Abstract
Purpose
Documents indicated that the average prevalence of intraspinal neural axis abnormalities (INAAs) in presumed idiopathic scoliosis (PIS) patients was about 17.7%. However, paucity study focuses on the incidence of INAAs in severe spinal deformity (SSDs). In this study, we investigate the incidence of intraspinal neural axis abnormalities (IINAAs) and the clinical relevance in SSD at a single center.
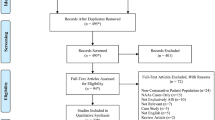
Methods
All the patients with SSDs admitted for spinal surgery were evaluated from 2003 to 2014. Inclusion criteria: patients who present with coronal Cobb over 90° (and/or the sagittal Cobb ≥ 90°); patients with whole spine magnetic resonance imaging (MRI) done preoperatively; and patients with documented clinical findings preoperatively. Exclusion criteria: ankylosing spondylitis, adult onset scoliosis, scoliosis secondary to bone destruction, and spinal dysraphism.
Results
101 patients fulfilled the criteria were included. 43 patients were detected with INAAs (42.6%, 43/101). The most common INAAs was syrinx (S) (16/43, 37.2%). Of which, 43.7% (7/16), 37.5% (6/16), and 18.7% (3/16) were spindle, slit, and swelling types, respectively. Most of them were located in thoracic (6/16, 37.5%) and cervical (5/16, 31.3%) region. MRI revealed Chiari malformation with syringomyelia (C + S) in ten patients (10/43, 23.2%), Chiari malformation (C) in 6 patients (6/43, 13.9%) and others in 11 patients (11/43, 25.6%). As to the etiology, most patients with INAAs were PIS (34/43, 79.1%). On clinical examination, 16 of 101 patients (16/101, 15.8%) had abnormal neurologic signs. 15 of 16 patients (15/16, 93.7%) with abnormal neurologic signs had INAAs on MRI. On the other hand, 28 of 43 patients (28/43, 65.1%) with INAAs on MRI presented neurologically intact. 28 of 85 patients (28/85, 32.9%) with neurologically intact were detected with INAAs on MRI.
Conclusion
The incidence of INAAs in SSDs was 42.6%. 65.1% of them present intact neurologic status. The most common neural anomaly was syrinx. Preoperative whole spine MRI must be beneficial for SSDs even in the absence of neurological findings.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
References
Morcuende JA, Dolan LA, Vazquez JD et al (2004) A prognostic model for the presence of neurogenic lesions in atypical idiopathic scoliosis. Spine 29:51–58
Singhal R, Perry DC, Prasad S et al (2013) The use of routine preoperative magnetic resonance imaging in identifying intraspinal anomalies in patients with idiopathic scoliosis: a 10-year review. Eur Spine J 22:355–359
Martin BD, McClung A, Denning JR et al (2014) Intrathecal anomalies in presumed infantile idiopathic scoliosis: when is MRI necessary? Spine Deform 2:444–447
Dobbs Matthew B, Lenke Lawrence G, Szymanski DA et al (2002) Prevalence of neural axis abnormalities in patients with infantile idiopathic scoliosis. J Bone Jt Surg Am 84:2230–2234
Inoue M, Minami S, Nakata Y et al (2005) Preoperative MRI analysis of patients with idiopathic scoliosis a prospective study. Spine 30:108–114
Hamzaoglu A, Ozturk C, Tezer M et al (2008) Simultaneous surgical treatment in congenital scoliosis and/or kyphosis associated with intraspinal abnormalities. Spine 32:2880–2884
Pahys JM, Samdani AF, Betz RR et al (2009) Intraspinal anomalies in infantile idiopathic scoliosis prevalence and role of magnetic resonance imaging. Spine 34:434–438
Zhang W, Sha S, Xu L et al (2016) The prevalence of intraspinal anomalies in infantile and juvenile patients with “presumed idiopathic” scoliosis: a MRI-based analysis of 504 patients. BMC Musculoskelet Disord (Engl) 17:189
Ghandhari H, Tari HV, Ameri E et al (2015) Vertebral, rib, and intraspinal anomalies in congenital scoliosis: a study on 202 Caucasians. Eur Spine J 24(7):1510–1521
Sucato DJ et al (2010) Management of severe spinal deformity scoliosis and kyphosis. Spine 35:2186–2192
Jankowski PP, Bastrom T, Ciacci JD et al (2016) Intraspinal pathology associated with pediatric scoliosis: a ten-year review analyzing the effect of neurosurgery on scoliosis curve progression. Spine 41:1600–1605
Inoue M, Minami S, Nakata Y et al (2004) Preoperative MRI analysis of patients with idiopathic scoliosis. A prospective study. Spine 30:108–114
Furuya K, Sano K, Segawa H et al (1998) Symptomatic tonsillar ectopia. J Neurol Neurosurg Psychiatry 64:221–226
Noordeen MH, Taylor BA, Edgar MA et al (1994) Syringomyelia. a potential risk factor in scoliosis surgery. Spine 19:1406–1409
Xie JM, Zhang Y, Wang YS et al (2014) The risk factors of neurologic deficits of one-stage posterior vertebral column resection for patients with severe and rigid spinal deformities. Eur Spine J 23:149–156
Milhorat TH et al (2000) Classification of syringomyelia. Neurosurg Focus 8:1
Sakushima K, Tsuboi S, Yabe I et al (2012) Nationwide survey on the epidemiology of syringomyelia in Japan. J Neurol Sci 313:147–152
Brickell KL, Anderson NE, Charleston AJ et al (2006) Ethnic differences in syringomyelia in New Zealand. J Neurol Neurosurg Psychiatry 77:989–991
Strahle J, Muraszko KM, Kapurch J et al (2011) Chiari malformation type I and syringomyelia in children undergoing magnetic resonance imaging. J Neurosurg Pediatr 8:205–213
Kelly MP, Guillaume TJ, Lenke LG et al (2015) Spinal deformity associated with Chiari malformation. Neurosurg Clin N Am 26:579–585
Tubbs RS, Beckman J, Naftel RP et al (2011) Institutional experience with 500 cases of surgically treated pediatric Chiari malformation Type I. J Neurosurg Pediatr 7:248–256
Tubbs RS, McGirt MJ, Oakes WJ et al (2003) Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg 99:291–296
Aitken LA, Lindan CE, Sidney S et al (2009) Chiari type I malformation in a pediatric population. Pediatr Neurol 40:449454
Strahle J, Muraszko KM, Kapurch J et al (2011) Chiari malformation Type I and syringomyelia in children undergoing magnetic resonance imaging. J Neurosurg Pediatr 8(2):205–213
Farley FA, Puryear A, Hall JM et al (2002) Curve progression in scoliosis associated with Chiari I malformation following suboccipital decompression. J Spinal Disord Tech 15:410–414
Whitaker C, Schoenecker PL, Lenke LG et al (2003) Hyperkyphosis as an indicator of syringomyelia in idiopathic scoliosis: a case report. Spine 28:16–20
Lewonowski K, King JD, Nelson MD et al (1992) Routine use of magnetic resonance imaging in idiopathic scoliosis patients less than eleven years of age. Spine 17(6 Suppl):109–116
Gupta P, Lenke LG, Bridwell KH et al (1998) Incidence of neural axis abnormalities in infantile and juvenile patients with spinal deformity. Spine 23:206–210
Belmont PJ Jr, Kuklo TR, Taylor KF et al (2004) Intraspinal anomalies associated with isolated congenital hemivertebra: the role of routine magnetic resonance imaging. J Bone Jt Surg Am 86:1704–1710
Acknowledgements
The manuscript submitted does not contain information about medical device(s)/drug(s). Fund from the Joint Special Fund of Kunming Medical (Grant No. 2015FB053) was received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Y., Xie, J., Wang, Y. et al. Intraspinal neural axis abnormalities in severe spinal deformity: a 10-year MRI review. Eur Spine J 28, 421–425 (2019). https://doi.org/10.1007/s00586-018-5522-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5522-3