Abstract
Purpose
Little is known about the long-term status of patients operated for spine deformities. The aim of this study was to determine the survival of primary fusion in adult idiopathic scoliosis and identify the risk factors of revision surgery.
Methods
Adult patients who underwent primary fusion for idiopathic scoliosis between 1983 and 2011 were included in a continuous monocentric retrospective series. Any additional surgery was registered for survival analysis. Survival and follow-up were estimated by the Kaplan–Meier method and an analysis was performed to identify the risk factors of revision surgery.
Results
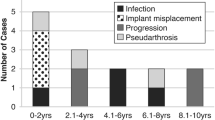
This series included 447 women (86.5 %) and 70 men (13.5 %) reviewed after a mean follow-up of 7 years (range 0–26.4). Mean age was 44.4 years. Fusion was performed on a median 11 levels (range 3–15); revision rate was 13 % (CI 10–17), 18 % (CI 14–23) and 20 % (CI 16–26) at 5, 10 and 15 years, respectively. Revision surgery was associated with age, anterior release, length of fusion, the inferior limit of fusion, post-operative sagittal balance and junctional kyphosis. The length of fusion (HR 1.13 per vertebrae fused, p = 0.007) and the lower limit of fusion (HR 5.9, p < 0.001) remained independent predictors of revision surgery on multivariate analysis.
Conclusion
This series evaluated the risk of revision surgery following spinal fusion for idiopathic scoliosis. Our results show that the risk seemed to increase linearly with a rate of nearly 20 % after 10 years. The length and lower limit of fusion are the main risk factors for revision surgery. Level IV (e.g. case series).



Similar content being viewed by others
References
Cho SK, Bridwell KH, Lenke LG, Cho W, Zebala LP, Pahys JM et al (2012) Comparative analysis of clinical outcome and complications in primary versus revision adult scoliosis surgery. Spine Mars 37(5):393–401
Carreon LY, Puno RM, Lenke LG, Richards BS, Sucato DJ, Emans JB et al (2007) Non-neurologic complications following surgery for adolescent idiopathic scoliosis. J Bone 89:2427–2432
Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR (2003) Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am 85(11):20892092
Bago J, Ramirez M, Pellise F, Villanueva C (2003) Survivorship analysis of Cotrel–Dubousset instrumentation in idiopathic scoliosis. Eur Spine J 12(4):435–439
Guigui P, Blamoutier A, Groupe d’Etude de la Scoliose (2005) Complications of surgical treatment of spinal deformities: a prospective multicentric study of 3311 patients. Rev Chir Orthopédique Réparatrice Appar Mot juin 91(4):314–327
Ramo BA, Richards BS (2012) Repeat surgical interventions following « definitive » instrumentation and fusion for idiopathic scoliosis: five-year update on a previously published cohort. Spine 37(14):1211–1217
Richards BS, Hasley BP, Casey VF (2006) Repeat surgical interventions following « definitive » instrumentation and fusion for idiopathic scoliosis. Spine 31(26):3018–3026
Mok JM, Cloyd JM, Bradford DS, Hu SS, Deviren V, Smith JA et al (2009) Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. [miscellaneous article]. Spine 34(8):832–839
Luhmann SJ, Lenke LG, Bridwell KH, Schootman M (2009) Revision surgery after primary spine fusion for idiopathic scoliosis. Spine 34(20):2191–2197
Asher MA, Lai SM, Burton DC (2010) Analysis of instrumentation/fusion survivorship without reoperation after primary posterior multiple anchor instrumentation and arthrodesis for idiopathic scoliosis. Spine J Janv 10(1):5–15
Campos M, Dolan L, Weinstein S (2012) Unanticipated revision surgery in adolescent idiopathic scoliosis. Spine 37(12):1048–1053
Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin DM, BULLET, Study Group on Scoliosis (2012) Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients [miscellaneous article]. Spine 37(8):693–700
Biau DJ, Hamadouche M (2011) Estimating implant survival in the presence of competing risks. Int Orthop 35(2):151–155
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP et al (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Sansur CA, Smith JS, Coe JD, Glassman SD, Berven SH, Polly DW et al (2011) Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine 36(9):E593–E597
Kuklo TR, Potter BK, Lenke LG, Polly DWJ, Sides B, Bridwell KH (2007) Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine 32(20):2258–2264
Pichelmann MA, Lenke LG, Bridwell KH, Good CR, O’Leary PT, Sides BA (2010) Revision rates following primary adult spinal deformity surgery: six hundred forty-three consecutive patients followed-up to twenty-two years postoperative. Spine 35(2):219–226
Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS (2002) Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine 27(7):776–786
Edwards CC 2nd, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG (2004) Long adult deformity fusions to L5 and the sacrum a matched cohort analysis. Spine 29(18):1996–2005
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Kim YW (2007) Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine 32(24):2653–2661
Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Lee TJ et al (2008) Short fusion versus long fusion for degenerative lumbar scoliosis. Eur Spine J 17(5):650–656
OʼShaughnessy BA, Bridwell KH, Lenke LG, Cho W, Baldus C, Chang MS et al (2012) Does a long-fusion « T3-sacrum » portend a worse outcome than a short-fusion « T10-sacrum » in primary surgery for adult scoliosis? Spine 37(10):884–890
Hartin NL, Mehbod AA, Joglekar SB, Transfeldt EE (2013) The fusion risk score: evaluating baseline risk in thoracic and lumbar fusion surgery. Spine 38(25):E1616–E1623
Pearcy M, Portek I, Shepherd J (1984) Three-dimensional x-ray analysis of normal movement in the lumbar spine. Spine 9(3):294–297
Dvorak J, Panjabi M, Chang D, Theiler R, Grob D (1991) Functional radiographic diagnosis of the lumbar spine flexion-extension and lateral bending. Spine 16(5):562–571
Edmondston SJ, Christensen MM, Keller S, Steigen LB, Barclay L (2012) Functional radiographic analysis of thoracic spine extension motion in asymptomatic men. J Manipulative Physiol Ther 35(3):203–208
Marks M, Newton PO, Petcharaporn M, Bastrom TP, Shah S, Betz R et al (2012) Postoperative segmental motion of the unfused spine distal to the fusion in 100 patients with adolescent idiopathic scoliosis. Spine 37(10):826–832
Lee MC, Ounpuu S, Solomito M, Smith BG, Thomson JD (2013) Loss in spinal motion from inclusion of a single mid-lumbar level in posterior spinal fusion for adolescent idiopathic scoliosis. Spine 10:118
Li G, Patil CG, Lad SP, Ho C, Tian W, Boakye M (2008) Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine 33(11):1250–1255
Patil CG, Santarelli J, Lad SP, Ho C, Tian W, Boakye M (2008) Inpatient complications, mortality, and discharge disposition after surgical correction of idiopathic scoliosis: a national perspective. Spine J Off J North Am Spine Soc 8(6):904–910
Lee MJ, Konodi MA, Cizik AM, Bransford RJ, Bellabarba C, Chapman J (2012) Risk Factors for Medical Complication after Spine Surgery: a multivariate analysis of 1591 patients. Spine J Mars 12(3):197–206
Bess S, Boachie-Adjei O, Burton D, Cunningham M, Shaffrey C, Shelokov A et al (2009) Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine 34(20):2186–2190
Glassman SD, Schwab FJ, Bridwell KH, Ondra SL, Berven S, Lenke LG (2007) The selection of operative versus nonoperative treatment in patients with adult scoliosis [Miscellaneous Article]. Spine 32(1):93–97
Helenius I, Remes V, Yrjönen T, Ylikoski M, Schlenzka D, Helenius M et al (2005) Does gender affect outcome of surgery in adolescent idiopathic scoliosis? Spine 30(4):462–467
Yagi M, King AB, Boachie-Adjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis minimum 5 years of follow-up. Spine 37(17):1479–1489
Sun Z, Qiu G, Zhao Y, Guo S, Wang Y, Zhang J et al (2015) Risk factors of proximal junctional angle increase after selective posterior thoracolumbar/lumbar fusion in patients with adolescent idiopathic scoliosis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc févr 24(2):290–297
Koller H, Pfanz C, Meier O, Hitzl W, Mayer M, Bullmann V, et al (2015) Factors influencing radiographic and clinical outcomes in adult scoliosis surgery: a study of 448 European patients. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 1–17
Lazennec JY, Ramaré S, Arafati N, Laudet CG, Gorin M, Roger B et al (2009) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc févr 9(1):47–55
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G (2006) Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine 31(20):2329–2336
Yagi M, King AB, BoachieAdjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis minimum 5 years of follow-up. Spine 37(17):147914–147989
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Riouallon, G., Bouyer, B. & Wolff, S. Risk of revision surgery for adult idiopathic scoliosis: a survival analysis of 517 cases over 25 years. Eur Spine J 25, 2527–2534 (2016). https://doi.org/10.1007/s00586-016-4505-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4505-5