Abstract
Purpose
Recent literature has reported that the ]progression risk of Lenke 5 adolescent idiopathic scoliosis (AIS) during adulthood had been underestimated. Surgery is, therefore, proposed more to young patients with progressive curves. However, choice of the approach and fusion levels remains controversial. The aim of this study was to analyze the influence of the length of posterior fusion on clinical and radiological outcomes in Lenke 5 AIS.
Methods
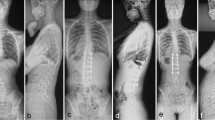
All Lenke 5 AIS operated between 2008 and 2012 were included with a minimum 2-year follow-up. Patients were divided into two groups according to the length of fusion. In the first group (selective), the upper instrumented level (UIV) was the upper end vertebra of the main structural curve and distally the fusion was extended to the stable and neutral vertebra, according to Lenke’s classification. In the second group (hyperselective), shorter fusions were performed and the number of levels fused depended on the location of the apex of the curve (at maximum, 2 levels above and below, according to Hall’s criteria). Apart from the fusion level selection, the surgical procedure was similar in both groups. Radiological outcomes and SRS-22 scores were reported.
Results
78 patients were included (35 selective and 43 hyperselective). The number of levels fused was significantly higher in the first group (7.8 ± 3 vs 4.3 ± 0.6). None of the patients was fused to L4 in selective group. No correlation was found between length of fusion and complication rate. Eight patients had adding-on phenomenon among which 6 (75%) had initially undergone hyperselective fusions and had significantly higher postoperative lower instrumented vertebra (LIV) tilt. In the adding-on group, LIV was located above the last touching vertebra (LTV) in 62.5% of the cases and above the stable vertebra (SV) in 87.5%. Patients in the selective group reported a significantly lower score in the SRS function domain.
Conclusion
Coronal alignment was restored in both groups. Hyperselective posterior fusions can be considered in Lenke 5 AIS, preserving one or two mobile segments, with similar clinical and radiological outcomes. However, selection of the LIV according to SV and LTV need to be accurately analyzed in order to avoid adding-on during follow-up.



Similar content being viewed by others
References
Pesenti S, Jouve J-L, Morin C, Wolff S, Sales de Gauzy J, Chalopin A et al (2015) Evolution of adolescent idiopathic scoliosis: results of a multicenter study at 20 years’ follow-up. Orthop Traumatol Surg Res 101:619–622
Ilharreborde B, Morel E, Mazda K, Dekutoski MB (2009) Adjacent segment disease after instrumented fusion for idiopathic scoliosis: review of current trends and controversies. J Spinal Disord Tech. 22(7):530–539
Danielsson AJ, Nachemson AL (2003) Back pain and function 23 years after fusion for adolescent idiopathic scoliosis: a case-control study—part II. Spine 28(18):E373–E383
Sanchez-Raya J, Bago J, Pellise F, Cuxart A, Villanueva C (2012) Does the lower instrumented vertebra have an effect on lumbar mobility, subjective perception of trunk flexibility, and quality of life in patients with idiopathic scoliosis treated by spinal fusion? J Spinal Disord Tech 25(8):437–442
Paonessa KJ, Engler GL (1992) Back pain and disability after Harrington rod fusion to the lumbar spine for scoliosis. Spine 17(8 Suppl):S249–S253
Pérez-Grueso FS, Fernández-Baíllo N, Arauz de Robles S, García Fernández A (2000) The low lumbar spine below Cotrel-Dubousset instrumentation: long-term findings. Spine 25(18):2333–2341
Takayama K, Nakamura H, Matsuda H (2009) Quality of life in patients treated surgically for scoliosis: longer than sixteen-year follow-up. Spine 34(20):2179–2184
Helenius I, Remes V, Yrjönen T, Ylikoski M, Schlenzka D, Helenius M et al (2002) Comparison of long-term functional and radiologic outcomes after Harrington instrumentation and spondylodesis in adolescent idiopathic scoliosis: a review of 78 patients. Spine 27(2):176–180
Ding R, Liang J, Qiu G, Shen J, Li Z (2014) Evaluation of quality of life in adolescent idiopathic scoliosis with different distal fusion level: a comparison of L3 versus L4. J Spinal Disord Tech. 27(5):E155–E161
Hall JE (1972) The anterior approach to spinal deformities. Orthop Clin North Am 3(1):81–98
Yu B, Wang Y, Qiu G, Zhang J, Shen J, Li Q et al (2009) Comparison of correction outcomes after anterior or posterior approach with lowest and vertebra instrumentation in adolescent idiopathic thoracolumbar/lumbar scoliosis. Zhonghua Yi Xue Za Zhi 89(37):2621–2625
Matsumoto M, Watanabe K, Hosogane N, Kawakami N, Tsuji T, Uno K et al (2013) Postoperative distal adding-on and related factors in Lenke type 1A curve. Spine 38(9):737–744
Koller H, Meier O, Hitzl W (2014) Criteria for successful correction of thoracolumbar/lumbar curves in AIS patients: results of risk model calculations using target outcomes and failure analysis. Eur Spine J 23(12):2658–2671
Kim S-S, Lim D-J, Kim J-H, Kim J-W, Um K-S, Ahn S-H et al (2014) Determination of the distal fusion level in the management of thoracolumbar and lumbar adolescent idiopathic scoliosis using pedicle screw instrumentation. Asian Spine J 8(6):804
Li J, Hwang SW, Shi Z, Yan N, Yang C, Wang C et al (2011) Analysis of radiographic parameters relevant to the lowest instrumented vertebrae and postoperative coronal balance in Lenke 5C patients. Spine 36(20):1673–1678
Nash CL, Moe JH (1969) A study of vertebral rotation. J Bone Jt Surg Am 51(2):223–229
Bernstein RM, Hall JE (1998) Solid rod short segment anterior fusion in thoracolumbar scoliosis. J Pediatr Orthop Part B. 7(2):124–131
Faro FD, Marks MC, Pawelek J, Newton PO (2004) Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine 29(20):2284–2289
Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG et al (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Jt Surg Am 83A(8):1169–1181
Berjano P, Cecchinato R, Damilano M, Morselli C, Sansone V, Lamartina C (2013) Preoperative calculation of the necessary correction in sagittal imbalance surgery: validation of three predictive methods. Eur Spine J 22(Suppl 6):S847–S852
Lamartina C, Berjano P, Petruzzi M, Sinigaglia A, Casero G, Cecchinato R et al (2012) Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J 21(Suppl 1):S27–S31
Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Jt Surg Am 87(2):260–267
Lonjon G, Ilharreborde B, Odent T, Moreau S, Glorion C, Mazda K (2014) Reliability and validity of the French–Canadian version of the scoliosis research society 22 questionnaire in France. Spine 39(1):E26–E34
Wang Y, Bünger CE, Zhang Y, Wu C, Li H, Hansen ES (2013) Distal adding-on in Lenke 1A scoliosis: how to more effectively determine the onset of distal adding-on. Spine 38(6):490–495
Helgeson MD, Shah SA, Newton PO, Clements DH, Betz RR, Marks MC et al (2010) Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine 35(2):177–181
Kim Y-C, Lenke LG, Bridwell KH, Hyun S-J, You K-H, Kim Y-W et al (2016) Results of revision surgery for proximal junctional kyphosis following posterior segmental instrumentation: minimum 2-year post-revision follow-up. Spine 41:E1444–E1452
Marty-Poumarat C, Scattin L, Marpeau M, Garreau de Loubresse C, Aegerter P (2007) Natural history of progressive adult scoliosis. Spine 32(11):1227–1234 (discussion 1235)
Jackson RP, McManus AC (1994) Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine 19(14):1611–1618
Chang DG, Yang JH, Suk SI, Suh SW, Kim YH, Cho W et al (2016) Importance of distal fusion level in major thoracolumbar and lumbar adolescent idiopathic scoliosis treated by rod derotation and direct vertebral rotation following pedicle screw instrumentation. Spine (Phila Pa 1976). doi:10.1097/BRS.0000000000001998
Yang C, Zhao Y, Zhai X, Li J, Zhu X, Li M (2016) Coronal balance in idiopathic scoliosis: a radiological study after posterior fusion of thoracolumbar/lumbar curves (Lenke 5 or 6). Eur Spine J. doi:10.1007/s00586-016-4844-2
Lee CS, Ha J-K, Hwang CJ, Lee D-H, Kim TH, Cho JH (2016) Is it enough to stop distal fusion at L3 in adolescent idiopathic scoliosis with major thoracolumbar/lumbar curves? Eur Spine J 25(10):3256–3264
Sudo H, Ito M, Kaneda K, Shono Y, Abumi K (2013) Long-term outcomes of anterior dual-rod instrumentation for thoracolumbar and lumbar curves in adolescent idiopathic scoliosis: a twelve to twenty-three-year follow-up study. J Bone Jt Surg Am. 95(8):e49
Green DW, Lawhorne TW, Widmann RF, Kepler CK, Ahern C, Mintz DN et al (2011) Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine 36(23):1948–1954
Xu X-M, Wang F, Zhou X-Y, Liu Z-X, Wei X-Z, Bai Y-S et al (2015) Sagittal balance in adolescent idiopathic scoliosis: a radiographic study of spinopelvic compensation after selective posterior fusion of thoracolumbar/lumbar (Lenke 5C) curves. Medicine (Baltimore) 94(45):e1995
La Maida GA, Zottarelli L, Mineo GV, Misaggi B (2013) Sagittal balance in adolescent idiopathic scoliosis: radiographic study of spino-pelvic compensation after surgery. Eur Spine J 22(S6):859–867
Yang X, Liu L, Song Y, Zhou C, Zhou Z, Wang L et al (2015) Pre- and postoperative spinopelvic sagittal balance in adolescent patients with Lenke Type 5 idiopathic scoliosis. Spine 40(2):102–108
Potter BK, Lenke LG, Kuklo TR (2004) Prevention and management of iatrogenic flatback deformity. J Bone Jt Surg Am 86A(8):1793–1808
Green DW, Lawhorne TW, Widmann RF, Kepler CK, Ahern C, Mintz DN et al (2011) Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine 36(23):1948–1954
Cochran T, Irstam L, Nachemson A (1983) Long-term anatomic and functional changes in patients with adolescent idiopathic scoliosis treated by Harrington rod fusion. Spine 8(6):576–584
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that they have no potential conflict of interest.
Rights and permissions
About this article
Cite this article
Ilharreborde, B., Ferrero, E., Angelliaume, A. et al. Selective versus hyperselective posterior fusions in Lenke 5 adolescent idiopathic scoliosis: comparison of radiological and clinical outcomes. Eur Spine J 26, 1739–1747 (2017). https://doi.org/10.1007/s00586-017-5070-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5070-2