few surgeons have access to. The aim of this study was to identify an easy alternative method that uses the available radiation dose data from the C-arm to accurately predict physician exposure.
Methods
The senior surgeon wore a digital dosimeter during all minimally invasive spine fusion procedures performed over a 12-month period. Patient demographics, procedure information, and radiation exposure throughout the procedure were recorded.
Results
Fifty-five minimally invasive spine fusions utilizing 330 percutaneous screws were included. Average radiation dose was 0.46 Rad/screw to the patient. Average radiation exposure to the surgeon was 1.06 ± 0.71 μSv/screw, with a strong positive correlation (r = 0.77) to patient dose. The coefficient of determination (r2) was 0.5928, meaning almost two-thirds of the variability in radiation exposure to the surgeon is explained by radiation exposure to the patient.
Conclusions
Intra-operative radiation exposure to the patient, which is easily identifiable as a continuously updated fluoroscopic monitor, is a reliable predictor of radiation exposure to the surgeon during percutaneous screw placement in minimally invasive spinal fusion surgery and therefore can provide an estimate of exposure without the use of a dosimeter. With this, a surgeon can better understand the magnitude of their exposure on a case-by-case basis rather than on a quarterly basis, or more likely, not at all.
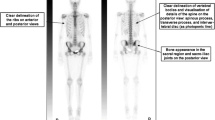
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material


Similar content being viewed by others
Change history
03 December 2019
Unfortunately, the first author surname was incorrectly published as ���Harrison Farber��� instead of ���Farber��� in original publication.
03 December 2019
Unfortunately, the first author surname was incorrectly published as ���Harrison Farber��� instead of ���Farber��� in original publication.
References
Baird EO, Egorova NN, McAnany SJ, Qureshi SA, Hecht AC, Cho SK (2014) National trends in outpatient surgical treatment of degenerative cervical spine disease. Glob Spine J 4:143–150. https://doi.org/10.1055/s-0034-1376917
Angevine PD, Arons RR, McCormick PC (2003) National and regional rates and variation of cervical discectomy with and without anterior fusion, 1990-1999. Spine 28:931–939. https://doi.org/10.1097/01.brs.0000058880.89444.a9 discussion 940
Gupta G, Singh R, Kotasthane DS, Kotasthane VD (2010) Myelodysplastic syndromes/neoplasms: recent classification system based on World Health Organization Classification of Tumors—International Agency for Research on Cancer for Hematopoietic and Lymphoid Tissues. J Blood Med 1:171–182. https://doi.org/10.2147/JBM.S12257
Presciutti SM, Karukanda T, Lee M (2014) Management decisions for adolescent idiopathic scoliosis significantly affect patient radiation exposure. Spine J Off J North Am Spine Soc 14:1984–1990. https://doi.org/10.1016/j.spinee.2013.11.055
Mastrangelo G, Fedeli U, Fadda E, Giovanazzi A, Scoizzato L, Saia B (2005) Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med 55:498–500. https://doi.org/10.1093/occmed/kqi048
Bindal RK, Glaze S, Ognoskie M, Tunner V, Malone R, Ghosh S (2008) Surgeon and patient radiation exposure in minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine 9:570–573. https://doi.org/10.3171/SPI.2008.4.08182
Ul Haque M, Shufflebarger HL, O’Brien M, Macagno A (2006) Radiation exposure during pedicle screw placement in adolescent idiopathic scoliosis: is fluoroscopy safe? Spine 31:2516–2520. https://doi.org/10.1097/01.brs.0000238675.91612.2f
Taher F, Hughes AP, Sama AA, Zeldin R, Schneider R, Holodny EI, Lebl DR, Fantini GA, Nguyen J, Cammisa FP, Girardi FP (2013) 2013 Young Investigator Award winner: how safe is lateral lumbar interbody fusion for the surgeon? A prospective in vivo radiation exposure study. Spine 38:1386–1392. https://doi.org/10.1097/BRS.0b013e31828705ad
Ahn Y, Kim CH, Lee JH, Lee SH, Kim JS (2013) Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: a prospective study. Spine 38:617–625. https://doi.org/10.1097/BRS.0b013e318275ca58
Blakely EA (2000) Biological effects of cosmic radiation: deterministic and stochastic. Health Phys 79:495–506
Mariscalco MW, Yamashita T, Steinmetz MP, Krishnaney AA, Lieberman IH, Mroz TE (2011) Radiation exposure to the surgeon during open lumbar microdiscectomy and minimally invasive microdiscectomy: a prospective, controlled trial. Spine 36:255–260. https://doi.org/10.1097/BRS.0b013e3181ceb976
Kim CH, Lee CH, Kim KP (2016) How high are radiation-related risks in minimally invasive transforaminal lumbar interbody fusion compared with traditional open surgery? A meta-analysis and dose estimates of ionizing radiation. Clin Spine Surg 29:52–59. https://doi.org/10.1097/BSD.0000000000000351
Srinivasan D, Than KD, Wang AC, La Marca F, Wang PI, Schermerhorn TC, Park P (2014) Radiation safety and spine surgery: systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg 82:1337–1343. https://doi.org/10.1016/j.wneu.2014.07.041
Kaminski L, Cordemans V, Cartiaux O, Van Cauter M (2017) Radiation exposure to the patients in thoracic and lumbar spine fusion using a new intraoperative cone-beam computed tomography imaging technique: a preliminary study. Eur Spine J 26:2811–2817. https://doi.org/10.1007/s00586-017-4968-z
Mroz TE, Yamashita T, Davros WJ, Lieberman IH (2008) Radiation exposure to the surgeon and the patient during kyphoplasty. J Spinal Disord Tech 21:96–100. https://doi.org/10.1097/BSD.0b013e31805fe9e1
Harstall R, Heini PF, Mini RL, Orler R (2005) Radiation exposure to the surgeon during fluoroscopically assisted percutaneous vertebroplasty: a prospective study. Spine 30:1893–1898
Grelat M, Greffier J, Sabatier P, Dauzac C, Lonjon G, Debono B, Le Roy J, Kouyoumdjian P, Lonjon N (2016) Assessment of the radiation exposure of surgeons and patients during a lumbar microdiskectomy and a cervical microdiskectomy: a French Prospective Multicenter Study. World Neurosurg 89:329–336. https://doi.org/10.1016/j.wneu.2016.02.021
Lee K, Lee KM, Park MS, Lee B, Kwon DG, Chung CY (2012) Measurements of surgeons’ exposure to ionizing radiation dose during intraoperative use of C-arm fluoroscopy. Spine 37:1240–1244. https://doi.org/10.1097/BRS.0b013e31824589d5
Synowitz M, Kiwit J (2006) Surgeon’s radiation exposure during percutaneous vertebroplasty. J Neurosurg Spine 4:106–109. https://doi.org/10.3171/spi.2006.4.2.106
Choi HC (2011) Fluoroscopic radiation exposure during percutaneous kyphoplasty. J Korean Neurosurg Soc 49:37–42. https://doi.org/10.3340/jkns.2011.49.1.37
McArthur N, Conlan DP, Crawford JR (2015) Radiation exposure during scoliosis surgery: a prospective study. Spine J Off J North Am Spine Soc 15:S33–36. https://doi.org/10.1016/j.spinee.2014.12.149
Nelson EM, Monazzam SM, Kim KD, Seibert JA, Klineberg EO (2014) Intraoperative fluoroscopy, portable X-ray, and CT: patient and operating room personnel radiation exposure in spinal surgery. Spine J Off J North AmSpine Soc 14:2985–2991. https://doi.org/10.1016/j.spinee.2014.06.003
Villard J, Ryang YM, Demetriades AK, Reinke A, Behr M, Preuss A, Meyer B, Ringel F (2014) Radiation exposure to the surgeon and the patient during posterior lumbar spinal instrumentation: a prospective randomized comparison of navigated versus non-navigated freehand techniques. Spine 39:1004–1009. https://doi.org/10.1097/BRS.0000000000000351
Iprenburg M, Wagner R, Godschalx A, Telfeian AE (2016) Patient radiation exposure during transforaminal lumbar endoscopic spine surgery: a prospective study. Neurosurg Focus 40:E7. https://doi.org/10.3171/2015.11.FOCUS15485
Clark JC, Jasmer G, Marciano FF, Tumialan LM (2013) Minimally invasive transforaminal lumbar interbody fusions and fluoroscopy: a low-dose protocol to minimize ionizing radiation. Neurosurg Focus 35:E8. https://doi.org/10.3171/2013.5.FOCUS13144
Bordoli SJ, Carsten CG 3rd, Cull DL, Johnson BL, Taylor SM (2014) Radiation safety education in vascular surgery training. J Vasc Surg 59:860–864. https://doi.org/10.1016/j.jvs.2013.10.085
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Harrison Farber, S., Nayar, G., Desai, R. et al. Radiation exposure to the surgeon during minimally invasive spine procedures is directly estimated by patient dose. Eur Spine J 27, 1911–1917 (2018). https://doi.org/10.1007/s00586-018-5653-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5653-6