Abstract
Background
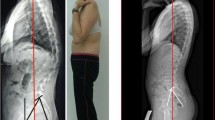
Pelvic balance is a version of the pelvis defined by pelvic orientation parameters of PT and SS. Two distinct versions of pelvis are defined: (1) balanced characterized by a relatively low PT and high SS, and (2) unbalanced with relatively high PT and low SS meaning excessive retroversion of the pelvis. It was proved for patients with a high-grade spondylolisthesis that rebalancing of the pelvis can positively affect clinical outcomes. Little is known about the impact of such rebalancing in low-grade isthmic spondylolisthesis.
Purpose
To determine whether clinical outcomes correlated with rebalancing of the pelvis after surgical correction of mid- and low-grade adult isthmic spondylolisthesis.
Methods
One hundred and three adult patients with a mid- and low-grade isthmic slip were the participants. Clinical outcomes were assessed at least 2 years after the surgery with the use of the Oswestry Disability Index (ODI) and a back pain visual analogue scale. Statistical analysis was used to identify differences in clinical outcomes between patients (1) with a balanced and unbalanced pelvis postoperatively, (2) who regained and did not regain pelvic balance postoperatively, (3) who maintained and lost pelvic balance postoperatively, and (4) with reduced and increased postoperative PT.
Results
There were no significant differences in clinical outcomes between patients with a balanced and unbalanced pelvis postoperatively regardless of whether they lost, maintained, or regained pelvic balance after the surgery (Student’s t test for independent variables or the non-parametric Mann–Whitney U, p value = 0.05). No correlation (Spearman’s rank correlation) was found between postoperative reduction of PT and postoperative: (1) level of back pain (r = −0.10, p = 0.3063), (2) degree of reduction in back pain (r = 0.03, p = 0.7927), (3) ODI scores (r = −0.18, p = 0.0696), and (4) degree of reduction in ODI scores (r = 0.13, p = 0.1893).
Conclusions
Radiological improvement of pelvic balance after surgical correction of mid- and low-grade isthmic spondylolisthesis did not correlate with clinical outcomes.







Similar content being viewed by others
References
Labelle H, Roussouly P, Chopin D et al (2003) The importance of spino-pelvic balance after spinal instrumentation for high grade spondylolisthesis. Scoliosis Research Society Annual Meeting, Quebec City
Labelle H, Roussouly P, Berthonnaud E et al (2005) The importance of spino-pelvic balance in L5–S1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine 30:S27–S34
Hresko MT, Labelle H, Roussouly P et al (2007) Classification of high-grade spondylolistheses based on pelvic version and spine balance: possible rationale for reduction. Spine 32:2208–2213
Mac-Thiong JM, Labelle H, Parent S et al (2008) Reliability and development of a new classification of lumbosacral spondylolisthesis. Scoliosis 3:19
Vialle R, Ilharreborde B, Dauzac CI et al (2007) Is there a sagittal imbalance of the spine in isthmic spondylolisthesis? A correlation study. Eur Spine J 16:1641–1649
Labelle H, Mac-Thiong JM, Roussouly P (2011) Spino-pelvic sagittal balance of spondylolisthesis: review and classification. Eur Spine J 20:S641–S646
Labelle H, Roussouly P, Chopin D (2008) Spino-pelvic alignment after surgical correction for developmental spondylolisthesis. Eur Spine J 17:1170–1176
Feng Y, Chen L, Gu Y et al (2014) Influence of the posterior lumbar interbody fusion on the sagittal spino-pelvic parameters in isthmic L5–S1 spondylolisthesis. J Spinal Disord Tech 27:E20–E25
Mac-Thiong JM, Wang Z, de Guise JA et al (2008) Postural model of sagittal spino-pelvic alignment and its relevance for lumbosacral developmental spondylolisthesis. Spine 33:2316–2325
Roussouly P, Gollogly S, Berthonnaud E et al (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30:346–353
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20:S609–S618
Bourghli A, Aunoble S, Reebye O et al (2011) Correlation of clinical outcome and spinopelvic sagittal alignment after surgical treatment of low-grade isthmic spondylolisthesis. Eur Spine J 20:S663–S668
Lazennec JY, Ramaré S, Arafati N et al (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9:47–55
Schwab F, Lafage V, Patel A et al (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine 34:828–1833
Hresko MT, Hirschfeld R, Buerk AA et al (2009) The effect of reduction and instrumentation of spondylolisthesis on spinopelvic sagittal alignment. J Pediatr Orthop 29:157–162
Lafage V, Schwab F, Patel A et al (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 34:E599–E606
Maciejczak A, Jabłońska K, Bączek D et al (2014) Changes in spino-pelvic alignment after surgical treatment of isthmic spondylolisthesis. Neurol Neurochir Pol 48:21–29
Duval-Beaupere G, Robain G (1987) Visualisation on full spine radiographs of the anatomical connections of the centres of the segmental body mass supported by each vertebra and measured in vivo. Int Orthop 11:261–269
Legaye J, Duval-Beaupere G, Hecquet J et al (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Boulay C, Tardieu C, Hecquet J et al (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 15:415–422
Barrey C, Jund J, Perrin G et al (2007) Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery 61:981–986
Vialle R, Levassor N, Rillardon L et al (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am 87:260–267
Vaz G, Roussouly P, Berthonnaud E et al (2002) Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 11:80–87
Labelle H, Roussouly P, Berthonnaud E et al (2004) Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine 29:2049–2054
Park SJ, Lee CS, Chung S et al (2011) Postoperative changes in pelvic parameters and sagittal balance in adult isthmic spondylolisthesis. Neurosurgery 68:355–363
Yang EZ, Xu JG, Liu XK, Jin GY, Xiao W, Zeng BF, Lian XF (2016) Surgery for adult spondylolisthesis: a systematic review of the evidence. Eur Spine J 25:1587–1594. doi:10.1007/s00586-015-4341-z
Hsu HT, Yang SS, Chen TY (2016) The correlation between restoration of lumbar lordosis and surgical outcome in the treatment of low-grade lumbar degenerative spondylolisthesis with spinal fusion. Clin Spine Surg (United States) 29(1):pE16–pE20
Jablonska-Sudol K, Maciejczak A (2015) Relationship between the spino-pelvic parameters and the slip grade in isthmic spondylolisthesis. Neurol Neurochir Pol (Poland) 49(6):p381–p388
Schulte TL, Ringel F, Quante M, Eicker SO, Muche-Borowski C, Kothe R (2015) Surgery for adult spondylolisthesis: a systematic review of the evidence. Eur Spine J (Epub ahead of print)
Debnath UK, Chatterjee A, McConnell JR et al (2016) Interbody fusion in low grade lumbar spondylolisthesis: clinical outcome does not correlate with slip reduction and neural foraminal dimension. Asian Spine J (Korea South) 10(2):314–320
Zhu F, Bao H, Liu Z et al (2014) Analysis of L5 incidence in normal population use of L5 incidence as a guide in reconstruction of lumbosacral alignment. Spine 39(2):E140–E146
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Maciejczak, A., Jabłońska-Sudoł, K. Correlation between correction of pelvic balance and clinical outcomes in mid- and low-grade adult isthmic spondylolisthesis. Eur Spine J 26, 3112–3121 (2017). https://doi.org/10.1007/s00586-016-4808-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4808-6