Abstract
Purpose
Pectus excavatum can negatively impact cardiac function during scoliosis surgery. Several authors reported severe hypotension associated with the prone position during scoliosis surgery in children that had both scoliosis and pectus excavatum. However, we could find no studies that evaluated the change in the thoracic factors, such as sternal tilt angle and Haller index after scoliosis surgery in patients with both scoliosis and pectus excavatum. The purpose of this study is to evaluate the change in thoracic factors after surgical treatment for scoliosis associated with pectus excavatum.
Methods
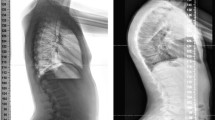
We performed a retrospective review on 20 patients (10 males and 10 females) who underwent surgical treatment for scoliosis associated with pectus excavatum from August 2004 to April 2014 in our hospital. We investigated the scoliosis diagnosis, preoperative and postoperative Cobb and thoracic kyphosis (TK) angles, the change in TK after surgery and thoracic factors, including the AP and transverse diameters of the chest, the sternal tilt angle, and Haller index.
Results
Patient mean age was 13.2 years old (4–27 years old) at surgery. Types of scoliosis were idiopathic in 8 patients, syndromic in 10, and neuromuscular in 2. The mean Cobb angles were 72.1° preoperatively and 19.0° postoperatively. Curve locations were thoracic in 13 patients, thoracolumbar in 4, and lumbar in 3. Surgical treatment of pectus excavatum was performed in 9 patients (45 %) before scoliosis treatment. Mean sternal tilt angles were 11.5° preoperatively and 11.1° postoperatively. Mean Haller indices were 4.8 preoperatively and 5.3 postoperatively. This was especially true for syndromic or neuromuscular scoliosis and thoracolumbar/lumbar curve type patients in which scoliosis surgery tended to worsen the Haller index.
Conclusion
The Haller index increased postoperatively in 11 of 20 patients, which means sternal depression deteriorated after scoliosis surgery in about 50 % of patients. We suggest that surgeons fully assess the thoracic factors in patients with scoliosis and pectus excavatum prior to performing scoliosis surgery and carefully monitor their patient’s general condition during surgery.



Similar content being viewed by others
References
Waters P, Welch K, Micheli LJ, Shamberger R, Hall JE (1989) Scoliosis in children with pectus excavatum and pectus carinatum. J Pediatr Orthop 9:551–556
Hong JY, Suh SW, Park HJ, Kim YH, Park JH, Park SY (2011) Correlations of adolescent idiopathic scoliosis and pectus excavatum. J Pediatr Orthop 31(8):870–874
Wang Y, Chen G, Xie L, Tang J, Ben X, Zhang D, Xiao P, Zhou H, Zhou Z, Ye X (2012) Mechanical factors play an important role in pectus excavatum with thoracic scoliosis. J Cardiothorac Surg 7:118
Ha HI, Seo JB, Lee SH, Kang JW, Goo HW, Lim TH, Shin MJ (2007) Imaging of Marfan syndrome: multisystemic manifestations. Radiographics 27(4):989–1004
Lawson ML, Barnes-Eley M, Burke BL, Mitchell K, Katz ME, Dory CL, Miller SF, Nuss D, Croitoru DP, Goretsky MJ, Kelly RE Jr (2006) Reliability of a standardized protocol to calculate cross-sectional chest area and severity indices to evaluate pectus excavatum. J Pediatr Surg 41:1219–1225
Kuru P, Cakiroglu A, Er A, Ozbakir H, Cinel AE, Cangut B, Iris M, Canbaz B, Pıçak E, Yuksel M (2016) Pectus excavatum and pectus carinatum: associated conditions, family history, and postoperative patient satisfaction. Korean J Thorac Cardiovasc Surg 49(1):29–34
Brochhausen C, Turial S, Muller FK, Schmitt VH, Coerdt W, Wihlm JM, Schier F, Kirkpatrick CJ (2012) Pectus excavatum: history, hypotheses and treatment options. Interact Cardiovasc Thorac Surg 14(6):801–806
Haller JA, Kramer SS, Lietman SA (1987) Use of CT scans in selection of patients for pectus excavatum surgery: a preliminary report. J Pediatr Surg 22:904–906
Lowe TG, Edgar M, Margulies JY, Miller NH, Raso VJ, Reinker KA, Rivard CH (2000) Etiology of idiopathic scoliosis: current trends in research. J Bone Joint Surg Am 82-A(8):1157–1168
Wang WJ, Yeung HY, Chu WC, Tang NL, Lee KM, Qiu Y, Burwell RG, Cheng JC (2011) Top theories for the etiopathogenesis of adolescent idiopathic scoliosis. J Cardiothorac Surg Pediatr Orthop 31(1 Suppl):S14–S27
Takahashi Y, Kou I, Takahashi A, Johnson TA, Kono K, Kawakami N, Uno K, Ito M, Minami S, Yanagida H, Taneichi H, Tsuji T, Suzuki T, Sudo H, Kotani T, Watanabe K, Chiba K, Hosono N, Kamatani N, Tsunoda T, Toyama Y, Kubo M, Matsumoto M, Ikegawa S (2011) Scoliosis. Nat Genet 23; 43(12):1237–1240
Gurnett CA, Alaee F, Bowcock A, Kruse L, Lenke LG, Bridwell KH, Kuklo T, Luhmann SJ, Dobbs MB (2009) Genetic linkage localizes an adolescent idiopathic scoliosis and pectus excavatum gene to chromosome 18 q. Spine 15; 34(2):E94–E100
Alexianu D, Skolnick ET, Pinto AC, Ohkawa S, Roye DP Jr, Solowiejczyk DE, Hyman JE, Sun LS (2004) Severe hypotension in the prone position in a child with neurofibromatosis, scoliosis and pectus excavatum presenting for posterior spinal fusion. Anesth Analg 98:334–335
Bafus BT, Chiravuri D, van der Velde ME, Chu BI, Hirshl R, Farley FA (2008) Severe hypotension associated with the prone position in a child with scoliosis and pectus excavatum undergoing posterior spinal fusion. J Spinal Disord Tech 21:451–454
Galas JM, van der Velde ME, Chiravuri SD, Farley F, Parra D, Ensing GJ (2009) Echocardiographic diagnosis of right ventricular inflow compression associated with pectus excavatum during spinal fusion in prone position. Congenit Heart Dis 4:193–195
Harris JA, Mayer OH, Shah SA, Campbell RM Jr, Balasubramanian S (2014) A comprehensive review of thoracic deformity parameters in scoliosis. Eur Spine J 23(12):2594–2602
Chu ZG, Yu JQ, Yang ZG, Peng LQ, Bai HL, Li XM (2010) Correlation between sternal depression and cardiac rotation in pectus excavatum: evaluation with helical CT. AJR Am J Roentgenol 195:W76–W80
Acknowledgments
We sincerely express our appreciation to Ms. Hiraiwa for her contribution to this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
No funds were received in support of this work. No benefits in any form have been or will be received from commercial party related directly or indirectly to the subject of this manuscript.
We absolutely had approval of their information about their surgery from patients and/or their parents. We had signed documents about ethical approval and informed consent from them.
Conflict of interest
The authors have no financial conflicts of interest.
Additional information
This paper is designed and submitted acting on guideline of IRB of Meijo Hospital.
Rights and permissions
About this article
Cite this article
Tauchi, R., Kawakami, N., Tsuji, T. et al. Evaluation of thoracic factors after scoliosis surgery in patients with both scoliosis and pectus excavatum. Eur Spine J 27, 381–387 (2018). https://doi.org/10.1007/s00586-016-4753-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4753-4