Abstract
Purpose
The aim of this study was to evaluate the prevalence of depressive symptoms and disability pre-operatively, at 3 months and at 1 year after lumbar spine fusion surgery.
Methods
Data was extracted from a dedicated lumbar spine fusion register, giving 232 patients (mean age 62 years, 158 females) who had undergone instrumented lumbar spine fusion. The frequency of depressive symptoms and disability was evaluated using the Depression Scale (DEPS) and Oswestry Disability Index (ODI).
Results
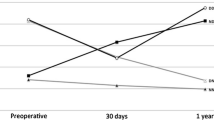
Depressive symptoms were found in 34, 13, and 15 % of the patients pre-operatively, at 3 months and at 1 year after surgery, respectively. The mean DEPS score decreased from 16.2 to 8.6 (p < 0.001) in patients who had depressive symptoms pre-operatively, and from 6.1 to 3.8 (p < 0.001) in those patients without pre-operative depressive symptoms. The mean ODI values pre-operatively, at 3 months and at 1 year after surgery were 53, 30, and 23, respectively, in patients with pre-operative depressive symptoms and 41, 23, and 20 in those patients without pre-operative depressive symptoms. The differences between the groups were statistically significant at all time points (p < 0.001).
Conclusions
One-third of our patients with chronic back pain undergoing spinal fusion had depressive symptoms pre-operatively. The prevalence of depressive symptoms decreased after surgery. Although disability remained higher in those patients who had reported depressive symptoms pre-operatively, disability did decrease significantly in both groups post-operatively. Thus, there is no need to exclude depressive patients from operation, but screening measures and appropriate treatment practises throughout both pre-operative and post-operative periods are encouraged.


Similar content being viewed by others
References
Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Dvorak J, Jacobshagen N, Semmer NK, Boos N (2007) Predictors of multidimensional outcome after spinal surgery. Eur Spine J 16(6):777–786
Reme SE, Tangen T, Moe T, Eriksen HR (2011) Prevalence of psychiatric disorders in sick listed chronic low back pain patients. Eur J Pain 15(10):1075–1080
Hägg O, Fritzell P, Ekselius L, Nordwall A, Swedish Lumbar Spine Study (2003) Predictors of outcome in fusion surgery for chronic low back pain. A report from the Swedish Lumbar Spine Study. Eur Spine J 12(1):22–33
Magni G (1984) Chronic low-back pain and depression: an epidemiological survey. Acta Psychiatr Scand 70(6):614–617
Polatin PB, Kinney RK, Gatchel RJ, Lillo E, Mayer TG (1993) Psychiatric illness and chronic low-back pain. The mind and the spine—which goes first? Spine (Phila Pa 1976) 18(1):66–71
Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, Blood EA, Birkmeyer NJ, Hilibrand AS, Herkowitz H, Cammisa FP, Albert TJ, Emery SE, Lenke LG, Abdu WA, Longley M, Errico TJ, Hu SS (2007) Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 356(22):2257–2270
Mirza SK, Deyo RA (2007) Systematic review of randomized trials comparing lumbar fusion surgery to non-operative care for treatment of chronic back pain. Spine (Phila Pa 1976) 32(7):816–823
Sinikallio S, Aalto T, Airaksinen O, Lehto SM, Kröger H, Viinamäki H (2011) Depression is associated with a poorer outcome of lumbar spinal stenosis surgery: a two-year prospective follow-up study. Spine (Phila Pa 1976) 36(8):677–682
LaCaille RA, DeBerard MS, Masters KS, Colledge AL, Bacon W (2005) Presurgical biopsychosocial factors predict multidimensional patient: outcomes of interbody cage lumbar fusion. Spine J 5(1):71–78
Katz JN, Stucki G, Lipson SJ, Fossel AH, Grobler LJ, Weinstein JN (1999) Predictors of surgical outcome in degenerative lumbar spinal stenosis. Spine (Phila Pa 1976) 24(21):2229–2233
Poutanen O, Koivisto AM, Salokangas RK (2008) The Depression Scale (DEPS) as a case finder for depression in various subgroups of primary care patients. Eur Psychiatry 23(8):580–586 Epub Sep 7
Salokangas RK, Poutanen O, Stengård E (1995) Screening for depression in primary care. Development and validation of the Depression Scale, a screening instrument for depression. Acta Psychiatr Scand 92(1):10–16
Poutanen O, Koivisto AM, Kääriä S, Salokangas RK (2010) The validity of the Depression Scale (DEPS) to assess the severity of depression in primary care patients. Fam Pract 27(5):527–534
Pekkanen L, Kautiainen H, Ylinen J, Salo P, Häkkinen A (2011) Reliability and validity study of the Finnish version 2.0 of the Oswestry Disability Index. Spine (Phila Pa 1976) 36(4):332–338
Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25(22):2940–2952 (discussion 2952)
Price DD, McGrath PA, Rafii A, Buckingham B (1983) The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 17(1):45–56
Trief PM, Ploutz-Snyder R, Fredrickson BE (2006) Emotional health predicts pain and function after fusion: a prospective multicenter study. Spine (Phila Pa 1976) 31(7):823–830
Okoro T, Sell P (2009) The prediction of outcome in somatised patients undergoing elective lumbar surgery. J Bone Joint Surg Br 91(4):517–521
Carreon LY, Glassman SD, Djurasovic M, Dimar JR, Johnson JR, Puno RM, Campbell MJ (2009) Are preoperative health-related quality of life scores predictive of clinical outcomes after lumbar fusion? Spine (Phila Pa 1976) 34(7):725–730
Ayuso-Mateos JL, Vázquez-Barquero JL, Dowrick C, Lehtinen V, Dalgard OS, Casey P, Wilkinson C, Lasa L, Page H, Dunn G, Wilkinson G, ODIN Group (2001) Depressive disorders in Europe: prevalence figures from the ODIN study. Br J Psychiatry 179:308–316
Vanhala M, Jokelainen J, Keinänen-Kiukaanniemi S, Kumpusalo E, Koponen H (2009) Depressive symptoms predispose females to metabolic syndrome: a 7-year follow-up study. Acta Psychiatr Scand 119(2):137–142
Salokangas RK, Vaahtera K, Pacriev S, Sohlman B, Lehtinen V (2002) Gender differences in depressive symptoms. An artefact caused by measurement instruments? J Affect Disord 68(2–3):215–220
Enthoven P, Skargren E, Carstensen J, Oberg B (2006) Predictive factors for 1-year and 5-year outcome for disability in a working population of patients with low back pain treated in primary care. Pain 122(1–2):137–144
Andersen T, Videbaek TS, Hansen ES, Bünger C, Christensen FB (2008) The positive effect of posterolateral lumbar spinal fusion is preserved at long-term follow-up: a RCT with 11–13 year follow-up. Eur Spine J 17(2):272–280
Hägg O, Fritzel P, Nordwall A (2003) The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J 12(1):12–20
Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J 8(6):968–974
Hägg O, Fritzell P, Nordwall A, The Swedish Lumbar Spine Study Group (2002) Characteristics of patients with chronic low back pain selected for surgery: a comparison with the general population reported from the Swedish lumbar spine study. Spine (Phila Pa 1976) 27(11):1223–1231
Acknowledgments
The authors thank Tampere University Hospital and Jyväskylä Central Hospital spine register teams, especially Liisa Pekkanen, Kati Kyrölä, Kirsi Piitulainen and Seija Rautiainen for collecting the register data. We also thank Virginia Mattila and Honorary Professor Associate Ian McDermott for editing English language of this manuscript. The study was supported by Medical Research Funds from Tampere University Hospital and Jyväskylä Central Hospital, Finland.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wahlman, M., Häkkinen, A., Dekker, J. et al. The prevalence of depressive symptoms before and after surgery and its association with disability in patients undergoing lumbar spinal fusion. Eur Spine J 23, 129–134 (2014). https://doi.org/10.1007/s00586-013-2896-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2896-0