Abstract
Purpose
Dynamic trunk flexion–extension testing has been proven to objectively diagnose low back pain in persons under the age of 60 years but older persons have difficulty complying with standardized movement velocity.
Methods
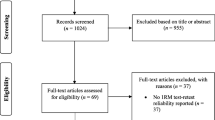
190 patients and 71 matched healthy volunteers (18–90 years of age) performed modified testing by holding static positions at standing, half, and full trunk flexion.
Results
Lumbar extensor muscle activity in isometric positions was significantly higher in patients with higher activity in the oldest (60–90 years) and the middle-aged (40–59 years) but not in the youngest (18–39 years) subgroups compared to normal. There were no differences in gross trunk range of motion, half flexion relaxation ratio, proprioception, muscle activity differences between positions, and fear-avoidance behavior. The diagnostic accuracy as expressed by the area under the curve was fair (0.74).
Conclusions
Lumbar extensor muscle activity demonstrated moderate to good diagnostic value in old patients.


Similar content being viewed by others
Abbreviations
- RMS SEMG:
-
Root mean square surface electromyography (–ic)
- ROM:
-
Range of motion
- MVC:
-
Maximum voluntary contraction
- HFR:
-
Half flexion relaxation ratio
- PRM:
-
Physical medicine and rehabilitation
- 3d-accelerometer:
-
Three dimensional accelerometer
- L5:
-
Lumbar spine level 5
- T4:
-
Thoracic spine level 4
- s:
-
Second
- kg/m2 :
-
Kilogram per square meter
- ROC:
-
Receiver operating analysis
- AUC:
-
Area under the curve
References
Laird RA, Gilbert J, Kent P, Keating JL (2014) Comparing lumbo-pelvic kinematics in people with and without back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord 1:1–13. doi:10.1186/1471-2474-15-229
Mayer TG, Neblett R, Brede E, Gatchel RJ (2009) The quantified lumbar flexion-relaxation phenomenon is a useful measurement of improvement in a functional restoration program. Spine 22:2458–2465. doi:10.1097/BRS.0b013e3181b20070
Neblett R, Mayer TG, Brede E, Gatchel RJ (2010) Correcting abnormal flexion-relaxation in chronic lumbar pain: responsiveness to a new biofeedback training protocol. Clin J Pain 5:403–409. doi:10.1097/AJP.0b013e3181d2bd8c
Neblett R, Mayer TG, Brede E, Gatchel RJ (2014) The effect of prior lumbar surgeries on the flexion relaxation phenomenon and its responsiveness to rehabilitative treatment. Spine J. 6:892–902. doi:10.1016/j.spinee.2013.07.442
Watson PJ, Booker CK, Main CJ, Chen AC (1997) Surface electromyography in the identification of chronic low back pain patients: the development of the flexion relaxation ratio. Clin Biomech 3:165–171
Alschuler KN, Neblett R, Wiggert E, Haig AJ, Geisser ME (2009) Flexion-relaxation and clinical features associated with chronic low back pain: a comparison of different methods of quantifying flexion-relaxation. Clin J Pain 9:760–766. doi:10.1097/AJP.0b013e3181b56db6
Neblett R, Brede E, Mayer TG, Gatchel RJ (2013) What is the best surface EMG measure of lumbar flexion-relaxation for distinguishing chronic low back pain patients from pain-free controls? Clin J Pain 4:334–340. doi:10.1097/AJP.0b013e318267252d
Colloca CJ, Hinrichs RN (2005) The biomechanical and clinical significance of the lumbar erector spinae flexion-relaxation phenomenon: a review of literature. J Manipulative Physiol Ther 8:623–631
Descarreaux M, Blouin JS, Teasdale N (2005) Repositioning accuracy and movement parameters in low back pain subjects and healthy control subjects. Eur Spine J 2:185–191. doi:10.1007/s00586-004-0833-y
Hidalgo B, Gilliaux M, Poncin W, Detrembleur C (2012) Reliability and validity of a kinematic spine model during active trunk movement in healthy subjects and patients with chronic non-specific low back pain. J Rehabil Med 9:756–763. doi:10.2340/16501977-1015
Kienbacher T, Paul B, Habenicht R, Starek C, Wolf M, Kollmitzer J, Mair P, Ebenbichler G (2015) Age and gender related neuromuscular changes in trunk flexion-extension. J Neuroeng Rehabil 12:3. doi:10.1186/1743-0003-12-3
Kienbacher T, Fehrmann E, Habenicht R, Koller D, Oeffel C, Kollmitzer J, Mair P, Ebenbichler G (2016) Age and gender related neuromuscular pattern during trunk flexion-extension in chronic low back pain patients. J Neuroeng Rehabil 13:16. doi:10.1186/s12984-016-0121-1
Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS, Furman JM (2005) Clinical measurement of sit-to-stand performance in people with balance disorders: validity of data for the five-times-sit-to-stand test. Phys Ther 10:1034–1045
Bullinger M (1995) German translation and psychometric testing of the SF-36 Health Survey: preliminary results from the IQOLA Project. International quality of life assessment. Soc Sci Med 10:1359–1366
Hasenbring MI, Hallner D, Rusu AC (2009) Fear-avoidance- and endurance-related responses to pain: development and validation of the Avoidance-Endurance Questionnaire (AEQ). Eur J Pain 6:620–628. doi:10.1016/j.ejpain.2008.11.001
Wiesinger GF, Nuhr M, Quittan M, Ebenbichler G, Wolfl G, Fialka-Moser V (1999) Cross-cultural adaptation of the Roland-Morris questionnaire for German-speaking patients with low back pain. Spine 11:1099–1103
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 8:1381–1395. doi:10.1249/01.mss.0000078924.61453.fb
Hermens HJ, Freriks B, Merletti R, Stegeman D, Blok J, Rau G, Disselhorst-Klug C, Hägg G (1999) European recommendations for surface electromyography. Roessingh Res Develop Enschede 2:13–54
Lariviere C, Arsenault AB, Gravel D, Gagnon D, Loisel P (2002) Evaluation of measurement strategies to increase the reliability of EMG indices to assess back muscle fatigue and recovery. J Electromyogr Kinesiol 2:91–102
R Core Team (2015) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/
Geisser ME, Ranavaya M, Haig AJ, Roth RS, Zucker R, Ambroz C, Caruso M (2005) A meta-analytic review of surface electromyography among persons with low back pain and normal, healthy controls. J Pain 11:711–726. doi:10.1016/j.jpain.2005.06.008
Haig AJ, Weismann G, Haugh LD, Pope M, Grobler LJ (1993) Prospective evidence for change in paraspinal muscle activity after herniated nucleus pulposus. Spine 7:926–929
Hodges PW, Tucker K (2011) Moving differently in pain: a new theory to explain the adaptation to pain. Pain 3:90–98
Alschuler KN, Neblett R, Wiggert E, Haig AJ, Geisser ME (2009) Flexion-relaxation and clinical features associated with chronic low back pain: a comparison of different methods of quantifying flexion-relaxation. Clin J Pain 9:760–766
Newcomer KL, Laskowski ER, Yu B, Johnson JC, An KN (2000) Differences in repositioning error among patients with low back pain compared with control subjects. Spine 19:2488–2493
Sánchez-Zuriaga D, Artacho-Pérez C, Biviá-Roig G (2016) Lumbopelvic flexibility modulates neuromuscular responses during trunk flexion–extension. J Electromyogr Kinesiol 28:152–157. doi:10.1016/j.jelekin.2016.04.007
Beneck GJ, Story JW, Donald S (2016) Postural Cueing to increase lumbar lordosis increases lumbar multifidus activation during trunk stabilization exercises: electromyographic assessment using intramuscular electrodes. J Orthop Sports Phys Ther 4:293–299. doi:10.2519/jospt.2016.617429
Acknowledgments
The authors gratefully thank Haley Milko for providing English language corrections.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
In the past 5 years, we have not received reimbursements, fees, funding, financing of the manuscript, or salary from an organization that may in any way gain or lose financially from the publication of this manuscript, either now or in the future.
We do not hold any stocks or shares in an organization that may in any way gain or lose financially from the publication of this manuscript, either now nor in the future.
We do not hold nor are currently applying for any patents relating to the content of the manuscript. We have not received reimbursements, fees, funding, or salary from an organization that holds or has applied for patents relating to the content of the manuscript.
We have no other financial competing interest.
We have no non-financial competing interest (political, personal, religious, ideological, academic, intellectual, commercial, or any other) to declare in relation to the manuscript.
Rights and permissions
About this article
Cite this article
Kienbacher, T., Fehrmann, E., Habenicht, R. et al. Diagnostic value of trunk flexion–extension testing in old chronic low back pain patients. Eur Spine J 26, 510–517 (2017). https://doi.org/10.1007/s00586-016-4758-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4758-z