Abstract
Purpose
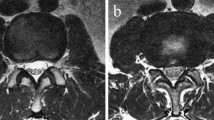
The nerve root sedimentation sign (SedSign) is a magnetic resonance imaging (MRI) sign for the diagnosis of lumbar spinal stenosis (LSS). It is included in the assessment of LSS to help determine whether decompression surgery is indicated. Assessment of the reversibility of the SedSign after surgery may also have clinical implications for the decision about whether or not a secondary operation or revision is needed. This study investigated if lumbar decompression leads to a reversal of the SedSign in patients with LSS and a positive SedSign pre-operatively; and if a reversal is associated with more favourable clinical outcomes. If reversal of the SedSign is usual after sufficient decompression surgery, a new positive SedSign could be used as an indicator of new stenosis in previously operated patients.
Methods
A prospective cohort study of 30 LSS patients with a positive pre-operative SedSign undergoing decompression surgery with or without instrumented fusion was undertaken to assess the presence of nerve root sedimentation (=negative SedSign) on MRI at 3 months post-operation. Functional limitation (Oswestry Disability Index, ODI), back and leg pain (Visual Analogue Scale, VAS), and treadmill walking distance were also compared pre- and 3 months post-operatively. The short follow-up period was chosen to exclude adjacent segment disease and the potential influence of surgical technique on clinical outcomes at longer follow-up times.
Results
30 patients [median age 73 years (interquartile range (IQR) 65–79), 16 males] showed a median pre-operative ODI of 66 (IQR 52–78), a median VAS of 8 (IQR 7–9), and a median walking distance of 0 m (IQR 0–100). Three months post-operation 27 patients had a negative SedSign. In this group, we found improved clinical outcomes at follow-up: median post-operative ODI of 21 (IQR 12–26), median VAS of 2 (IQR 2–4), and median walking distance of 1000 m (IQR 500–1000). These changes were all statistically significant (p < 0.001). Three patients had a positive SedSign at 3-month follow-up due to epidural fat (n = 2) or a dural cyst following an intra-operative dural tear (n = 1), but also showed improvements in clinical outcomes for ODI, VAS and walking distance.
Conclusion
The reversibility of a pre-operative positive SedSign was demonstrated after decompression of the affected segmental level and associated with an improved clinical outcome. A persisting positive SedSign could be the result of incomplete decompression or surgical complications. A new positive SedSign after sufficient decompression surgery could be used as an indicator of new stenosis in previously operated patients.




Similar content being viewed by others
References
Verbiest H (1954) A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Jt Surg Br 36-B(2):230–237
Deyo RA et al (2005) United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 30(12):1441–1445 discussion 1446–7
Aizawa T et al (2015) Reoperation rates after fenestration for lumbar spinal canal stenosis: a 20-year period survival function method analysis. Eur Spine J 24(2):381–387
Modhia U et al (2013) Readmission rates after decompression surgery in patients with lumbar spinal stenosis among medicare beneficiaries. Spine (Phila Pa 1976) 38(7):591–596
Forsth P et al (2016) A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 374(15):1413–1423
Ghogawala Z et al (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374(15):1424–1434
Barz T et al (2010) Nerve root sedimentation sign: evaluation of a new radiological sign in lumbar spinal stenosis. Spine (Phila Pa 1976) 35(8):892–897
Barz T et al (2014) Clinical validity of the nerve root sedimentation sign in patients with suspected lumbar spinal stenosis. Spine J 14(4):667–674
Weber C et al (2016) Is there an association between radiological severity of lumbar spinal stenosis and disability, pain, or surgical outcome? A multicenter observational study. Spine (Phila Pa 1976) 41(2):E78–E83
Moses RA et al (2015) Is the sedimentation sign associated with spinal stenosis surgical treatment effect in SPORT? Spine (Phila Pa 1976) 40(3):129–136
Macedo LG, Wang Y, Battie MC (2013) The sedimentation sign for differential diagnosis of lumbar spinal stenosis. Spine (Phila Pa 1976) 38(10):827–831
Zhang L et al (2015) Diagnostic value of the nerve root sedimentation sign, a radiological sign using magnetic resonance imaging, for detecting lumbar spinal stenosis: a meta-analysis. Skelet Radiol 44(4):519–527
Schizas C et al (2010) Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976) 35(21):1919–1924
Lonne G et al (2014) MRI evaluation of lumbar spinal stenosis: is a rapid visual assessment as good as area measurement? Eur Spine J 23(6):1320–1324
Sakai Y et al (2017) Clinical outcome of lumbar spinal stenosis based on new classification according to hypertrophied ligamentum flavum. J Orthop Sci 22(1):27–33
Fairbank JC et al (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66(8):271–273
Schmidt JD et al (1976) Chemotherapy of advanced prostatic cancer. Evaluation of response parameters. Urology 7(6):602–610
Barz T et al (2008) The diagnostic value of a treadmill test in predicting lumbar spinal stenosis. Eur Spine J 17(5):686–690
Deyo RA et al (2013) Complications after surgery for lumbar stenosis in a veteran population. Spine (Phila Pa 1976) 38(19):1695–1702
Booth KC et al (1999) Minimum 5-year results of degenerative spondylolisthesis treated with decompression and instrumented posterior fusion. Spine (Phila Pa 1976) 24(16):1721–1727
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20(1):37–46
Tomkins-Lane CC et al (2013) Nerve root sedimentation sign for the diagnosis of lumbar spinal stenosis: reliability, sensitivity, and specificity. Spine (Phila Pa 1976) 38(24):E1554–E1560
Melloh M et al (2013) Is the positive nerve root sedimentation sign in patients with lumbar spinal stenosis reversible after decompression surgery? The International Society for the Study of the Lumbar Spine Annual Meeting, Scottsdale, AZ, 13th–17th May 2013
Barz T et al (2014) Increased intraoperative epidural pressure in lumbar spinal stenosis patients with a positive nerve root sedimentation sign. Eur Spine J 23(5):985–990
Laitt R, Jackson A, Isherwood I (1996) Patterns of chronic adhesive arachnoiditis following Myodil myelography: the significance of spinal canal stenosis and previous surgery. Br J Radiol 69(824):693–698
Kim NH, Yang IH (1996) A study of motor and sensory evoked potentials in chronic cauda equina compression of the dog. Eur Spine J 5(5):338–344
Gerling MC et al (2016) Risk factors for reoperation in patients treated surgically for lumbar stenosis: a subanalysis of the 8 year data from the SPORT trial. Spine (Phila Pa 1976) 41(10):901–909
Leonardi MA et al (2010) Early postoperative MRI in detecting hematoma and dural compression after lumbar spinal decompression: prospective study of asymptomatic patients in comparison to patients requiring surgical revision. Eur Spine J 19(12):2216–2222
Oba H et al (2013) Study of dural sac cross-sectional area in early and late phases after lumbar decompression surgery. Spine J 13(9):1088–1094
Kao FC et al (2015) Symptomatic epidural hematoma after lumbar decompression surgery. Eur Spine J 24(2):348–357
Shimizu T et al (2016) A multi-center study of reoperations within 30 days of spine surgery. Eur Spine J 25(3):828–835
Munting E et al (2015) Patient outcomes after laminotomy, hemilaminectomy, laminectomy and laminectomy with instrumented fusion for spinal canal stenosis: a propensity score-based study from the Spine Tango registry. Eur Spine J 24(2):358–368
Wells AJ et al (2014) Lumbosacral epidural lipomatosis causing rapid onset cauda equina syndrome. J Clin Neurosci 21(7):1262–1263
Zhang L et al (2016) The nerve root sedimentation sign for differential diagnosis of lumbar spinal stenosis: a retrospective, consecutive cohort study. Eur Spine J. doi:10.1007/s00586-016-4435-2
de Schepper EI et al (2013) Diagnosis of lumbar spinal stenosis: an updated systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976) 38(8):E469–E481
Andreisek G et al (2014) Consensus conference on core radiological parameters to describe lumbar stenosis—an initiative for structured reporting. Eur Radiol 24(12):3224–3232
Tomkins-Lane C et al (2016) Consensus on the clinical diagnosis of lumbar spinal stenosis: results of an international Delphi study. Spine (Phila Pa 1976)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no potential conflict of interest.
Rights and permissions
About this article
Cite this article
Barz, C., Melloh, M., Staub, L.P. et al. Reversibility of nerve root sedimentation sign in lumbar spinal stenosis patients after decompression surgery. Eur Spine J 26, 2573–2580 (2017). https://doi.org/10.1007/s00586-017-4962-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-4962-5